Rachna Mehta PT, DPT, CIMT, OCS, PRPC, RYT 200 is Board certified in Orthopedics, a Certified Integrated Manual Therapist, and a Herman & Wallace certified Pelvic Rehab Practitioner. Rachna has a personal interest in various eastern holistic healing traditions and she noticed that many of her chronic pain patients were using complementary health care approaches including acupuncture and yoga. Her course Acupressure for Optimal Pelvic Health brings a unique evidence-based approach and explores complementary medicine as a powerful tool for holistic management of the individual as a whole focusing on the physical, emotional, and energy body.
A patient walks into the clinic 30 minutes late for their appointment with me, brimming with anxiety and apologizing profusely. “I’m so sorry,” they say, “I kept driving around in circles and could not find a single parking spot.” Another patient, a teacher, reports that her anxiety and pelvic pain progressively worsens as her day progresses and peaks when she gets home with her own two young children at the end of a long day. A third patient with a 15-year history of pelvic pain with unexplained infertility who has failed every conventional ART treatment suddenly conceives her miracle child naturally with acupuncture. She shares, “My anxiety was always so high, I could never relax. They stimulated acupuncture points all over my body, and it worked. My anxiety was so much under control this time.”
Here are the things running through my mind as I work with these patients:
- What could be the most effective hands-on clinical intervention I could use to calm them down?
- Could I teach them daily acupressure self-care and wellness regimens to alleviate anxiety?
- Could I foster a feeling of self-control in them to manage anxiety in stressful situations?
- How does acupuncture really work for infertility, and why does it use points all over the body?
- Can acupressure be used to stimulate key potent acupoints for anxiety?
- Is there a physical practice of yoga that is calm and meditative and is complementary to acupressure?
These questions led to researching the currently available evidence, and I found that there has been a rising clinical interest in complementary holistic practices over the last several decades for anxiety & chronic stress management. Current research supports both acupressure and yin yoga as powerful tools in the realm of energy medicine.
Acupressure is based on 3000 years of Traditional Chinese Medicine (TCM) that believes in Meridian Theory and energy channels which are connected to the function of the visceral organs. There is emerging scientific evidence of acupoints transmitting Qi energy through the vast network of interstitial connective tissue connecting the peripheral nervous system to the central viscera with potentially powerful integrative applications across multiple systems. This network is also continuous with more specialized connective tissues such as the periosteum, perimysium, perineurium, pleura, peritoneum, and meninges (1). Fascia and connective tissue literally pervade every anatomic dimension in the body.
Helene Langevin (2) and colleagues proposed an anatomical/ physiological parallel to explain some of the key concepts of TCM.
- Qi: Sum of all body energetic phenomena (e.g. metabolism, movement, signaling, information exchange)
- Meridian Qi: Connective tissue biochemical/bioelectrical signaling
- Blockage of Qi: Changed connective tissue matrix composition leading to a change in signal transduction
- Restoration of the flow of Qi: Cellular activation/gene expression leading to restored connective tissue matrix composition and signal transduction
Modern acupressure charts map the principal 12 meridians connected to the physiological functions of key organs. The key meridians to focus on in pelvic health patients would be the bladder, kidney, spleen, and stomach meridians. Acupressure is systemically effective for a host of conditions including anxiety, insomnia, chronic pelvic pain, dysmenorrhea, infertility, constipation, digestive disturbances, and urinary dysfunctions. Each acupressure point has many internal connections to the visceral organs. Stimulating these points by using acupressure assists the body’s self-regulating mechanisms and facilitate healing and neurophysiological quieting.
A recent study by Elizabeth Monson (3) and colleagues retrospectively analyzed 519 acupressure treatments on hospitalized patients, nurses, and the general public across six US states. They followed a specific acupressure protocol and looked at pre- and post-treatment in conjunction with self-rated pain and anxiety scores, where 0 represented no pain or anxiety, and 10 represented the worst pain and anxiety. They found that:
- Hospitalized patients demonstrated a 4 point ↓ in pain scores and 5 point ↓ in anxiety scores
- Nurses demonstrated a 3 point ↓ in pain scores and 4 point ↓ in anxiety scores
This study concluded that acupressure is a highly satisfactory complementary therapy that can demonstrate a clinically significant decrease in self-rated pain and anxiety scores (2).
A robust body of research also attests to yoga being a powerful integrative health practice for alleviating daily anxiety and stress. Yoga is an umbrella term for various physical, mental, and spiritual practices originating in ancient India. Hath Yoga is the most popular form of Yoga in western society. Yin Yoga, a derivative of Hath Yoga, is a much calmer meditative practice that uses seated and supine postures, held three to five minutes while maintaining deep breathing. Its focus on calmness and mindfulness makes Yin Yoga a tool for relaxation and stress coping, thereby improving psychological health (4).
Yin Yoga is also a wonderful complimentary practice that can be combined with Acupressure. Yin Yoga engages the physical, emotional, and energy body. Yin postures supportively align the body to stress connective tissues along specific meridian lines that activate potent acupressure points along those meridians. The Acupressure for Optimal Pelvic Health remote course explores Yin postures within key meridians and integrates acupressure and Yin Yoga with modifications into rehabilitation interventions. Anxiety and daily wellness self-care program is also a key part of the course.
As pelvic health therapists and medical providers, we can empower our patients to recognize the mind-body-energy interconnections and how they affect multiple systems, giving them the tools and self-care regimens to live healthier anxiety and pain-free lives. Combining our orthopedic skills with mindfulness-based holistic interventions also complements our best evidence-based practices.
The course Acupressure for Optimal Pelvic Health is an evidence-based journey of holistic healing and empowerment curated and taught by Rachna Mehta. To learn how to integrate acupressure and Yin Yoga into your practice, join the next scheduled remote course on October 23-24, 2021.
- Kaptchuk TJ. 2000. The web that has no weaver. Understanding Chinese medicine. Chicago: Contemporary Publishing Group, Inc.2.
- Langevin HM, Yandow JA. Relationship of acupuncture points and meridians to connective tissue planes. Anat Rec. 2002;269(6):257-265. doi:10.1002/ar.10185
- Monson E, Arney D, Benham B, et al. Beyond Pills: Acupressure Impact on Self-Rated Pain and Anxiety Scores. J Altern Complement Med. 2019;25(5):517-521. doi:10.1089/acm.2018.0422
- Daukantaitė D, Tellhed U, Maddux RE, Svensson T, Melander O. Five-week Yin Yoga-based interventions decreased plasma adrenomedullin and increased psychological health in stressed adults: A randomized controlled trial. PLoS One. 2018;13(7)
- Hmwe NTT, Browne G, Mollart L, Allanson V, Chan SW. An Integrative review of Acupressure interventions for older people: A focus on sleep quality, depression, anxiety, and agitation. Int J Geriatr Psychiatry. 2019;34(3):381-396. doi:10.1002/gps.5031
- Au DW, Tsang HW, Ling PP, Leung CH, Ip PK, Cheung WM. Effects of Acupressure on Anxiety: A Systematic review and meta-analysis. Acupunct Med. 2015;33(5):353-359. doi:10.1136/acupmed-2014-010720
Molly O'Brien-Horn, PT, DPT, CLT is a pelvic health physical therapist in California. She is a teaching assistant with Herman & Wallace and will be acting as a TA in the upcoming remote course, Inclusive Care for Gender and Sexual Minorities. Molly is a Certified Lymphedema Therapist (CLT), an LSVT BIG Parkinson’s Disease certified therapist, a trained childbirth doula, and a trained postpartum doula. She is a member of the American Physical Therapy Association Section of Pelvic Health. She has experience in a variety of physical therapy settings, including pediatric oncology, school-based pediatrics, outpatient orthopedics, and wound care. Her passion, however, is working in the field of pelvic floor physical therapy with children, teens, and adults of all gender identities, all sexualities, and all ability levels. In her spare time, Molly enjoys doing yoga, hiking, and relaxing at the beach.
