



Since its launch in the beginning of 2024, Modalities for Pelvic Function has only continued to grow. The cool thing about this class is that although the curriculum content stays mostly the same, there are always amazing products for pelvic health being released and discovered by the curriculum team. Our next class offering is in July of 2025 and we’re adding at least 3 new products to the class. Enjoy our introduction to them in the order they will appear in our course work!
New to the Myofascial Techniques Lab - The BAligned Bowtie
The BAlign® Bowtie by TheraTrain is a therapy tool designed by Dr. Jaime Loomis, a Doctor of Physical Therapy, to promote spinal alignment and alleviate musculoskeletal discomfort. The BAlign Bowtie is a compact, hard rubber device shaped like two connected ovals. Dr. Jamie gives tips on where to place it, usually the base of the spine or pelvis, and then the client lies on it for a few minutes to help realign the spine and relieve pain. This tool is particularly beneficial for individuals experiencing low back pain, hip tightness, or asymmetrical posture. It's also been reported to aid in conditions like scoliosis and improve mobility in activities such as golf and running.
I had the privilege of meeting with Dr. Jamie to talk about her product, and she gave me the insider scoop on it. This product can be used for pelvic alignment, but can also be used higher up in the spine to help with asymmetry and pain. I personally love a multifaceted tool for investment and creative purposes! She created this tool to save time in therapy sessions. Dr. Jamie noticed that patients with pelvic and shoulder asymmetries would have improvement with their alignment and pain in therapy, but then be back to baseline by their next session. She’d have to spend time in their session repeating previous work to realign things again. She found that with this tool, her patients could have something actionable at home and their return sessions in alignment and were able to focus on other areas of therapy such as strength, function, and mobility.


When we think of pelvic floor dysfunction, our minds often go straight to adults. We may even consider toddlers or children struggling with conditions like constipation or bedwetting. A population I frequently find missed is the infant! Many providers don’t realize that the pelvic floor issues that show up in infancy don’t have to be waited out.
As pediatric pelvic health providers, we have a unique and powerful role to play in helping babies who struggle with common challenges like reflux, colic, constipation, feeding difficulties, and even motor delays. At the root of many of these concerns lies the pelvic floor—an area often overlooked in traditional pediatric care. These parents will go to their providers, and they’ll be offered advice like “hold them upright for 20 minutes after feeding” or “try a lactation consultation,” but what happens if these interventions are not enough, OR what happens if a rehab provider wants to provide more support to a struggling family.
You may be thinking, “I don’t do pediatrics.” If that is your stance, I recommend you keep reading. You don’t have to be a dedicated pediatric therapist to provide families struggling with cranky or uncomfortable babies. Even if you don’t want to provide specific recommendations and treatment, you can still screen and offer referrals for support and even this step will create improvement in the quality of life of your families.
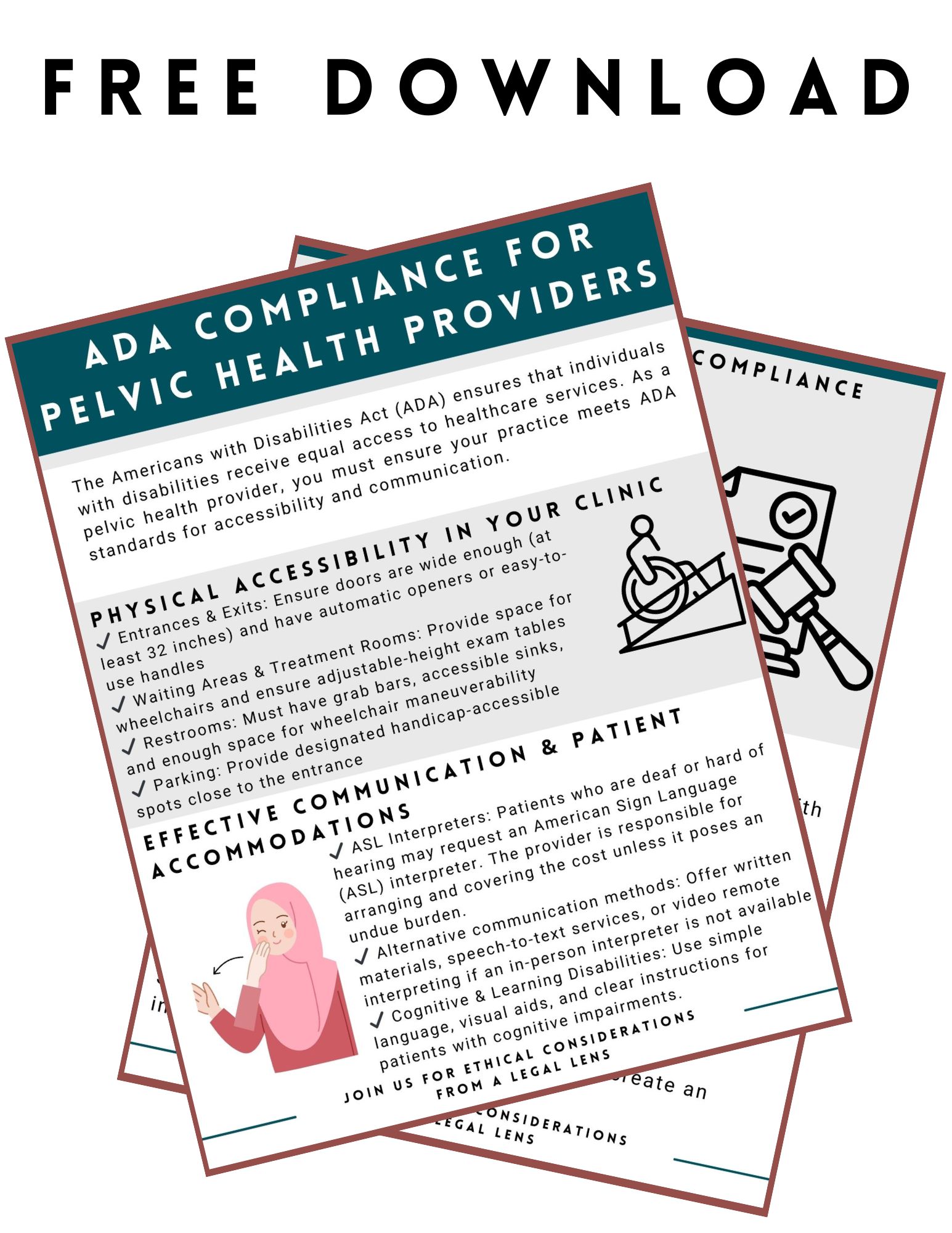

