Hypopressive Exercise for Post-prostatectomy Incontinence
Tamara Rial, PhD, CSPS, co-founder and developer of Low Pressure Fitness will be presenting the first edition of “Low Pressure Fitness and abdominal massage for pelvic care” in Princeton, New Jersey in July, 2018. Tamara is internationally recognized for her work with hypopressive exercise and Low Pressure Fitness. In this article she presents the novel topic of hypopressives as a complementary pelvic floor muscle training tool for incontinence after prostate cancer surgery.
Urinary Incontinence is the most common side effect men suffer after prostate cancer surgery along with erectile dysfunction. Although it is not life threatening, urinary incontinence definitely has a negative impact on the patient’s quality of life Sountoulides et al., 2013. Beyond the frustration and embarrassment associated with pelvic floor dysfunction, many patients describe it as depressing, disheartening and devastating.
The first line of conservative treatment - and most often recommended - is pelvic floor muscle training Andersen et al., 2015. Over the past few years, some researchers have also recommended alternative exercise programs with a holistic approach such as Pilates and hypopressives to improve the patient’s quality of life and urinary incontinence symptoms (Santa Mina et al., 2015). These alternative pelvic floor muscle training programs draw upon the connection between the pelvic floor, it’s synergistic muscles (abdominal, pelvic, lumbar) and their interrelated role in posture and breathing Hodges, 2007; Sapsford, 2004; Madill and McLean, 2008; Talasz et al., 2010. Among these complementary exercise programs, hypopressives have gained increasing attention for the recovery of post-prostatectomy urinary incontinence Santa Mina et al., 2015; Mallol-Badellino, et al. 2015.
What is known about hypopressives for post-prostatectomy incontinence?
Although hypopressive exercise has become popular for women, some researchers, clinicians and practitioners have begun to apply these exercises for specific male issues such as urinary incontinence following a prostatectomy. Recently, a case-study I co-authored about an adapted program of hypopressive exercise for urinary incontinence following a radical prostatectomy surgery was published in the Journal of the Spanish physiotherapy association Chulvi-Medrano & Rial, 2018. We describe the case of a 46-year-old male with severe stress urinary incontinence six months after surgery. We used a pelvic floor exercise program consisting of hypopressive exercises as described in the Low Pressure Fitness level 1 practical manual Rial & Pinsach, 2017 combined with contraction of the pelvic floor muscles. Satisfactory results were obtained after the rehabilitation protocol as evidenced by a reduction from 3 daily pads to none. Of note, clinical trails have demonstrated the benefits of initiating a rehabilitation program to strengthen the pelvic floor as soon as possible after prostatectomy. Previously, I’ve studied hypopressive exercise for female urinary incontinence Rial et al., 2015 and for the improvement of female athletes pelvic floor function Álvarez et al., 2016. However, this was the first time we’ve studied hypopressives in the context of male urinary leakage.
In the same light, other researchers have also included hypopressives in their pelvic floor training protocol for post-prostatectomy urinary incontinence. For example, Serda et al (2010) and Mallol-Badellino (2015) used protocols that combined pelvic floor contractions with postural re-education and hypopressives. Both studies found improvements in the severity of involuntary leakages and improvements in the patients’ quality of life. Similar results are also described in the clinical case by Scarpelini et al. (2014) who used hypopressives and psoas stretching exercises to reduce urinary incontinence after prostatectomy.
But how do hypopressives work?
The hypothesis underlying the use of hypopressives as a complementary pelvic floor and core exercise program is that it retrains the core system with specific postural and breathing strategies while reducing pressure on the pelvic organs and structures. The most striking part of hypopressives breathing technique is the abdominal vacuum. This breathing maneuver involves a low pulmonary volume exhale-hold technique followed by a rib-cage expansion involving the activation of the inspiratory muscles. The rib-cage expansion during the breath-holding phase leads to a noticeable draw-in of the abdominal wall and simultaneously to the rise of the thoracic diaphragm. Recent observational studies have shown how the hypopressive technique was able to elevate the pelvic viscera and to activate the pelvic floor and deep core muscles in women trained with hypopressives Navarro et al., 2017. From an historical point of view, this characteristic breathing maneuver was first described and practiced as a yoga pranayama called Uddiyanha Bandha Omkar & Vishwas, 2009.