October is LGBT History Month. This annual occurrence is a month-long observance of lesbian, gay, bisexual, and transgender history, and the history of the gay rights and related civil rights movements. H&W is proud to offer courses for treating the whole patient across the gender and age spectrum. The remote courses featured in this blog are Inclusive Care for Gender and Sexual Minorities with instructor Brianna Durand, and Transgender Patients: Pelvic Health and Orthopedic Considerations with co-instructors Sandra Gallagher and Caitlin Smigelski.

Many LGBTQ+ individuals, drag artists, and cisgender and heterosexual persons engage in binding, tucking, packing, and padding for several reasons. These techniques can be life-changing. Many people use these techniques for gender expression, but they can also be used for gender affirmation.
Gender dysphoria occurs when an individual feels distress due to a mismatch between their assigned gender at birth and their own gender identity. For many folx who are transgender, non-binary, queer, or intersex, these practices help reduce gender dysphoria. Instead, they provide feelings of gender euphoria by creating joy, enhancing mental well-being, and improving quality of life through affirming gender identity. Additionally, these methods can provide safety by helping to protect folx in unsafe and unfamiliar environments. Some of these devices, such as packers, can even be used for sexual function and urination
So how does it all work? Binding is when a person wears a device, called a binder, to flatten or minimize the appearance of their chest. Many folx who identify as transmasculine and non-binary engage in binding. However, not all people who bind identify as transmasculine or non-binary. For example, cis and queer women, and cisgender men with gynecomastia may use binders. Also of note, not all people who bind use the same binding methods. Compression shirts and tops, sports bras, and tape are a few examples of the many different binding methods available.
Conversely, padding can be used to enhance the shape and appearance of one’s body, often at the hips and gluteal regions. Padded bras can also be used to enhance breast size and shape. Many transfeminine, queer, intersex, non-binary, and cisgender women often use some form of padding or shapewear devices to help create a more effeminate silhouette. Drag artists often use some form of padding to modify their appearance for their performances to achieve the optimal look for their drag persona. Transmen and cismen can also use padding. Furthermore, wigs and prosthetics (e.g. silicone breast forms, breastplates, and prosthetic vaginas) can be used by these populations to achieve a desired appearance.
Regarding prosthetics, many transmasculine folx, cisgender men, intersex folx, and queer individuals use prosthetics for packing. When someone packs, they use a phallic-shaped device to enhance the prominence of their genitals, often to create the appearance of a bulge in their pants. Some packers can extend the length of a phallus for sexual play, as well. This can be helpful for transmasculine folx post metoidioplasty, intersex folx who may have anatomical differences in sexual or reproductive anatomy, as well as cisgender men who suffer from erectile dysfunction. Packers are often made of silicone and can also include or not include certain features like pubic hair, moveable foreskin, and testes. However, packers don’t have to be made of silicone and can instead be made from other items, such as a pair of socks. They can have multiple functions and be used for things other than packing, such as standing for urination, sexual pleasure for oneself, and sexual pleasure for partners.
While packing increases the prominence of one’s genitals, tucking, conversely, is used to minimize the prominence of external genitalia by creating a flatter appearance between the legs. This act gets its name from the tucking of one's testicles into the inguinal canals, after which the penis and scrotum are then tucked between the legs back towards the anus. Frequently gaffs, tape, or tucking underwear are used to maintain the genitalia in these positions. Tucking is commonly used by transfeminine, non-binary, and intersex persons. However, tucking is not just limited to these groups, as cismen, drag artists, and other populations can tuck also.
While binding, packing, tucking, and padding have many positives, there can be some inherent drawbacks. For example, tucking can increase the risk of Urinary Tract Infections due to the position of the urethra close to the anus. Binding can alter posture and impact breathing by reducing diaphragmatic and rib mobility. Pads can be uncomfortable and hot, while packing devices, Stand-to-Pee devices, in particular, require regular cleaning to prevent unwanted smells and/or infections. All of these practices carry the risk of skin breakdown or irritation if performed too frequently or with improper technique. However, it is important to remember that even with these and other various drawbacks, these acts can be so lifesaving, gender-affirming, and life-protecting for many folx, that at times, the benefits of performing these practices greatly outweigh the risks.
The ins and outs of binding, packing, tucking, and padding can be quite complex, and there is so much to learn about proper usage and technique.
Want to learn more about these and other things related to LGBTQ+ health? Check out these remote course options:
- Inclusive Care for Gender and Sexual Minorities, Brianna Durand and her TA Molly O'Brien-Horn will dive deeper into these and other topics surrounding LGBTQ+ healthcare to educate pelvic health practitioners on how to provide better, safer, and more skilled care for the LGBTQ+ populations.
- Transgender Patients: Pelvic Health and Orthopedic Considerations, co-instructors Sandra Gallagher and Caitlin Smigelski will expand your skills for working with people of all gender identities. This course includes particular education regarding gender-affirming genital surgeries as well as discussion of other gender-affirming surgeries and medical interventions that people transitioning might choose.
What are you waiting for? Sign up and join us today!

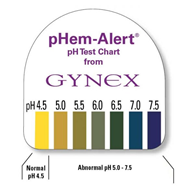
Many years ago a urology doctor shared the skill of testing vaginal pH as part of my pelvic floor exam. I’ve since used it to gather objective data around estrogen status, often finding elevated levels in post-partum, breastfeeding, and peri and post-menopausal women. When correlated with symptoms and visual skin changes this can be a helpful tool to both direct treatment and monitor treatment effectiveness.
To perform pH testing, place a pH strip into the distal vagina. Let it sit there for a few seconds to absorb vaginal moisture. Remove and record results. Any concerning changes in vaginal pH can be documented and reported back to your patient’s medical provider.
Here’s a quick tour through the research on vaginal pH. I hope you enjoy learning and consider adding vaginal pH testing to your clinical practice.
-Normal vaginal pH is considered to range between 4.0 and 5.0 in menstruating women (Garcia-Closas)
-Intervaginal pH does not vary between vaginal location (proximal, mid, distal)
-Clinician test vs self-test results vary slightly but not significantly (Ferris)
-Low serum estradiol levels are associated with high vaginal pH values
-Vaginal pH of 4.5 is indicative of premenopausal estradiol levels and the absence of bacterial overgrowth
-Vaginal pH of 5.0 to 6.5 may indicate either estrogen changes or bacterial overgrowth, a culture may be warranted
-Vaginal pH of 6.0 to 7.5 is strongly suggestive of menopause
-Vaginal pH measurements can be helpful in determining the efficacy of treatment with vaginal estrogen (Caillouette)
-Vaginal pH levels (high) were as sensitive as blood serum FSH levels in the detection of menopause status (Roy) and (Panda)
-Understanding of the vaginal microbiome and its effect on vaginal pH continues to evolve
-“Although lactic acid (produced by Lactobacillus) is the primary acid in normal vaginal secretions, other organic acids such as acetic, mydriatic, and linoleic acid are also normally found in vaginal fluid. Some healthy women actually lack vaginal Lactobacilli, but their vaginal pH is in the normal (moderately acidic) range, and other lactic acid-producing bacteria, such as Atopobium, Megasphaera, and/or Leptotrichia species, are present.”