What do you know about the Americans with Disabilities Act (ADA)? You may be thinking that you are a pelvic health provider, so you don’t need to worry about laws, rules, and regulations. You may need to know more about the ADA than you thought.
Scenario: Your patient calls and requests an American Sign Language interpreter during their pelvic health evaluation. You don’t know much about this. You start to research online, and here is what you find…
Google search answer: “Yes, under the Americans with Disabilities Act (ADA), if your practice is a place of public accommodation (e.g., a healthcare provider), you are generally required to provide effective communication, which may include an ASL interpreter when necessary. However, the law considers "undue burden," meaning if the cost is too high relative to your resources, alternative accommodations (like written communication or remote video interpreting) may be acceptable. You cannot charge the patient for the interpreter.”

As I cruise through online Facebook Pelvic Health Mentorship Groups - a weird bedtime passtime that brings me more satisfaction than doom scrolling on TikTok - I hear many providers worried about getting in trouble for patient abandonment. As rehab providers, we have worked hard to get our education, licensure, jobs, and clients that trust us, so it makes sense there would be a fear of losing any of all of those things.
When this concern comes up, I just want to reassure providers and also let them know that there are three continuing education classes in the Herman & Wallace curriculum tailor-made to address other ethical questions and concerns pelvic rehabilitation providers may have:
- Ethical Considerations from a Legal Lens - Scheduled for April 12th
- Ethical Considerations for Pediatric Pelvic Health - Scheduled for July 27th
- Ethical Concerns for Pelvic Health Professionals - Next date TBD
What is patient abandonment? Patient abandonment is a failure of the provider to fulfill their duty of care, leaving a patient without necessary medical support at a critical time. Unlike a patient voluntarily discontinuing care or being referred to another provider, abandonment involves a lack of appropriate communication or planning.

I’ve been “on the record saying” I used to be a modalities skeptic. I didn’t think I used them a ton in my practice and when I switched from a big hospital system to my own private practice, I didn’t have access to the larger equipment machines like the big ultrasound or biofeedback devices.
I have, however, always been a fan of gadgets and tools as a pelvic health provider. For anyone who has ever been to a class where I was a teaching assistant, you’ve likely seen me literally roll in with a giant suitcase full of example things - models, pelvic trainers, examples of belts, braces, dilators, wands, weights, lube samples, pelvic organ stuffies etc. I always called it my toolkit and so many of my peers had this as well. When the Content & Curriculum team asked me to be on the team for writing for this project, I was initially unsure. I didn’t think I used modalities enough or valued them enough to create a two-day course on the topic.
Long story short…I was wrong. What I have learned is I was very wrong, and I use them constantly.

