To episiotomy or not to episiotomy?
Episiotomy is defined as an incision in the perineum and vagina to allow for sufficient clearance during birth. The concept of episiotomy with vaginal birth has been used since the mid to late 1700’s and started to become more popular in the United States in the early 1900’s. Episiotomy was routinely used and very common in approximately 25% of all vaginal births in the United States in 2004. However, in 2006, the American Congress of Obstetricians and Gynecologists recommended against use of routine episiotomies due to the increased risk of perineal laceration injuries, incontinence, and pelvic pain. With this being said, there is much debate about their use and if there is any need at all to complete episiotomy with vaginal birth.
 What are the negative outcomes of episiotomy?
What are the negative outcomes of episiotomy?
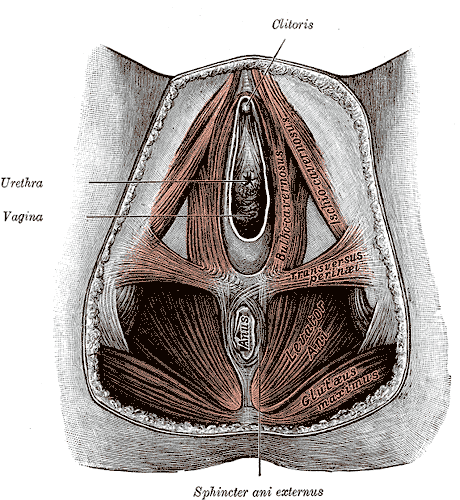
The primary risks are severe perineal laceration injuries, bowel or bladder incontinence, pelvic floor muscle dysfunction, pelvic pain, dyspareunia, and pelvic floor laxity. Use of a midline episiotomy and use of forceps are associated with severe perineal laceration injury. However, mediolateral episiotomies have been indicated as an independent risk factor for 3rd and 4th degree perineal tears. If episiotomy is used, research indicates that a correctly angled (60 degrees from midline) mediolateral incision is preferred to protect from tearing into the external anal sphincter, and potentially increasing likelihood for anal incontinence.
What are the indications for episiotomy, if any?
This remains controversial. Some argue that episiotomies may be necessary to facilitate difficult child birth situations or to avoid severe maternal lacerations. Examples of when episiotomy may be used could include shoulder dystocia (a dangerous childbirth emergency where the head is delivered but the anterior shoulder is unable to pass by the pubic symphysis and can result in fetal demise.), rigid perineum, prolonged second stage of delivery with non reassuring fetal heart rate, and instrumented delivery.
On the other side of the fence, many advocate never using an episiotomy due to the previously stated outcomes leading to perineal and pelvic floor morbidity. In a recent cohort study in 2015 by Amorim et al., the question of “is it possible to never perform episiotomy with vaginal birth?” was explored. 400 women who had vaginal deliveries were assessed following birth for perineum condition and care satisfaction. During the birth there was a strict no episiotomy policy and Valsalva, direct pushing, and fundal pressure were avoided, and perineal massage and warm compresses were used. In this study there were no women who sustained 3rd or 4th degree perineal tears and 56% of the women had completely intact perineum. 96% of the women in the study responded that they were satisfied or very satisfied with their care. The authors concluded that it is possible to reach a rate of no episiotomies needed, which could result in reduced need for suturing, decreased severe perineal lacerations, and a high frequency of intact perineum’s following vaginal delivery.
Are episiotomies actually being performed less routinely since the 2006 American Congress of Obstetricians and Gynecologists recommendation?
Yes, a recent study in the Journal of the American Medical Association by Friedman, it showed that the routine use of episiotomy with vaginal birth has declined over time likely reflecting an adoption of the American Congress of Obstetricians and Gynecologists recommendations. This is ideal, as it remains well established that episiotomy should not be used routinely. However, indications for episiotomy use remain to be established. Currently, physicians use clinical judgement to decide if episiotomy is indicated in specific fetal-maternal situations. If one does receive an episiotomy then a mediolateral incision is preferred. The World Health Organization’s stance is that an acceptable global rate for the use of episiotomy is 10% or less of vaginal births. So the question still remains, (and of course more research is needed) to episiotomy or not to episiotomy?
Amorim, M. M., Franca-Neto, A. H., Leal, N. V., Melo, F. O., Maia, S. B., & Alves, J. N. (2014). Is It Possible to Never Perform Episiotomy During Vaginal Delivery?. Obstetrics & Gynecology, 123, 38S.
Friedman, A. M., Ananth, C. V., Prendergast, E., D’Alton, M. E., & Wright, J. D. (2015). Variation in and Factors Associated With Use of Episiotomy. JAMA, 313(2), 197-199.
Levine, E. M., Bannon, K., Fernandez, C. M., & Locher, S. (2015). Impact of Episiotomy at Vaginal Delivery. J Preg Child Health, 2(181), 2.
Melo, I., Katz, L., Coutinho, I., & Amorim, M. M. (2014). Selective episiotomy vs. implementation of a non episiotomy protocol: a randomized clinical trial. Reproductive health, 11(1), 66.
By accepting you will be accessing a service provided by a third-party external to https://www.hermanwallace.com/





