-Lactic acid is also a byproduct of anaerobic glucose metabolism within the cells of the vaginal mucosa
-The summation of vaginal pH is determined by both the vaginal mucosal metabolism (which is influenced by estrogen) and the vaginal microbiome, both of which are unique to each female
-Vaginal pH is around 5 in newborns, before colonization from microbes, rises to neutral range by 6 weeks of life, and falls when puberty ushers in an increase in estrogen
-Normal vaginal pH helps to keep optimal inflammatory responses and skin barrier functions in vaginal and vulvar skin. Elevated pH in menopause leads to susceptibility to vulvar contact dermatitis
-Topical application to the menopausal vagina restores surface pH and lowers infection risk
-Candida infections do not alter vaginal pH
-STI via chlamydia, gonorrhea, or trichomonas as well as bacterial vaginosis may cause elevations in vaginal pH (Linhares)
- “Detection of HPV was positively associated with vaginal pH, mainly in women < 35 years. Elevated vaginal pH was associated with 30% greater risk of infection with multiple HPV types and with LSIL (low-grade intraepithelial lesions), predominantly in women younger than 35 and 65+ years of age. Detection of C. trachomatis DNA was associated with increased vaginal pH in women < 25 years” (Clarke)
-pH self-testing during pregnancy and treatment of underlying infections positively impacted preterm birth rates (Holyoke and Saling)
-The microbiome in humans is generally >70% Lactobacilli, where other mammals have 1% or less
-Average pH of 21 non-human mammals is 5.4 to 7.8
-Authors propose that the high level of starch in human diets contributes to increased levels of vaginal glycogen which in turn proliferates lactobacilli…continued research will contribute to our collective knowledge base (Miller)
-Vaginal microbiome variability may have an effect on fertility (Xu)
-Douching with an over-the-counter lactic acid containing douche: did not significantly affect vaginal pH or microbiome composition and may promote candida infections (van der Veer)
|
Solution |
pH |
|
Gastric acid |
1.5-2.0 |
|
Vinegar |
2.9 |
|
Orange juice |
3.5 |
|
Beer |
4.5 |
|
4.5 |
|
|
Skin surface moisture |
4.0-5.5 |
|
Milk |
6.5 |
|
Pure water |
7.0 |
|
Saliva |
6.5-7.4 |
|
Semen |
7.2-8.0 |
|
Blood |
7.3-7.5 |
|
Seawater |
7.7-8.3 |
|
Sodium bicarbonate |
8.4 |
|
Hand soap solution |
9.0-10.0 |
|
Bleach |
12.5 |
Linhares. Vaginal pH and Lactobacilli. Am J Obstet Gynecol 2011.
References:
Caillouette, J. C., Sharp Jr, C. F., Zimmerman, G. J., & Roy, S. (1997). Vaginal pH as a marker for bacterial pathogens and menopausal status. American journal of obstetrics and gynecology, 176(6), 1270-1277.
Clarke, M. A., Rodriguez, A. C., Gage, J. C., Herrero, R., Hildesheim, A., Wacholder, S., ... & Schiffman, M. (2012). A large, population-based study of age-related associations between vaginal pH and human papillomavirus infection. BMC infectious diseases, 12(1), 1-9.
Ferris, D. G., Francis, S. L., Dickman, E. D., Miler-Miles, K., Waller, J. L., & McClendon, N. (2006). Variability of vaginal pH determination by patients and clinicians. The Journal of the American Board of Family Medicine, 19(4), 368-373.
García-Closas, M., Herrero, R., Bratti, C., Hildesheim, A., Sherman, M. E., Morera, L. A., & Schiffman, M. (1999). Epidemiologic determinants of vaginal pH. American journal of obstetrics and gynecology, 180(5), 1060-1066.
Hoyme, U. B., & Saling, E. (2004). Efficient prematurity prevention is possible by pH-self measurement and immediate therapy of threatening ascending infection.
Linhares, I. M., Summers, P. R., Larsen, B., Giraldo, P. C., & Witkin, S. S. (2011). Contemporary perspectives on vaginal pH and lactobacilli. American journal of obstetrics and gynecology, 204(2), 120-e1.
Miller, E. A., Beasley, D. E., Dunn, R. R., & Archie, E. A. (2016). Lactobacilli dominance and vaginal pH: Why is the human vaginal microbiome unique?. Frontiers in microbiology, 7, 1936.
Panda, S., Das, A., Santa Singh, A., & Pala, S. (2014). Vaginal pH: A marker for menopause. Journal of mid-life health, 5(1), 34.
Roy, S., Caillouette, J. C., Roy, T., & Faden, J. S. (2004). Vaginal pH is similar to follicle-stimulating hormone for menopause diagnosis. American journal of obstetrics and gynecology, 190(5), 1272-1277.
Xu, J., Bian, G., Zheng, M., Lu, G., Chan, W. Y., Li, W., ... & Du, Y. (2020). Fertility factors affect the vaginal microbiome in women of reproductive age. American Journal of Reproductive Immunology, 83(4), e13220.
Van Der Veer, C., Bruisten, S. M., Van Houdt, R., Matser, A. A., Tachedjian, G., van de Wijgert, J. H. H. M., ... & van der Helm, J. J. (2019). Effects of an over-the-counter lactic-acid containing intra-vaginal douching product on the vaginal microbiota. BMC microbiology, 19(1), 1-13.
*Citations are noted at the end of each article summary
This product was recommended by S. Roy for accurate testing:
It’s OK to be feeling (insert feeling) right now. (maybe: sad, fearful, angry, denial, numb, anxious, avoidant, bored?)
 It’s OK to acknowledge those feelings.
It’s OK to acknowledge those feelings.
It’s also OK to create a plan and direction about what we may do about our feelings, thoughts, and actions.
We can change how we think, what we do and ultimately how we feel.
Breathe. Place a hand on your chest and a hand on your abdomen. Practice inhaling long and deep as if you were pouring the air into your body- first filling the lower hand and then filling the top hand. Pause for a moment when you feel your canister is full and then exhale slowly (top to bottom or bottom to top- either works fine). I prefer breathing through my nose for inhale and exhale but know if you are congested, mouth breathing is fine or you can inhale through the nose and exhale through the mouth- find what works for you. Work on increasing the number counted (silently in your mind) while you inhale, pause briefly and then exhale- making that number count on exhale the same or even longer. Make it a game to see how long and deep your breath can become. Reduce intensity if feeling lightheaded.
Focus on your breath and feel calmness. Return to this breathing whenever you can.
Body Scan/Progressive Relaxation. Take a moment and scan your body for pain or tension. You can start at the top of your body or where your feet are grounded to floor. Notice your body and allow it to be, without judgement. Then starting from the top of your body or the bottom, contract your muscles systematically and then relax. Or focus on the muscle group and allow the muscles to relax and slacken. Maybe send your long, deep breath to each area? Maybe think of color washing each area? Make your scan personal and positive for you. Check-in to your body without judgement and send gratefulness for the work your amazing body does.