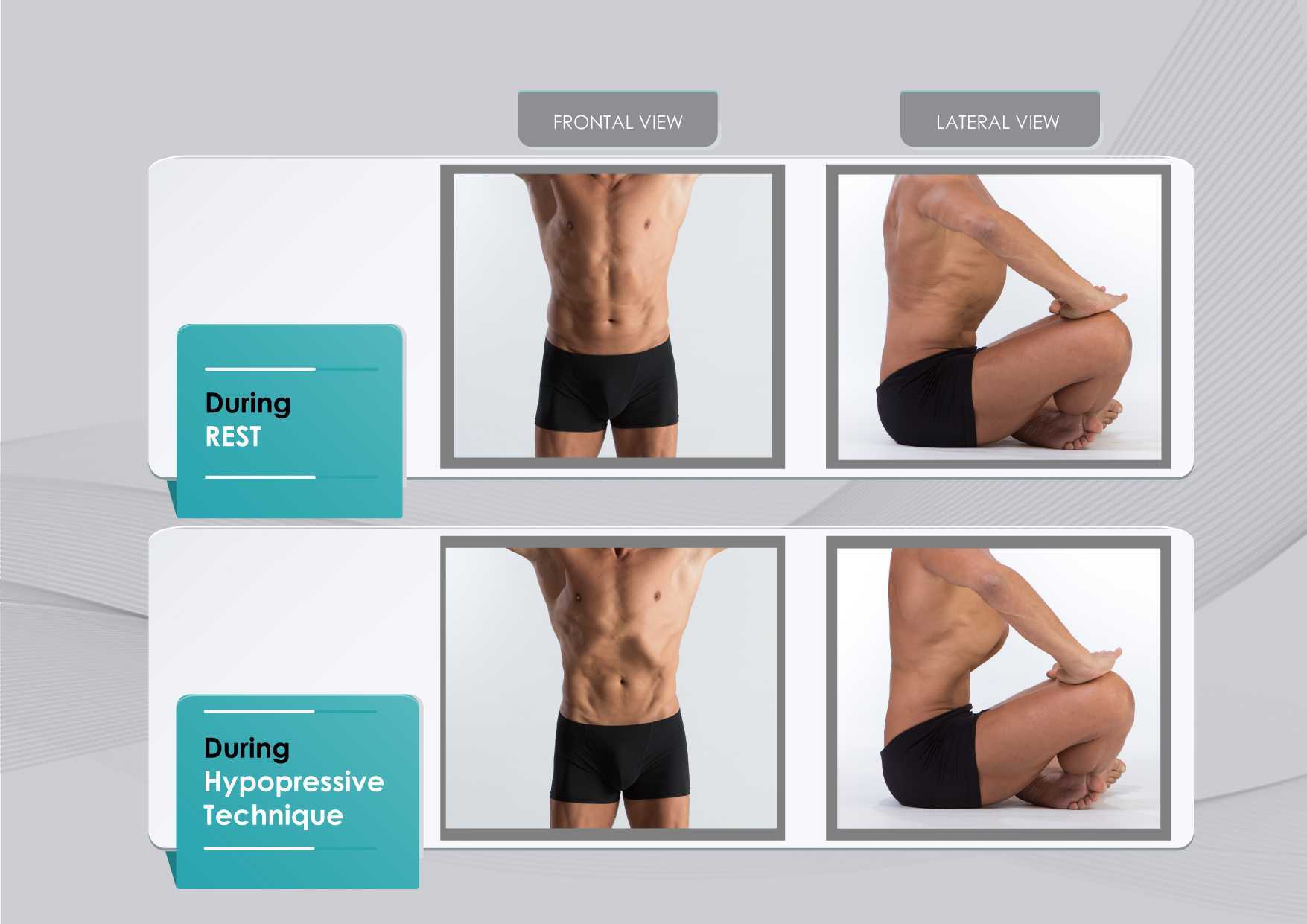
Figure 1 shows the anatomical behavior of the rib cage and the abdominal wall when performing the hypopressive breathing maneuver, which should not be confused with an abdominal hollowing, or a bracing maneuver. Anatomical observation of the thoracic and abdominal behavior during the breathing maneuver of the hypopressive exercise. Figure elaborated by the author.
