

Hi, I’m Deb Gulbranson, co-creator of the course Osteoporosis Management: An Introductory Course for Healthcare Professionals. Along with my partner, Frank Ciuba, we have created a program based on the works of Sara Meeks, whom we taught with for many years.
We know that posture is important, and we may include it in our evaluations, but how do we objectively measure it? How much time do we spend on education, training, exercises, and return demonstration? Chances are, not as much as we should.
Optimal alignment affects our breathing, balance, efficiency of gait, digestion, AND bone density.

Ask anyone on the street what one should do for osteoporosis and the typical answer is weight-bearing exercises - and they would be partially right. Weight-bearing, or loading, activities have been shown to increase bone density.(1) But that’s not the whole story. Different exercises have different strain magnitudes, strain rates, and strain frequencies - all of which impact bone density.
- Strain Magnitude - the force or impact of the exercise. Exercises such as gymnastics and weightlifting have a high strain magnitude.
- Strain Rate - the rate of impact of the exercise. Exercises such as jumping or plyometrics have a high strain rate.
- Strain Frequency - the frequency of impact during the exercise session. Exercises such as running have a high strain frequency.
When considering weight-bearing exercises for a home exercise program, the million-dollar question is, “How much weight-bearing is enough to stimulate bone growth, and how much is too much to compromise bone at risk for a fracture?” We know that there are incidents of individuals fracturing from just their body weight upon standing. Recently patients have been asking about heel drops and stomping, and whether they should do them. One size does not fit all.
An alternative is to focus on odd impact loading. A study by Nikander et a (2) targeted female athletes in a variety of sports classified by the type of loading they apparently produce at the hip region; that is, high-impact loading (volleyball, hurdling), odd-impact loading (squash-playing, soccer, speed-skating, step aerobics), high magnitude loading (weightlifting), low-impact loading (orienteering, cross-country skiing), and non-impact loading (swimming, cycling). The results showed that high impact and odd impact loading sports were associated with the highest bone mineral density.
When thinking of the Developmental Sequence (Supine, Side-lying, Prone, Quadruped, Tall Kneeling, Half-kneeling, Standing, and Walking), I used to think of either pediatrics or people with strokes. However, the developmental sequence can be very useful from an orthopedic standpoint specifically with osteoporosis patients.
We know that sitting is the most compressive position for our spines, yet repeatedly, I see physical therapists start exercise programs in sitting. There are several reasons I’d like you to consider starting patients in supine.
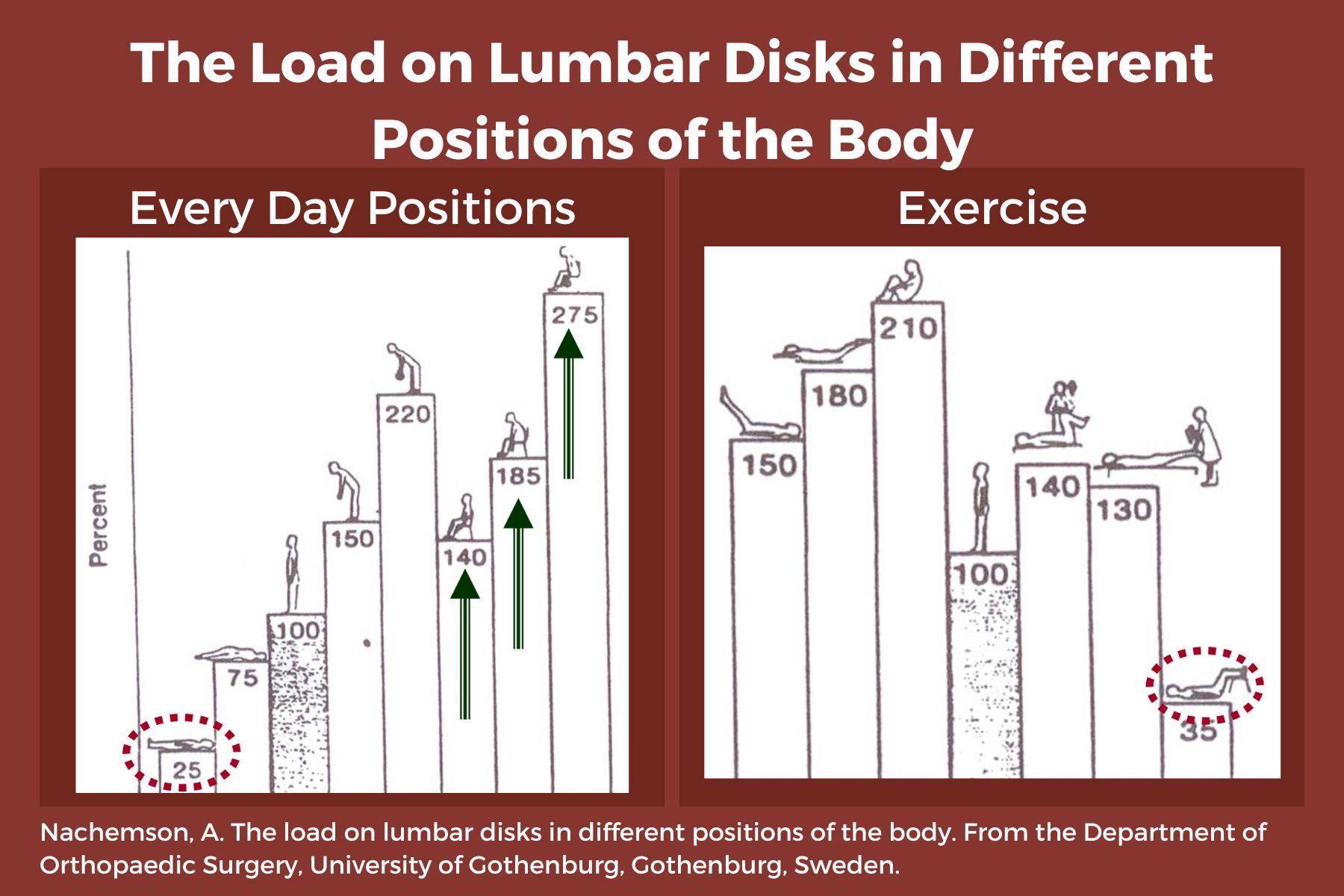
- Sitting increases intradiscal pressure. (1)