Stand Big. Find a wall and place your backside onto it. Pretend there is a string at the crown of your head and imagine your head being pulled up towards the ceiling. Lift your chest as you are standing tall and use your slow, steady, deep breathing to create bigness and calmness. Relax your shoulders. Maybe place the back of your hands onto wall and feel the opening of your chest. Once you have practiced this posture, you can refer to this posture during your day. Stand big, breathe big, be big.
Intentionally SCHEDULE into your life what you love. Schedule time listening to your favorite music. Maybe take up playing an instrument? Practice singing in the shower or car. Set a timer and dance fervently. Create time to draw or paint or write. Make a recipe. Get frozen berries and make smoothies. Maybe add frozen spinach to your smoothie?
Pick up a book. Play a game, cards or even solitaire. Practice Sudoku. Take a bath or shower. Go for a long walk while keeping your distance from others. Find a workout you can do at home that makes you feel powerful. Whatever you love, turn it into a scheduled ritual. Make one small goal and work towards it. Focus on what we can do instead of what we cannot. Find some activity and fulfill a passion just for you. Make sleep a priority and know if you have a bad night, that the next night you will likely sleep better. Perhaps create a sleeping ritual? Call others and ask what they are doing for themselves? Remember to forgive yourself and to feel or express the feelings that are within you. We are all going through this together. Make you a priority and schedule yourself some HAPPY.
Lastly- try to limit the news, your phone and the frig. All of these can create negative feelings that do not fulfill us.
Breathe. Find love in positive activities. Be brave. Be grateful. Forgive.
We are all in this together.
Lauren Mansell DPT, CLT, PRPC is the author and instructor of the Trauma Awareness for the Pelvic Therapist course. She is also offering several courses via Zoom video conference during the Covid-19 pandemic, which can be found on our Remote Learning Opportunities page. Prior to becoming a physical therapist, Lauren counseled suicidal and homicidal SES at-risk youth who had survived sexual violence. Lauren was certified as a medical and legal advocate for sexual assault survivors in 1999 and has advocated for over 130 sexual assault survivors of all ages in the ED. Lauren's physical therapy specialty certifications include Certified Lymphedema Therapist (CLT), Pelvic Rehabilitation Professional Certificate (PRPC) and Certified Yoga Therapist (CYT). She is a board member of Chicagoland Pelvic Floor Research Consortium, American Physical Therapy Association Section of Women's Health and Section of Oncology.
A Weekend of Transformation
Let me start this plog (picture/blog?) by saying it had been almost 2 years since Nari Clemons and I taught Boundaries, Self Care, and Meditation for the first time. Nari had some amazing ideas to change some of the course material to reflect more of our hearts’ intention for personal reflection and transformative change. We were excited and nervous to see how our second run of this material would be received. We were also profoundly aware of how the (at times painful) events in our lives that led up to the development of the course have molded and shaped us into much healthier versions of ourselves. We wanted to share a bit about what we have learned and how it has changed us.
We met up in beautiful San Diego on Thursday. Because this course was Saturday to Mononday we had an added bonus of extra time to spend together. We decided to spend our time practicing what we talk about in class.
1. Get out in nature:
Tory Pines State Park provided much needed rejuvination. Ahh sea air.
2. Self-care is mandatory:
We spent Friday relaxing at a beautiful resort in Del Mar. We are learning we don’t need to justify or feel bad about caring for ourselves. It’s necessary and important. We are responsible for meeting our own needs and for refueling ourselves when we provide care for others.
3. Get out of your comfort zone:
The robes we got from the resort were super cozy and it was chilly on the beach, so why not walk the beach in a robe? We laughed at ourselves and others laughed at us and with us. But we were comfy and warm.
4. Do the work when it is time to do the work:
Instead of thinking and talking about the course all day we committed ourselves to being in the moment. When it came time to discuss the details of the next three days, a plan came together with relative ease. This is us working at the resort.
5. Challenges can change your perspective. And a change in perspective can help you with challenges:
This is a (terrible, sorry) picture of us interrupting our morning run to climb a tree. It was a fun challenge and gave us an interesting perspective on our day.
A little more about the course. Woah. The people who showed up came with open minds and hearts, ready and ripe for change. We had powerful times of sharing, listening, learning, and supporting. Meditation and yoga and a healing, honest and real atmosphere brought about transformation in the most beautiful awe-inspiring way. We were profoundly moved. The changes Nari suggested were PERFECT and I was grateful for her innovations. We were all pretty much out of our comfort zones, but that is where change happens.
In the words of one student, “This course couldn’t have come at a more appropriate time because I was in major burnout. I was becoming an unhappy person both professionally and personally. I needed to make a change. Now I am leaving this course empowered to care for myself so I can help patients in a healthy way and enjoy my job again. I am walking away from this course with so many valuable strategies and also feel so much more relaxed and hopeful”
6. Be silly sometimes:
Laugh a lot. Especially at work. Play jokes, have fun. You know what they say about all work and no play. Play.
7. At the end of the day Shake it off (and use pain science as needed):
Our last day we took a run to the beach. When crossing a rail line I tripped and bashed the HECK out of my lower leg. Since I could still run I repeated the mantra “Hurt not harm!!” (which we discuss in class) with great vigor until the throbbing subsided, and we enjoyed a beautiful sunset and the conclusion of our time in San Diego.
Last words of Wisdom:
Gratitude can change us in powerful ways.
A huge and heart felt thank you to Herman & Wallace, our host site, and for each and every participant. We couldn’t do what we do without you and for this we are eternally grateful.
Thank you. Thank you. Thank you.

In a previous post on The Pelvic Rehab Report, Sagira Vora, PT, MPT, WCS, PRPC explored the impact that pelvic floor exercises can have on arousal and orgasm in women. Today we hear part two of the conversation, and learn what factors can impact a woman's ability to achieve orgasm.
 “An orgasm in the human female is a variable, transient peak sensation of intense pleasure, creating an altered state of consciousness, usually with an initiation accompanied by involuntary, rhythmic contractions of the pelvic striated circumvaginal musculature, often with concomitant uterine and anal contractions, and myotonia that resolves the sexually induced vasocongestion and myotonia, generally with an induction of well-being and contentment.”
“An orgasm in the human female is a variable, transient peak sensation of intense pleasure, creating an altered state of consciousness, usually with an initiation accompanied by involuntary, rhythmic contractions of the pelvic striated circumvaginal musculature, often with concomitant uterine and anal contractions, and myotonia that resolves the sexually induced vasocongestion and myotonia, generally with an induction of well-being and contentment.”
Wow, that sounds like paradise! The question is--how to get there? Many of our cohorts and many our female patients have not experienced this or orgasm happens for them rarely. Findings from surveys and clinical reports suggest that orgasm problems are the second most frequently reported sexual problems in women. Some of the reasons cited for lack of orgasm are orgasm importance, sexual desire, sexual self-esteem, and openness of sexual communication with partner by Kontula el. al. in 2016. Rowland found that most commonly-endorsed reasons were stress/anxiety, insufficient arousal, and lack of time during sex, body image, pain, inadequate lubrication.