In addition to breath control, the hypopressive technique involves a series of static and dynamic poses which operate on the hypothesis of training the stabilizing muscles of the spine, such as the core and pelvic muscles. In this sense, hypopressives are not exclusively a breathing technique, but rather they are an integrated whole-body technique. The practice of hypopressives involves body control, body awareness, postural correction and mindfulness throughout its different poses and postural techniques. The introduction of holistic exercise programs to train the synergist pelvic floor muscles and breathing patterns can be viewed as complementary tools for the restoration of a patient’s body awareness and functionality.
Another hypothesis of the effects of the hypopressive-breathing in the pelvic floor is the ability to move the pelvic viscera cranially as a consequence of the ribcage opening up after the breath-hold. This vacuum lifts the diaphragm and consequently creates an upward tension on the transversalis fascia, the peritoneum and other related fascial structures. In addition to the diaphragmatic suction effect, a correct alignment of the rib cage and pelvis during the exercise contributes to an improved suspension and position of the viscera in the pelvis. The mobility achieved with the breathing and its body sensations may be one of the reasons why hypopressives have also been recommended as a proprioceptive facilitator for those with low ability to “find their pelvic floor” Latorre et al., 2011.
It’s crucial to highlight that a complete surgical resection of the prostate will cause - in most of the cases - post-operative fibrosis and neurovascular damage Hoy-Land et al., 2014. Both, the neurovascular and musculoskeletal injuries are contributing factors for urinary incontinence post-prostatectomy. Subsequently, exercises focusing on increasing local vascular irrigation and re-activating the damaged musculature have been highlighted as the main goals to help patients recover continence. In this sense, breathing movements, fascia manipulation and decreased pelvic pressure can result in increased vascular supply. A previous study has shown an improvement in venous return of the femoral artery during the hypopressive-breathing maneuver Thyl et al., 2009. Collectively, all these factors may favor microcirculation in the pelvic area. Finally, the muscle activation of the pelvic floor and core muscles observed during the practice of hypopressives (Ithamar et al., 2017) and the changes of puborectalis and iliococcygeus muscles after an intensive pelvic floor muscle training (Dierick et al., 2018) are other factors that could have impact on urge incontinence, stress incontinence and overflow incontinence symptoms common after prostatectomy surgeries.
To date, the results from these investigations and clinical reports open new complementary pelvic floor training strategies for the treatment of post-prostatectomy incontinence. Hypopressives and pelvic floor muscle exercises are non-invasive, don’t require expensive material, and provide an exercise-based approach as part of a healthy lifestyle. However, qualified instruction, technique-driven progression and adherence to the intervention are critical components of any pelvic floor and hypopressive training protocol.
Álvarez M, Rial T, Chulvi-Medrano I, García-Soidán JL, Cortell JM. 2016. Can an eight-week program based on the hypopressive technique produce changes in pelvic floor function and body composition in female rugby players? Retos nuevas Tendencias en Educación Física, Deporte y Recreación, 30(2): 26-29.
Anderson CA, Omar MI, Campbell SE, Hunter KF, Cody JD, Glazener CM. 2015. Conservative management for postprostatectomy urinary incontinence. Cochrane Database Syst Rev, 1:CD001843.
Chulvi-Medrano I, Rial T. 2018. A case study of hypopressive exercise adapted for urinary incontinence following radical prostactetomy surgery. Fisioterapia, 40, 101-4. Doi: DOI: 10.1016/j.ft.2018.01.004
Dierick F, Galrsova E, Laura C, Buisseret F, Bouché FB, Martin L. 2018. Clinical and MRI changes of puborectalis and iliococcygeus after a short period of intensive pelvic floor muscles training with or without instrumentation. European Journal of Applied Physiology, doi:10.1007/s00421-018-3899-7
Ithamar, L., de Moura Filho, A.G., Benedetti-Rodrigues, M.A., Duque-Cortez, K.C., Machado, V.G., de Paiva-Lima, C.R.O., et al. 2017. Abdominal and pelvic floor electromyographic analysis during abdominal hypopressive gymnastics. J. Bodywork. Mov. Ther. doi: 10.1016/j.jbmt.2017.06.011.