- Supine is a restful position, allowing tense muscles to relax, and can be a great way to reduce anxiety and cortisol running through the body. Ensure that the patient is propped with knees flexed or pillows under the knees, and forearms supported if there is tightness in the biceps.
- Patients can now concentrate on their breath, become aware of any “holding patterns” of tension throughout their body, and free up the mind to focus on learning new skills.
- When we are in higher levels of positioning-sitting, standing, or walking, our brain is focused on survival such as “not falling”. We have many more muscles and joints to control - ankles, knees, hips, etc. This reduces our ability to focus on learning new skills such as engaging the core muscles, relaxing the neck, stop clenching the fingers, etc.
- Preparation is key. We must help our patients gain mastery at one level and then move to the next. Once a patient can understand and find a neutral spine in prone, they are ready to move to side-lying.
- Side-lying can be very beneficial in teaching neutral spine because side-lying is “discombobulating.” We get lost in space and default to the fetal position - a flexed, contra-indicated posture for people with osteoporosis. Use a dowel rod or broom handle to provide feedback from the occiput to the mid-thoracic spine to the sacrum. Have your patient straighten their knees and hips so that, “If you were lying with your back against an imaginary wall, the back of your head, upper back, sacrum, and heels would touch the wall.”
- Prone: Not every osteoporosis patient you see will be able to ultimately transition to prone, but a high majority can and should. Again, propping is critical to allow any anatomical limitations such as shoulder tightness. Use a pillow longitudinally rather than transversely across the abdomen to elevate the shoulders so they can flex to allow the forehead on the hands. If not, keep arms by their side and provide a towel roll under the forehead. This position requires several “stages” of advancement over time and education to engage transversus abdominus, especially for those with spinal stenosis and/or tight hip flexors. The feet should be off the edge of the bed to allow for tightness in plantarflexion.
Working with patients in these three basic positions, while focusing on intercostal breathing, muscle relaxation of the neck, fingers, and other compensatory patterns as we move up the chain, builds a foundation to prepare for functional activities of sit-to-stand, static standing, and movement. These are not stepping stones to be skipped in order to jump into the higher-level functional activities. You would not build a house without a firm foundation. Make sure your patient has the building blocks necessary for the best possible outcomes.
Please join Frank Ciuba and me for our upcoming remote course: Osteoporosis Management: An Introductory Course for Healthcare Professionals on Saturday, Nov 2, 2024. We will discuss osteoporosis-safe exercises, balance and gait activities, and additional ways to help your patients build a strong foundation for movement competence!