One factor that comes up consistently, is the ability of women to focus on sexual stimuli. This point has been brought up by various studies and presented in different ways. Chambless talks about mindfulness training and improvements in orgasm ability noted equally in women who practiced mindfulness vs. women who engaged in Kegels and mindfulness. Rosenbaum and Padua note in their book, The Overactive Pelvic Floor, “women who do not have a low-tone pelvic floor and who seek to enhance sexual arousal and more frequent orgasms have not much to gain from pelvic floor muscle training. Actually, a relaxed pelvic floor and mindful attention to sexual stimuli and bodily sensations seem a more effective means of enhancing sexual arousal and orgasm.” Various studies specifically studying the effect of mindfulness training have demonstrated both improved arousal and orgasm ability in women who practiced mindfulness. Brotto and Basson found their treatment group, which consisted of 68 otherwise healthy women, who underwent mindful meditation, cognitive behavioral training and education, improved in sexual desire, sexual arousal, lubrication, sexual satisfaction, and overall sexual functioning.
Cognitive-behavioral therapy appears to play a significant role in improving sexual function in women. Meston et. al. notes, “cognitive behavioral therapy for anorgasmia focuses on promoting changes in attitudes and sexually relevant thoughts, decreasing anxiety, and increasing orgasmic ability and satisfaction. To date there are no pharmacological agents proven to be beneficial beyond placebo in enhancing orgasmic function in women.”
Alas, there are no magic pills to create the above described “state of altered consciousness,” allowing women a sense of “well-being and contentment.” However, mindfulness training and cognitive behavioral therapy are both accessible and attainable for women who want to improve their ability to enjoy this much desired state. Many Pelvic floor therapist incorporate cognitive behavioral and mindfulness approaches in their practice.
The studies above mention pain as one of the factors for inability to experience arousal and orgasm. Hucker and Mccabe even noted that their mindfulness treatment group demonstrated significant improvements in all domains of female sexual response except for sexual pain. Dealing with sexual pain is a daily battle pelvic floor therapist face each day. So, how do women with sexual pain dysfunction differ from women who are experiencing sexual dysfunction but not pain? Let’s explore this in our next blog…
Chambless DL, Sultan FE, Stern TE, O’Neill C, Garrison S. Jackson A. Effect of pubococcygeal exercise on coital orgasm in women. J Consult CLin Psychol. 1984; 52:114-8
Bratto LA, Basson R. Group mindfulness-based therapy significantly improves sexual desire in women Behav Res Ther. 2014 Jun; 57:43-5
Hucker A. Mccabe MP. Incorporating Mindfulness and Chat Groups Into an Online Cognitive Behavioral Therapy for Mixed Female Sexual Problems. J Sex Res. 2015;52(6):627-33
Kontula O., Mettienen A. Determinants of female sexual orgasms. Socioaffect Neurosci Psychol. 2016 Oct 25;6:31624. doi: 10.3402/snp.v6.31624. eCollection 2016
Meston CM1, Levin RJ, Sipski ML, Hull EM, Heiman JR. Women’s orgasm. Annu Rev Sex Res. 2004;15:173-257. Review
Rosenbaum, Talli Y., Padoa, Anna. The overactive Pelvic floor. 1st ed. 2016
Roland DL, Cempel LM, Tempel AR. Women’s attributions on why they have difficulty reaching orgasm. J. Marital Therapy. 2018 Jan 3:0

This post is a follow-up to the February 20th post written by Nancy Cullinane, "Pelvic Floor One is Heading to Kenya"
By the time folks are reading this, Nancy Cullinane, PT, MHS, WCS, Terri Lannigan, PT, DPT, OCS, and I will likely be in a warm, crowded classroom in Nairobi, Kenya helping 30+ “physios” navigate the world of misbehaving bladders, detailed anatomy description, and their first internal lab experiences. No doubt it will be both challenging and extremely rewarding. We are so grateful to the Herman & Wallace Pelvic Rehab Institute for sharing their curriculum in partnership with the Jackson Clinics Foundation to allow us to offer their valuable curriculum in order to affect positive health care changes.
I personally am humbled and honored to get to play a small but key role in the development of foundational knowledge and skills for these women PT’s who will no doubt change the lives of countless Kenyan women, and, consequently, their families.
My adventure truly began when I offered to write lectures on the topics of Fistula and FGM/C (female genital mutilation/cutting) and I began the process of crash course learning about these topics. The quest has taken me on a deep dive into professional journals, NGO websites, surgical procedure videos and insightful interviews with some of the pioneers working for years including “in the field” to help women in Africa and in countries where these issues are prevalent.
Before I began my research on the topic of fistula, I pretty much thought of a fistula as a hole between two structures in the body where it doesn’t belong, and narrowly thought of in terms of anal fistulas, acknowledging how lucky we are that there are skilled colorectal surgeons who can fix them. But after more research, my world view changed. (Operative word here being “world”).
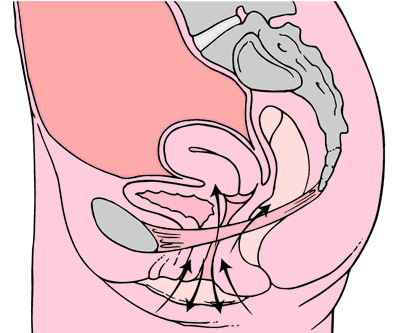
A fistula is an abnormal or surgically made passage between a hollow or tubular organ and the body surface, or between two hollow or tubular organs. For our purposes here today, I am referring to an abnormal hole or passage between the vagina and the bladder, or rectum, or both. When the fistula forms, urine and/or stool passes through the vagina. The results are that the woman becomes incontinent and cannot control the leakage because the vagina is not designed to control these types of body fluids.
According to the Worldwide Fistula Fund, there are ~ 2 million women and girls suffering from fistulas. Estimates range from 30 to 100 thousand new cases developing each year; 3-5 cases/1000 pregnancies in low-income countries. A woman may suffer for 1-9 years before seeking treatment. For women who develop fistula in their first pregnancy, 70% end up with no living children.
Vesicovaginal fistulas (VVF) can involve the bladder, ureters, urethra, and a small or large portion of the vaginal wall. Women with VVF will complain of constant urine leakage throughout the day and night, and because the bladder never fills enough to trigger the urge to void, they may stop using the toilet altogether. During the exam there may be pooling of urine in the vagina.
Rectovaginal Fistula is less common, and accounts for ~ 10% of the cases. Women with RVF complain of fecal incontinence and may report presence of stool in the vagina. These women often will also have VVF.
In Kenya, most fistulas are obstetric fistulas, which occur as a result of prolonged obstetric labor (POL). These are also called gynecologic, genital, or pelvic fistulas. Traumatic fistulas account for 17-24 % of the cases and are caused by rape, sexual or other trauma, and sometimes even from FGM/C. The other type of fistula by cause is iatrogenic, meaning unintentionally caused by a health care provider during procedures such as during a C-section, hysterectomy, or other pelvic surgery. Most fistulas seen in the US are of this type.
Prolonged Obstructed Labor most often occurs when the infant’s head descends into the pelvis, but cannot pass though because of cephalo-pelvic disproportion (mismatch between fetus head and mother’s pelvis) thus creating sustained pressure on the tissues separating the tissues of the vagina and bladder or rectum, (or both) leading to a lack of blood flow and ultimately to necrosis of the tissue, and the development of the fistula. Those who develop this type of fistula spend an average of 3.8 days in labor (start of uterine contractions), some up to a week. In these cases, family members or traditional birth attendants may not recognize this is occurring, and even if they do, they may not have the instrumentation, the facilities or the skills necessary to handle the situation with an instrumental delivery or a C-section. And many of these women are in remote locations without transportation to appropriate facilities or lack the money to pay for procedures.