Latorre G, Seleme M, Resende AP, Stüpp L, Berghmans B. Hypopressive gymnastics: evidences for an alternative training for women with local proprioceptive deficit of the pelvic floor muscles. Fisioterapia Brasil 2011; 12(6): 463-6.
Hodges P. 2007. Postural and respiratory functions of the pelvic floor muscles. Neurourol Urodyn, 26(3): 362-371.
Hoyland K, Vasdev N, Abrof A, Boustead G. 2014. Post-radical prostatectomy incontinence: etiology and prevention. Rev Urol. 16(4), 181-8.
Madill, S., McLean, L. 2008. Quantification of abdominal and pelvic floor muscle synergies in response to voluntary pelvic floor muscle ontractions. J. Electromyogr. Kinesiol. 18, 955-64. doi: 10.1016/j.jelekin.2007.05.001.
Mallol-Badellino J., et al. 2015. Resultados en la calidad de vida y la severidad de la incontinencia urinaria en varones prostatectomizados por neoplasia de próstata. Rehabilitación, 49(4); 210-215.
Navarro, B., Torres, M., Arranz, B. Sánchez, O. 2017. Muscle response during a hypopressive exercise after pelvic floor physiotherapy: Assessment with transabdominal ultrasound. Fisioterapia. 39, 187-194. doi:10.1016/j.ft.2017.04.003.
Omkar, S., Vishwas, B. 2009. Yoga techniques as a means of core stability training. J. Bodywork Mov. Thep. 13, 98-103. doi: 10.1016/j.jbmt.2007.10.004.
Rial T, Chulvi-Medrano I, Cortell-Tormo JM, Álvarez M. 2015. Can an exercise program based on hypopressive technique improve the impact of urinary incontinence on women´s quality of life? Suelo Pélvico, 11:27-32.
Rial, T., Pinsach, P. 2017. Low Pressure Fitness practical manual level 1. International Hypopressive and Physical Therapy Institute, Vigo.
Santa Mina D, Au D, Alibhai S, Jamnicky L, Faghani N, Hilton W, Stefanky L, et al. 2015. A pilot randomized trial of conventional versus advanced pelvic floor exercises on treat urinary incontinence after radical prostatectomy: a study protocol. BMC Urology, 15. DOI 10.1186/s12894-015-0088-4
Sapsford R. 2004. Rehabilitation of pelvic floor muscles utilizing trunk stabilization. Man Ther, 9(1): 3-12.
Serdá B, Vesa, A. del Valle, y Monreal P. 2010. La incontinencia urinaria en el cáncer de próstata: diseño de un programa de rehabilitación. Actas Urológicas Españolas, 34(6): 522-30.
Scarpelini P, Andressa Oliveira F, Gabriela Cabrinha S, Cinira H. 2014. Protocolo de ginástica hipopressiva no tratamento da incontinência urinária pós-prostatectomia: relato de caso. UNILUS Ensino e Pesquisa, 11(23): 90-95
Talasz, H., Kofler, M., Kalchschmid, E., Pretterklieber, M., Lechleitner, M. 2010. Breathing with the pelvic floor? Correlation of pelvic floor muscle function and expiratory flows in healthy young nulliparous women. Int. Urogynecol. J. 21, 475-81. doi: 10.1007/s00192-009-1060-1.
Thyl S., Aude P, Caufriez M, Balestra C. 2009. Incidence de l'aspiration diaphragmatique associée à une apnée expiratoire sur la circulation de retour veineuse fémorale: étude par échographie-doppler. Kinésithérapie scientifique, 502; 27-30.
By accepting you will be accessing a service provided by a third-party external to https://www.hermanwallace.com/








































