Striking a Chord with Coccydynia
In my mid 20’s I had a sudden onset of severe, persistent pain at the bottom of my spine. I had fallen while running on trails and thought maybe I had fractured my coccyx. It hurt terribly to sit, especially on hard surfaces. When I finally succumbed to seeing a doctor, he diagnosed me with a pilonidal cyst and performed a simple excision of the infection right there in the office. I recall passing out on the table and waking up with an open wound stuffed with gauze. What I thought was “just” coccydynia turned out to be something completely different, requiring a specific and immediately effective treatment.
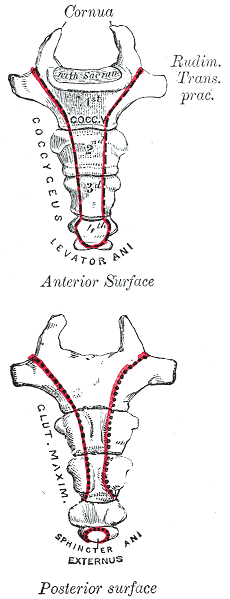 Differential diagnosis is essential in all medical professions. Blocker, Hill, and Woodacre2011 presented a case report on persistent coccydynia and the necessity of differential diagnosis. A 59-year old female reported constant coccyx pain after falling at a wedding. Her initial x-rays were normal, as was an MRI a year later, despite continued pain. Neither an ultrasound nor abdominal CT scan was performed until 16 months after the onset of pain, which was 2 months after she started having bladder symptoms. A CT scan then showed a tumor stemming from her sacrum and coccyx, and an MRI confirmed the sacrum as the tumor location. Chordomas are primary bone tumors generally found at the sacrum and coccyx or the base of the skull. They are relatively rare; however, they do exist in males and females and can present as low back pain, a soft tissue mass, or bladder/bowel obstruction. Clinicians need to listen for red flags of night pain and severe, unrelenting pain and ensure proper examination is performed for accurate diagnosis and expedient treatment.
Differential diagnosis is essential in all medical professions. Blocker, Hill, and Woodacre2011 presented a case report on persistent coccydynia and the necessity of differential diagnosis. A 59-year old female reported constant coccyx pain after falling at a wedding. Her initial x-rays were normal, as was an MRI a year later, despite continued pain. Neither an ultrasound nor abdominal CT scan was performed until 16 months after the onset of pain, which was 2 months after she started having bladder symptoms. A CT scan then showed a tumor stemming from her sacrum and coccyx, and an MRI confirmed the sacrum as the tumor location. Chordomas are primary bone tumors generally found at the sacrum and coccyx or the base of the skull. They are relatively rare; however, they do exist in males and females and can present as low back pain, a soft tissue mass, or bladder/bowel obstruction. Clinicians need to listen for red flags of night pain and severe, unrelenting pain and ensure proper examination is performed for accurate diagnosis and expedient treatment.
In a more recent case study by Gavriilidid & Kyriakou 2013, a 73 year old male presented with 6 months of tailbone pain, worse with sitting and rising from sitting. The physician initially referred him to a surgeon for a pilonidal cyst he diagnosed upon palpation. The surgeon found an unusual mass and performed a biopsy, which turned out to be a sacrococcygeal chordoma. The tumor was excised surgically along with the gluteal musculature, coccyx, and the fifth sacral vertebra, as well as a 2cm border of healthy tissue to minimize risk of recurrence of the chordoma. These authors reported coccygodynia is most often caused by pilonidal disease, clinically confirmed by abscess/sinus, fluid drainage, and midline skin pits. They concluded from this case study if one or more of those characteristic findings are absent, differential diagnoses of chordoma, perineural cyst, giant cell tumour, intra-osseous lipoma, or intradural Schwannoma should be investigated.
Honestly, if I were not a physical therapy tech when my coccyx started killing me 20 years ago, I am not sure I would have gone to the doctor right away. My boss called me out when I winced every time I sat down, and he sent me off to get an exam. The majority of patients are not blurting out specific details about buttock pain when they come for evaluation. Modesty prevails but does not always benefit a patient with persistent coccydynia. Thankfully I did not have a chordoma, but the pain was intense enough to bring me to tears, and it could have required surgery if I had not been diagnosed early enough. Providing a comfortable environment for our patients during their initial encounter can help them feel less vulnerable and discuss the root of their pain. If we can decipher between chordoma and other causes of coccydynia, we may strike a chord that saves a patient from a poor outcome.
The Herman & Wallace course "Coccyx Pain Evaluation & Treatment" is an excellent opportunity to learn new differential diagnosis techniques for coccyx pain patients. The next opportunity to attend this course is March 25-26 in Tampa, Florida.
Blocker, O., Hill, S., & Woodacre, T. (2011). Persistent coccydynia – the importance of a differential diagnosis. BMJ Case Reports, 2011, bcr0620114408. http://doi.org/10.1136/bcr.06.2011.4408
Gavriilidis, P., & Kyriakou, D. (2013). Sacrococcygeal chordoma, a rare cause of coccygodynia. The American Journal of Case Reports, 14, 548–550. http://doi.org/10.12659/AJCR.889688
By accepting you will be accessing a service provided by a third-party external to https://www.hermanwallace.com/



