There are many adverse events and medical consequences that can result as a result of untreated obstetrical fistulas including the death of the baby in 90% of the cases. Physical effects besides the incontinence previously mentioned can include lower extremity nerve damage, which can be disabling for these women, along with a host of other physical and systemic health issues. The social isolation, ostracization by community, divorce, and loss of employment can lead to depression, premature lifespan, and sometimes suicide.
The good news is there are several great organizations making a difference.
In most cases, surgery is needed to repair the fistula. Sometimes, however, if the fistula is identified very early, it may be treated by placing a catheter into the bladder and allowing the tissues to heal and close on their own, and this is more viable in high-income countries after iatrogenic fistulas, but unfortunately, most women in the low-income countries have to wait for months or years before they receive any medical care.
There is an 80-90% cure rate depending on the severity, but according to the Worldwide Fistula Fund, 90% are left untreated, as the treatment capacity is only around 15,000 per year for the 100,00 new patients requiring it. Prevention is vital.
Despite successful repair of vesicovaginal fistulas, research shows that 15-35% of women report post-op incontinence at the time of discharge from the hospital, and that 45-100% of women may become incontinent in the years following their repair. Studies suggest that scar tissue-fibrosis of the abdominal wall and pelvis, and vaginal stenosis are strongly associated with post-operative incontinence.
According to research by Castille, Y-J et al in Int. J Gynecology Obstet 2014, there can be improved outcome of surgery both in terms of successful closure of vesicovaginal fistula and reduced risk of persistent urinary incontinence if women are taught a correct pelvic floor muscle contraction and advised to practice PFM exercise. Other studies have shown a positive effect from pre and post op PT in both post op urinary incontinence and PFM strength and endurance with a reduction of incontinence in more than 70% of treated patients, with improvements maintained at the 1year follow up. SO, THIS IS ONE REASON WE ARE SO EXCITED TO BE GOING TO KENYA!
I inquired about the use of dilators via email communication with surgeon Rachel Pope , MD MPH who has done extensive work in Malawi with women who have suffered from fistula, including the use of dilators, and her response was: “in women who have had obstetric fistula the dilators seem only marginally helpful after standard fistula repairs. The key is to have a good vaginal reconstructive surgery where skin flaps that still maintain their blood supply replace the area in the vagina previously covered by scar tissue. The dilators work exceedingly well when there is healthy tissue in place, and I think the overall outcomes are better for women in those scenarios compared to the cement-like scar we often see in women with fistulas.”
In the US, there are specialist surgeons who provide surgical repairs. While genitourinary fistulas can occur because of obstructed labor and operative deliveries in high income countries, they can also occur in a variety of pelvic surgeries, post pelvic radiation, as well as in cases of cancer, infections, with stones, and as well etiology includes instrumentations such as D&Cs, catheters, endoscopic trauma, and pessaries, and as well in cases of foreign bodies, accidental trauma, and for congenital reasons. As pelvic therapists it is important to know your patients’ surgical and medical history and to pay special attention to the patient’s history regarding their incontinence description and onset and be mindful during exam to notice possible pooling of urine in the vagina. Though rare in terms of occurrence, we should be aware of the possibility and may play a role in referring the patient to a physician who can do further diagnostic testing
In conclusion, I want to thank UK physiotherapist Gill Brook MCSP (DSA) CSP MSC, president of the IOPTWH who shared with me by interview her knowledge of fistula and experiences with the Addis Ababa Fistula Hospital in Ethiopia, which she has been visiting for 10 years, as well as Seattle’s Dr. Julie LaCombe MD FACOG who has performed fistula surgeries in Uganda and Bangladesh and met with me personally to share about obstetrical trauma and fistula surgery and management.
Nancy, Terri and I will look forward to sharing photos and more about our journey and experiences, upon our return. In the meantime, check out the Campaign to End Fistula and join the campaign.
Andrea Wood, PT, DPT, WCS, PRPC is a pelvic health specialist at the University of Miami downtown location. She is a board certified women’s health clinical specialist (WCS) and a certified pelvic rehabilitation practitioner (PRPC). She is passionate about orthopedics and pelvic health. In her spare time, you can find her enjoying the south Florida outdoors.
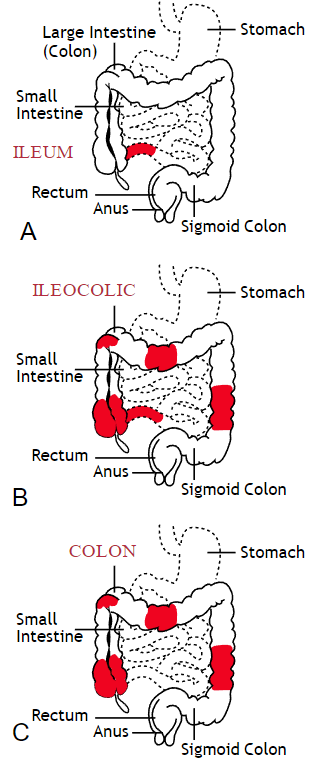
Inflammatory bowel disease (IBD) includes the two diagnosis of Crohn’s Disease and Ulcerative Colitis. While both can cause similar health effects, the differences of the disease pathologies are listed below:1
| Ulcerative Colitis | Crohn’s Disease | |
| Affected Area |
|
|
| Pattern of Damage |
|
|
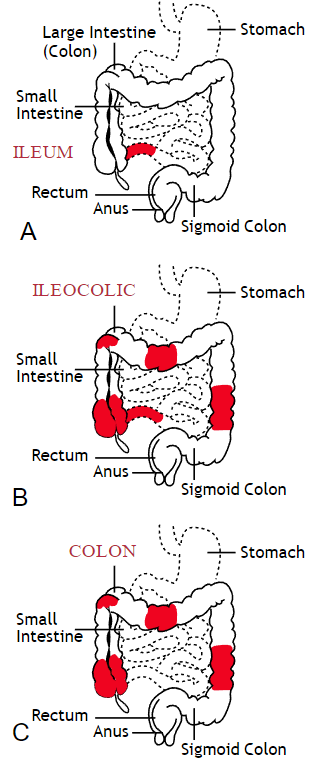
Common complications experienced by patients with IBD include fecal incontinence, fecal urgency, night time soiling, urinary incontinence, abdominal pain, hip and core weakness, pelvic pain, fatigue, osteoporosis, and sarcopenia. In a sample of 1,092 patients with Crohn’s Disease, Ulcerative Colitis, or unclassified IBD, 57% reported fecal incontinence. Fecal incontinence was reported not only during periods of flare ups, but also during remission periods.2 One common factor affecting fecal incontinence is external anal sphincter fatigue. External anal sphincter fatigue has also been shown to be present in IBD patients who are not experiencing fecal incontinence or fecal urgency. IBD patients have been shown in studies to have similar baseline pressures versus healthy matched controls, thus indicating the possibility that deficits in endurance versus strength can play a larger role in fecal incontinence.3 Other factors contributing to fecal incontinence include post inflammatory changes that may alter anorectal sensitivity, anorectal compliance, neuromuscular coordination, and cause visceral hypersensitivity. Visceral hypersensitivity may be caused by continuous release of inflammatory mediators found in patients with IBD. It is also important to screen properly for incomplete bowel emptying and stool consistency to rule out overflow diarrhea or fecal impaction. Reports of need to splint digitally for full evacuation may indicate incomplete bowel emptying and defaectory disorders such as paradoxical contraction of the puborectalis muscle or rectocele. Anorectal manometry testing may be highly useful in identifying patients likely to improve from biofeedback therapy.4
Urinary incontinence can also be another secondary consequence to IBD. In a sample of 4,827 patients with IBD, 1/3 of responders reported urinary incontinence that was strongly associated with the presence of fecal incontinence. Frequent toilet visits for defecation may stimulate overactive bladder. Women were more likely to experience fecal incontinence versus men. One possible mechanism for increased fecal incontinence in women is men often have a longer and more complete anal sphincter that may be protective of fecal incontinence.5
