In the United States, estimated direct medical costs for outpatient visits for chronic pelvic pain (CPP) is more than $2.8 billion per year.1 In a 2017 study in the Clinical Journal of Pain by Sanses et al, a detailed musculoskeletal exam of clients with CPP can assist both physicians as well as physical therapists in differential diagnosis and appropriate referrals for this population.
Evaluating a client with pelvic pain requires a skill set that includes direct pelvic floor as well as musculoskeletal test item clusters. The prioritization of which depends upon many factors including clinician discipline, experience, specialty vs. general setting, as well as client history, presentation and goals. In addition to the direct pelvic floor assessment, there are additional key musculoskeletal screening tests that are an essential part of a pelvic pain assessment. New this year, my course Finding the Driver in Pelvic Pain will incorporate the use of Real Time Ultrasound in neuromuscular assessment and re-education of the pelvic floor and abdominal wall during the Sunday morning lab session.
Peery et al (2012) noted that abdominal pain was one of the most common presenting reasons for an outpatient physician visit in the United States. Abdominal pain is one of the many complaints that our clients may report requiring differential diagnosis including urogynecologic, colorectal, musculoskeletal, visceral or neurogenic causes. Lower abdominal quadrant pain may denote serious emergent pathology. Clinical findings, physical exam and client symptoms in addition to smart differential diagnosis must be used to determine if the abdominal pain is musculoskeletal in nature. Direct access requires physical therapists to perform a skilled initial screening for abdominal pain in order to determine if it is abdominal wall versus a visceral origin. Physicians are fluent in ruling out emergent pathology but may not be familiar with musculoskeletal tests for non-emergent pathology. Assessment of bowel and bladder function and habits are essential to perform. This blog specifically addresses three physical exam tests that can be performed as part of abdominal wall pain screening. According to Cartwright et al, the location of the abdominal pain should drive the evaluation.
Carnett’s test is a simple clinical test that assesses abdominal pain response when a client tenses their abdominal muscles. A positive Carnett’s sign denotes the origin of symptoms within the abdominal wall with a negative tests suggesting intra-abdominal pathology. The test is performed in supine, the clinician gently palpating the area of abdominal pain and has the client lift their head and shoulders off the table. Conditions such as myofascial trigger points, scar and muscular pain would be flared with palpation of the contractile tissue with activation of the abdominal wall muscles. If the pain is due to visceral origin, appendicitis for example, the pain would remain unchanged with palpation with head lift. Although some perform Carnett’s test by lifting both legs off the table, this method may cause unnecessary pain in clients with poor lumbopelvic control. (Figure 1) The head and shoulder lift option is felt to be comparable method of performing Carnett’s test.
Blumberg’s sign is most commonly used to rule in appendicitis, peritonitis or a visceral driver of right lower quadrant pain. The test is performed by the clinician applying deep pressure over McBurney’s point (Figure 2) with an abrupt and rapid release of pressure. Although there are anatomical variations in appendix location, pain reproduction is consistent with a positive test and immediate referral to the ER is indicated.
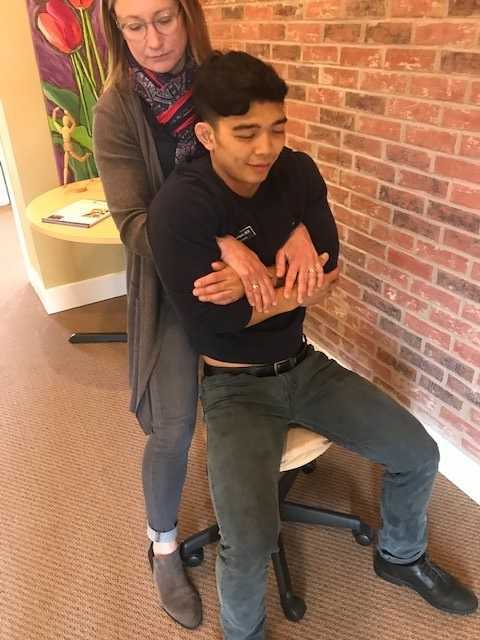
Thoracic dysfunction, including disc herniation, can result in abdominal pain.2 In thoracic discogenic driven abdominal pain, symptoms would likely be exacerbated by coughing, sneezing, spinal flexion and activities that would increase spinal loading. A simple screening for this is seated thoracic traction. If the client reports reduction or resolution of symptoms with traction, further musculoskeletal tests including regional movement and PIVM testing could be implemented to rule in or rule out need for diagnostic imaging.
In the Herman Wallace course “Finding the Driver in Pelvic Pain” participants learn a comprehensive musculoskeletal screen including abdominal, neural mobility and conductivity, pelvic ring, pelvic floor and biomechanical contributing factors to pelvic pain. Evidence based test item clusters are defined, along with their diagnostic accuracy, for all associated systems in order to outline a comprehensive screen for pelvic pain clients. To learn more about musculoskeletal screening for pelvic pain, check out faculty member Elizabeth Hampton PT, DPT, WCS, PRPC, BCB-PMD’s course Finding the Driver of Pelvic Pain, which is next offered Jun 28, 2019 - Jun 30, 2019 in Columbus, Ohio. We are fortunate to have Dick Poore, President of The Prometheus Group present on Sunday June 30th for technical support for the Real Time Ultrasound portion of the course.
1. Sanses et al. "The Pelvis and Beyond: Musculoskeletal Tender Points in Women with Chronic Pelvic Pain". Clin. J. Pain. 2016 Aug. doi: 10.1097/AJP.0000000000000307
2. Papadakos et al. "Thoracic Disc Prolapse Presenting with Abdominal Pain: Case Report and Review of the Literature". Ann. R. Coll. Surg. Engl. 20019 Jul. doi: 10.1308/147870809X401038