One of the things you'll learn when working with the pediatric population is that they're a different species than adults. Some of the common diagnoses may overlap, such as chronic constipation, fecal smearing, or nocturia. The way they present may be similar and the treatment ideas and philosophy may also overlap. However, how these treatments are implemented may vary when treating a child versus an adult. When I think of treating the pediatric population, I like to divide my thought process and approach into five different groups.
To me, pediatrics can be babies/infants, toddlers, preschool-aged children, elementary school-aged children, and then tweens/teens. It may feel excessive to divide this population into so many subgroups, but each of those groups has its own treatment considerations based on the child's development at that time in their lives. An infant may be working on regulating their GI system as they transition from being in-utero to being born. Toddlers and school-aged children are working through various internal and social benchmarks to help them continue to grow and develop. Likewise, a tween or teen may be managing the changes to their genitourinary system as they work through puberty towards adulthood or grappling with their sexuality and sexual identity as they mature.
Regardless of what stage they are in life, patients will potentially present differently and also need a customized treatment plan to meet them where they are at. When I have colleagues jumping into pediatric pelvic health, I rarely worry they have the clinical skills to help with the physical and physiological challenges a child may face. The place I see many clinicians struggle is how to apply the skills they know to these tiny humans in front of them. Treating reflux in an eighty-year-old versus an 8-week old person is very different.
Rehabilitation providers experience ethical conflicts every day, whether they realize it or not. Just today, I was cruising through social media on my lunch break and saw a post (edited for autonomy) that posed an ethical concern, potentially without its author even knowing. We’ll refer back to this post throughout the blog so please read:
“We have a patient at my clinic whose partner called and scheduled the appointment for the patient. My colleague did the evaluation this morning and said the partner answered all questions for the patient. The partner was inquiring about decreasing posterior pelvic floor tension for anal sex. The therapist found it strange that the partner was answering all the questions for the patient. At this time, I'm really wondering if the partner is forcing the patient to come to pelvic floor therapy and participate. How would you all handle this situation?”
You know this stopped my scroll immediately. Yes, it is a patient care question. However, this situation also brings up so many other intricacies that we encounter as pelvic health providers. I gave my reply and then read others, and this experience made me glad that Herman and Wallace offered three ethics classes talking about ethics for pelvic floor therapists to attend and be able to collaborate on issues just like the one above.

As a healthcare professional, staying informed about ethical and legal responsibilities is not just a requirement, but a crucial aspect of providing the best care for your patients. I instruct a remote course that tackles these difficult issues - my course, Ethical Considerations from a Legal Lens is a comprehensive remote course taking place on November 17, 2024, that will delve into these important topics from the perspective of the pelvic health rehabilitation field.
Why does this topic matter?
Navigating the complex legal and ethical landscape can be challenging for healthcare providers, particularly in specialized areas like pelvic rehabilitation or even more niche subsets within pelvic health. This course is designed to help practitioners gain a deeper understanding of ethical decision-making while helping a provider feel more legal compliance to safeguard the patient’s well-being and the integrity of a provider’s practice.
During this course, you’ll interactively explore key concepts including:

Each profession has its own code of ethics to give guidelines for the professional to act. This is the case for lawyers, doctors, mental health therapists, massage therapists, and accountants to name a few. In pelvic rehabilitation, the APTA and AOTA make different guidelines for physical therapists and occupational therapists respectively.
For physical therapists, the Code of Ethics is built upon the physical therapist's five roles, the profession's core values, and the multiple realms of ethical action. For occupational therapists, the code serves the two purposes of providing aspiration core values in professional and volunteer roles as well as delineating ethical principles and enforceable standards of conduct.
There are many areas of overlap and differences between the roles of physical and occupational therapists in pelvic rehabilitation. This blog will explore the areas that overlap in the world of ethical decision-making. Pelvic floor therapists must complete tasks such as management of patients/clients, consultation, education, research, and administration. Ethical realms can be individual, organizational, and societal and there are various situations an individual can find themselves in when providing care including problems, issues, dilemmas, temptation, distress, and silence.

September is Ovarian Cancer Awareness Month. Ovarian cancer is the seventh most common type of malignant neoplasm in women and the eighth cause of mortality for women (Gaona-Luviano et al, 2020). In women who have died from gynecological cancers, ovarian cancer is the leading cause of death (Arora et al., 2021). This type of cancer can originate from any of the ovary's three main components, including the epithelium, stroma, and germinal cells. Per Gaona-Luviano et al., 2020, “epidemiology of this cancer shows differences between races and countries due to several factors including genetic and economic.” Detection of ovarian cancer is problematic because there is no standardized screening process and most cases of ovarian cancer are found in the advanced stages (Gaona-Luviano et al, 2020).
How is ovarian cancer diagnosed?
Sadly, the existing screening tests have a low predictive value. A gynecological evaluation, transvaginal ultrasound, and tumor marker testing (cancer antigen-125/CA-125 assay) can help with early detection strategies but this has not shown a significant effect on the morbidity or mortality of this cancer (Arora et al., 2021).
How is ovarian cancer treated medically?



