Physical activity has been shown to be lower in patients with IBD versus healthy controls. 6, 7 Guiding IBD patients in proper exercises programs can have great benefits. Exercise may reduce inflammation in the gut and maintain the integrity of the intestines, reducing inflammatory bowel disease risk.8 It can also help increase bone mass density, an important factor in IBD patients who are at greater risk for osteoporosis. It has also been shown to help general fatigue in IBD patients. Patients with Crohn’s disease who participate in higher exercise levels may be less likely to develop active disease at 6 months. Treadmill training at 60% VO2 max and running three times a week has not been shown to evoke gastrointestinal symptoms in IBD patients. An increase of BMI predicts poorer outcomes and shorter time to first surgery in patients with Crohn’s disease.6
Conservative physical therapy interventions for treating IBD symptoms can include the following:
| Symptoms resulting from IBD | Physical Therapy Interventions |
| Fecal Incontinence (FI) |
|
| Urinary urgency |
|
| Sarcopenia |
|
| Fatigue |
|
| Pelvic Pain |
|
Surgical interventions for IBD are dependent upon what type of disease the patient has and what areas of the intestines are affected the most. Surgery may be considered once the disease has become non responsive to medication therapy and quality of life continues to decline. A colectomy involves removing the colon while a proctocolectomy involves both removal of the colon and rectum. For ulcerative colitis patients, options include total proctocolectomy with end ileostomy or a restorative proctocolectomy with ileal pouch anal anastomosis. Restorative proctocolectomy eliminates the need for an ostomy bag making it the preferred surgery of choice if possible and gold standard for ulcerative colitis patients.10 For patients with Crohn’s disease, options include resection of part of the intestines followed by an anastomosis of the remaining healthy ends of the intestines, widening of the narrowed intestine in a procedure called a strictureplasty, colectomy or proctocolectomy, fistula repair, and removal of abscesses if needed.11
1. Crohn’s and Colitis Foundation. 2019. What is Crohn’s Disease. Retrieved from: http://www.crohnscolitisfoundation.org/what-are-crohns-and-colitis/what-is-crohns-disease/
2. Vollebregt PF, van Bodegraven A, Markus-de Kwaadsteniet T, et al. Impacts on perianal disease and faecal incontinence on quality of life and employment in 1092 patients with inflammatory bowel disease. Ailment Pharmacol Ther. 2018; 47: 1253-1260
3. Athanasios A, Kostantinos H, Tatsioni A et al. Increased fatigability of external anal sphincter in inflammatory bowel disease: significance in fecal urgency and incontinence. J Crohns Colitis (2010) 4: 553-560.
4. Nigam G, Limdi J, Vasant D. Current perspectives on the diagnosis and management of functional anorectal disorders in patients with inflammatory bowel disease. Therap Adv Gastroenterol. 2018 Dec 6: doi: 10.1177/1756284818816956
5. Norton C, Dibley L, Basset P. Faecal incontinence in inflammatory bowel disease: Associations and effect on quality of life. J Crohn’s Colitis. (2013) 7, e302-e311.
6. Biliski J, Mazur-Bialy A, Brzozowski B et al. Can exercise affect the course of inflammatory bowel disease? Experimental and clinical evidence. Pharmacological Reports. 2016 (68): 827-836.
7. Tew G, Jones K, Mikocka-Walus A. Physical activity habits, limitations, and preditors in people with inflammatory bowel disease: a large cross-sectional online survey. Inflamm Bowel Dis. 2016; 22(12): 2933-2942.
8. Vincenzo M, Villano I, Messina A. Exercise modifies the gut microbiota with positive health effects. Oxidative Medicine and Cellular Longevitiy. 2017: Article ID 3831972.
9. Cramer H, Schafer M, Schols M. Randomised clinical trial: yoga vs written self care advice for ulcerative colitis. Aliment Pharmacol Ther. 2017; 45: 1379-1389.
10. Cornish J, Wooding K, Tan E, et al. Study of sexual, urinary, and fecal function in females following restorative proctocolectomy. Inflamm Bowel Dis. 18 (9) 2012. 1601-160
11. Crohn’s and Colitis Foundation. 2019. Surgery Options. Retrieved from: http://www.crohnscolitisfoundation.org/what-are-crohns-and-colitis/what-is-crohns-disease/surgery-options.html
Today's guest post comes from Kelsea Cannon, PT, DPT, a pelvic health practitioner in Seattle, WA. Kelsea graduated from Des Moines University in 2010 and practices at Elizabeth Rogers Pilates and Physical Therapy.
Many studies done on pelvic floor muscle training largely have subjects who are Caucasian, moderately well educated, and receive one-on-one individualized care with consistent interventions. This led a group of researchers to investigate the occurrence of pelvic floor dysfunction, specifically pelvic organ prolapse (POP), in parous Nepali women. These women are known to have high incidences of POP and associated symptomology. Another impetus to perform this research: the discovery that there was a major lack of proper pelvic floor education for postpartum women. These women were commonly encouraged to engage their pelvic floor muscles via performing supine double leg lifts, sucking in their tummies/holding their breath/counting to ten, and squeezing their glutes. These exercises would be on a list of no-no’s here in the United States. In 2017, Delena Caagbay and her team of researchers discovered that in Nepal, no one really knew the correct way to teach proper pelvic floor muscle contractions, preventing the opportunity for women to better understand their pelvic floors. The team then set out to investigate the needs of this population, with the eventual goal of providing effective pelvic floor education for Nepali women.
 Caagbay and her team first wanted to know what baseline muscle activity the Nepali women had in their pelvic girdle. Physical examinations and internal pelvic floor muscle strength assessments revealed that surprisingly there was a low prevalence of pelvic floor muscle defects, such as levator avulsions and anal sphincter trauma. Uterine prolapses were most common while rectoceles were comparatively less common. Their muscles were also strong and well-functioning, often averaging a 3/5 on the Modified Oxford Scale. It was hypothesized that these women had low prevalence of muscle injury because instruments were not commonly used during childbirth, they had lower birth weight babies, and the women were typically younger when giving birth (closer to 20-21 years old). But they had a high prevalence of POP even with good muscle tone? Researchers suggested that their incidence of POP is likely stemming from their sociocultural lifestyle requirements, as women are left to do most of the daily household chores and caregiving tasks while men often travelled away from the home to perform paid labor. Physical responsibilities for these women commonly begin at younger ages and while it helps promote good muscle tone, the heavier loading places pressure on the connective tissue and fascia that support the pelvic organs. Because of the demands of their lifestyles, Nepali women are often forced to return to their physically active state within a couple weeks after giving birth.