Reference:
- Comparison of In Vivo Intradiscal Pressure between Sitting and Standing in Human Lumbar Spine: A Systematic Review and Meta-Analysis. Journal ListLife (Basel) PMC8950176 Jia-Qi Li,1 Wai-Hang Kwong,1,* Yuk-Lam Chan,1 and Masato Kawabata2
AUTHOR BIO:
Deb Gulbrandson, PT, DPT
 Deb Gulbrandson, DPT has been a physical therapist for over 49 years with experience in acute care, home health, pediatrics, geriatrics, sports medicine, and consulting to business and industry. She owned a private practice for 27 years in the Chicago area specializing in orthopedics and Pilates. 5 years ago, Deb and her husband “semi-retired” to Evergreen, Colorado where she works part-time for a hospice and home-care agency, sees private patients as well as Pilates clients in her home studio and teaches Osteoporosis courses for Herman & Wallace. In her spare time, she skis and is busy checking off her Bucket List of visiting every national park in the country- currently 46 out of 63 and counting.
Deb Gulbrandson, DPT has been a physical therapist for over 49 years with experience in acute care, home health, pediatrics, geriatrics, sports medicine, and consulting to business and industry. She owned a private practice for 27 years in the Chicago area specializing in orthopedics and Pilates. 5 years ago, Deb and her husband “semi-retired” to Evergreen, Colorado where she works part-time for a hospice and home-care agency, sees private patients as well as Pilates clients in her home studio and teaches Osteoporosis courses for Herman & Wallace. In her spare time, she skis and is busy checking off her Bucket List of visiting every national park in the country- currently 46 out of 63 and counting.
Deb is a graduate of Indiana University and a former NCAA athlete where she competed on the IU Gymnastics team. She has always been interested in movement and function and is grateful to combine her skills as a PT and Pilates instructor. She has been certified through Polestar Pilates since 2005, a Certified Osteoporosis Exercise Specialist through the Meeks Method since 2008, and a Certified Exercise Expert for the Aging Adult through the Geriatric Section of the APTA.

Movement competence (or Movement Literacy) is defined as the development of sufficient skills to ensure successful performance in different physical activities. Often used in the world of sports and youth, it also applies to our everyday activities. For example, standing up from a chair or toilet, getting in/out of a car, moving our body from Point A to Point B (and the difference between the ground being even and dry vs uneven and icy).
In our course, Osteoporosis Management: An Introductory Course for Healthcare Professionals, Dr Frank Ciuba and I approach the starting point for individuals with low bone mass (osteopenia or osteoporosis), from an “optimal alignment position.” Patients start supine with hips and knees flexed and are educated on what optimal alignment feels like. Many need to be propped using pillows, towels, or blocks behind their heads, forearms, or between their knees to achieve “their optimal alignment.” Breathing and awareness play a huge role in activating core musculature to sustain this alignment when moving to a vertical position such as sitting or standing. In vertical, our weight-bearing forces and gravity should pass down through the skeleton to take advantage of bone-building benefits. We use dowel rods, broom handles, and walls to give feedback. Optimal alignment can and should be taught in a variety of positions: side-lying, prone, hands and knees, ½ kneeling as we move up the developmental chain.
Hip Hinging, a well-known concept by therapists, must be practiced and mastered for patients with low bone mass to reduce the risk of vertebral fractures. Activities that involve bending at the waist such as brushing teeth, making a bed, and putting dishes in the dishwasher all place the anterior portion of the vertebral bodies under pressure and increase fracture risk.

For the past 20 of my 49 years as a physical therapist, I have been focusing on osteoporosis management thanks to the intervention of Sara Meeks who began studying osteoporosis in the 1980s before it was even a “thing.” The WHO did not identify osteoporosis as a systemic disease until 1993! About 15 years ago, after attending all of Sara’s Osteoporosis seminars, she selected my current business partner, Frank Ciuba, and I to “carry the torch.” Since then, we have been teaching her course with updated evidence, additions, and new research as it becomes available.
According to the Bone Health and Osteoporosis Foundation, 50% of individuals over age 50 are diagnosed with low bone density (osteopenia or osteoporosis) and many assume the only therapy option is medication.
Not so fast!

Deb Gulbrandson, PT, DPT has been a physical therapist for over 42 years with experience in acute care, home health, pediatrics, geriatrics, sports medicine, and consulting to business and industry. Dr. Gulbrandson frequently presents community talks on topics related to Osteoporosis and safe ways to develop Core Strength. She is a member of the APTA Geriatric and Private Practice Sections, a Certified Osteoporosis Exercise Specialist using the Meeks Method, and is a CEEAA (Certified Exercise Expert for the Aging Adult) through the Geriatric Section of the APTA.
