New Clinical Guidelines for Peyronie's Disease
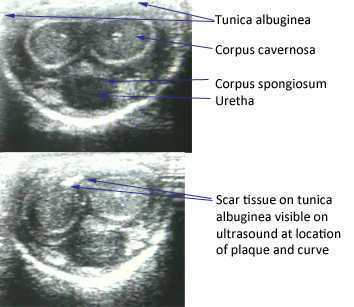
The American Urological Association issued new guidelines in May of this year for the diagnosis and treatment of Peyronie's. The disorder, which you can read more about at this link, often leads to a curvature in the penis that can be painful, or that can lead to impaired sexual or urinary function. While the exact mechanism leading to Peyronie's is still being researched, what is known is that plaques (sometimes calcified) may form in a deep layer of thick connective tissue called the tunica albuginea that surrounds the penis.
In the clinical guidelines, the authors state that a diagnostic process should include documentation of the signs and symptoms of Peyronie's disease. This can include a careful history (assessing any penile deformity, limitations in sexual function, penile pain, and level of distress). In the medical office, an intracavernosal injection (check here for a Medscape article describing an algorithm) can be completed. The authors also state, in line with expert opinion, that a provider should only evaluate a patient's Peyronie's disease when possessing "…the experience and diagnostic tools to appropriately evaluate, counsel, and treat the condition." In regards to pelvic rehabilitation, understanding the condition and encouraging the patient to visit a medical provider who is appropriately trained to manage Peyronie's is valuable. Establishing a baseline for the amount of dysfunction and curvature aids the patient and physician in determining current and future care planning.
Available treatments include education about possible treatments as well as adverse reactions to medical treatment. Interventions might include oral NSAIDs, intralesional injections (to reduce the amount of scar/thickened tissue or pain), and surgeries. Surgical options include procedures to remove the plaque or scar tissue, remodel the penile tissues after plaque removal, and for more severe cases, to implant a penile prosthesis. (Recommendations for treatments to avoid due to potential for harm or for lack of evidence are also listed in the article.)
The role of pelvic rehabilitation is emerging for men who present with genital pain, deformity, or pelvic dysfunction. There are certainly comorbid dysfunctions that we can address, such as pelvic muscle dysfunction, bowel and bladder issues if present, and we can provide a significant amount of education about pelvic health. Therapists are also teaching patients to perform connective tissue mobilization on the penile tissues, and some therapists are directing manual therapy, dry needling, and other modalities to the tissues. Rehabilitation lacks, at this time, compelling evidence to support direct treatment to the tissues, and hopefully that research will be seen in the near future. The authors of the new guidelines conclude that "…The most effective approach for a particular patient is best determined by the individual clinician and patient in the context of that patient’s history, values, and goals for treatment." This sounds to me like an effective approach for every patient who struggles with a condition that lacks a clear understanding of etiology and best treatments. These guidelines are a step forward in management of patients who deal with the frustrating condition, and the guidelines will be updated, according to the article, as the science advances.
If you would like to learn more about the rehabilitation implications of Peyronie's, and the potential and current roles of therapists in male pelvic health, you have two opportunities this year to attend the Male Pelvic Floor course , August in Denver, and November in Seattle. We expect the Seattle to course to sell out, and it's filling up fast, so check your calendar and come join us at the Male course.
By accepting you will be accessing a service provided by a third-party external to https://www.hermanwallace.com/





