Caagbay and her team first wanted to know what baseline muscle activity the Nepali women had in their pelvic girdle. Physical examinations and internal pelvic floor muscle strength assessments revealed that surprisingly there was a low prevalence of pelvic floor muscle defects, such as levator avulsions and anal sphincter trauma. Uterine prolapses were most common while rectoceles were comparatively less common. Their muscles were also strong and well-functioning, often averaging a 3/5 on the Modified Oxford Scale. It was hypothesized that these women had low prevalence of muscle injury because instruments were not commonly used during childbirth, they had lower birth weight babies, and the women were typically younger when giving birth (closer to 20-21 years old). But they had a high prevalence of POP even with good muscle tone? Researchers suggested that their incidence of POP is likely stemming from their sociocultural lifestyle requirements, as women are left to do most of the daily household chores and caregiving tasks while men often travelled away from the home to perform paid labor. Physical responsibilities for these women commonly begin at younger ages and while it helps promote good muscle tone, the heavier loading places pressure on the connective tissue and fascia that support the pelvic organs. Because of the demands of their lifestyles, Nepali women are often forced to return to their physically active state within a couple weeks after giving birth.
After assessing the current needs, cultural norms, and prevalence of POP in Nepali women, Caagbay et al created an illustrative pamphlet on how to contract pelvic floor muscles as well as provided verbal instruction on pelvic floor muscle activation. Transabdominal real time ultrasound was applied to assess the muscle contraction of 15 women after they received this education. Unfortunately, even after being taught how to engage their pelvic floor muscles, only 4 of 15 correctly contracted their pelvic floors.
This study highlighted that brief verbal instruction plus an illustrative pamphlet was not sufficient in teaching Nepali women how to correctly contract their pelvic floor muscles. Although there was a small sample size, these results can likely be extrapolated to the larger population. Further research is needed to determine how to effectively teach correct pelvic floor muscle awareness to women with low literacy and/or who reside in resource limited areas. Lastly, it is important to consider the significance of fascial and connective tissue integrity within the pelvic floor when addressing pelvic organ prolapse.
1 Can a leaflet with brief verbal instruction teach Napali women how to correctly contract their pelvic floor muscles? DM Caagbay, K Black, G Dangal, C Rayes-Greenow. Journal of Nepal Health Research Council 15 (2), 105-109.
https://www.nepjol.info/index.php/JNHRC/article/viewFile/18160/14771
2 Pelvic Health Podcast. Lori Forner. Pelvic organ prolapse in Nepali women with Delena Caagbay. May 31, 2018.
3 The prevalence of pelvic organ prolapse in a Nepali gynecology clinic. (2017) F. Turel, D. Caagbay, H.P. Dietz. Department of Obstetrics and Gynecology, Sydney Medical School Napean, University of Sydney.
4 The prevalence of major birth trauma in Nepali women. (2017) F. Turel, D. Caagbay, H.P. Dietz. Department of Obstetrics and Gynecology, Sydney Medical School Nepean, University of Sydney.
The following is a guest submission from Alysson Striner, PT, DPT, PRPC. Dr. Striner became a Certified Pelvic Rehabilitation Practitioner (PRPC) in May of 2018. She specializes in pelvic rehabilitation, general outpatient orthopedics, and aquatics and treats at Carondelet St Joesph’s Hospital in the Speciality Rehab Clinic located in Tucson, Arizona.
Recently, I had a patient present with Complex Regional Pain Syndrome (CRPS) on his right foot. He stated that the pain had started about 10 days after his prostatectomy when someone had fallen onto his right foot. He reported a bunionectomy on that foot 7 years prior and noted an episode of plantar facilities before his prostatectomy. CRPS is defined as “chronic neurologic condition involving the limbs characterized by severe pain along with sensory, autonomic, motor, and trophic impairments” in a 2017 article "Complex regional pain syndrome; a recent update" by Goh, En Lin. The article goes on to discuss how CRPS can set off a cascade of problems including altered cutaneous innervation, central and peripheral sensitization, altered sympathetic nervous system function, circulating catecholamines, changes in autoimmunity, and neuroplasticity.
 A recent persistent pain theory to explain the relationship between pelvic floor and his foot could be overflow or ‘smudging’ in his homunculus. The homunculus is the map of our physical body in our brain where the feet are located next to the genitals. Possibly when one has pain, there can be ‘smudging’ of our mental body map from one area into another. I have heard this explained as though a chalk or charcoal drawing has been swipes their hand through the picture. A recent study by Schrabrun, SM et al “Smudging of the Motor Cortex is Related to the Severity of Low Back Pain” found that people with chronic low back pain had a loss of cortical organization which and that this loss was associated with the severity and location of LBP.
A recent persistent pain theory to explain the relationship between pelvic floor and his foot could be overflow or ‘smudging’ in his homunculus. The homunculus is the map of our physical body in our brain where the feet are located next to the genitals. Possibly when one has pain, there can be ‘smudging’ of our mental body map from one area into another. I have heard this explained as though a chalk or charcoal drawing has been swipes their hand through the picture. A recent study by Schrabrun, SM et al “Smudging of the Motor Cortex is Related to the Severity of Low Back Pain” found that people with chronic low back pain had a loss of cortical organization which and that this loss was associated with the severity and location of LBP.
There are many ways to improve the organization of the homunculus and create neuroplasticity. One such way was suggested is with Transcutaneous electrical nerve stimulation (TENS) to the bottom of the foot to affect bladder spasms and pain. In recent study, “Transcutaneous electrical stimulation of somatic afferent nerves of the foot relieved symptoms related to postoperative bladder spasms,". Zhang, C et al. 2017 found that participates that had either a bladder surgery or a prostate surgery had improvement in bladder spasm symptoms and VAS scores on day two and three. Their protocol was to use two electrodes over the bottom of the foot at 5 Hz with 0.2 millisecond pulse width until a muscle twitch was achieved and was increased, but still comfortable for an hour (there is a picture of electrode placement in the article). The authors note that this neuromodulation of the foot sensory nerves may inhibit interactions between the somatic peripheral neuropathway and autonomic micturition reflex to calm the bladder and pain.
No matter what we do to help calm nervous systems from the top down; pain neuroscience education, mindful based relaxation, graded motor imagery, or from the bottom up; de-sensitization, biofeedback, or good old-fashioned TENS. The result is the same; a cortical organization and happier patients.
En Lin Goh†, Swathikan Chidambaram† and Daqing Ma. "Complex regional pain syndrome: a recent update". Burns & Trauma 2017 5:2.https://doi.org/10.1186/s41038-016-0066-4"
Schabrun SM, Elgueta-Cancino EL, Hodges PW. "Smudging of the Motor Cortex Is Related to the Severity of Low Back Pain." Spine (Phila Pa 1976). 2017 Aug 1;42(15):1172-1178. doi: 10.1097/BRS.0000000000000938
Chanjuan Zhang, et al. "Transcutaneous electrical stimulation of somatic afferent nerves in the foot relieved symptoms related to postoperative bladder spasms". BMC Urol. 2017; 17: 58. doi: 10.1186/s12894-017-0248-9