Hello, my name is Deb Gulbrandson. May is National Osteoporosis Month, and my colleague, Frank Ciuba, and I are creators of the upcoming remote course Osteoporosis Management on June 12-13, 2021.
Did you know that approximately half of all women and a quarter of all men will break a bone due to osteoporosis? Equally disheartening, every year about one-third of adults in the US age 65 and older will fall. Many of these falls will result in broken bones.
Deb Gulbrandson, PT, DPT, along with Frank J Ciuba DPT, MS, is the author and instructor for a new course on osteoporisis that is launching remotely this month. Join Deb in Osteoporosis Management: A Comprehensive Approach for Healthcare Professionals!
Osteoporosis is a disease of increasingly porous bones that are at greater risk for fracture. The normal “bone remodeling” of breaking down and building up bone as we age is out of balance. Similar to a bank account with withdrawals outpacing deposits, as time goes on there is more breaking down than building back up. This leaves the bone more vulnerable for fracture.
We tend to think of Osteoporosis as an old person’s disease and in fact age is certainly a risk factor. We see a sharp decline in bone density the first few years following menopause; a withdrawal from the “bone bank account.” But let me share a startling statistic. At the age of 20 we have 98% of the bone density we will ever achieve. We achieve Peak Bone Mass by age thirty when our bones have reached their maximum strength and density.
Deb Gulbrandson, PT, DPT is teaming up with Frank J Ciuba DPT, MS to create a new course called Osteoporosis Management: A Comprehensive Approach for Healthcare Professionals! This new course is launching remotely this July 25-26, 2020, and it emphasizes visual imagery cues which leads to enhanced performance for patients. Both course authors are trained by Sara Meeks, and have adapted her method to create this updated, evidence-based course on osteoporosis management.
How many times have you told your patients to stand up straight and stop looking down while walking? How’d that work out? Probably not so good. At best you may have noticed a temporary correction only for the patient to return to the formerly mentioned poor posture. We know that balance is affected by alignment of our trunk and spine. 1 Everyone needs to avoid falls but it’s particularly important with osteoporosis patients due to bone fragility.
We want our patients not only to move, but to move with optimal alignment. According to Fritz, et al 2 in the vhitepaper: “Walking Speed: The Sixth Vital Sign”, walking is a complex functional activity. Our ability to influence motor control, muscle performance, sensory and perceptual function, endurance and habitual activity level can result in a more efficient and safer gait.
Osteoporosis or low bone mass is much more common than most people realize. Approximately 1 in 2 women over the age of 50 will suffer a fragility fracture in their lifetime. A fragility fracture is identified as a fracture due to a fall from a standing height. According to the US Census Bureau there are 72 million baby boomers (age 51-72) in 2019. Currently over 10 million Americans have osteoporosis and 44 million have low bone mass.
Many myths abound regarding osteoporosis. Answer these 5 questions below to test your Osteoporosis IQ. 1
1. “Men don’t get osteoporosis.”
Fact: In addition to the statistic above regarding the incidence of fractures in women, up to 1 in 4 men over the age of 50 will suffer a fragility fracture.
Do you work with osteoporosis patients? This may be a trick question because you probably do whether you know it or not- even if you are a pediatric therapist! Osteoporosis is defined by the World Health Organization1 as a systematic skeletal disease characterized by:
- Low bone mass
- Micro-architectural deterioration of bone tissue
- Consequent increase in bone fragility and susceptibility to a fracture
Osteoporosis occurs in men, women and even children. It is sometimes called the “silent disease” because often people don’t know they have it until they break a bone. And even then, compression fractures are painful only 20-30% of the time. Old fractures are often found on x-rays when a person is imaged for illnesses such as pneumonia. According to the National Osteoporosis Foundation2, about one in two women and one in four men over the age of 50 will suffer a fracture due to bone fragility. At this point in time, it is estimated 80% of patients entering Emergency Departments with a fragility fracture (a fall from a standing height) are never followed up for care.
As therapists, we see patients for a variety of diagnoses with co-morbidities but osteoporosis may not be listed. This could be because they have never been identified. We are in a prime position to screen for signs associated with the disorder. Below are the top 3 signs to look for:



































