In 2007, after only speaking on the phone and never meeting in person, my new friend and colleague Stacey Futterman and I presented at the APTA National Conference on the topic of male pelvic pain. It was a 3 hour lecture that Stacey had been asked to give, and she invited me to assist her upon recommendation of one of her dear friends who had heard me lecture. I still recall the frequent glances I made to match the person behind the voice I had heard for so many long phone calls.
 Upon recommendation of Holly Herman, we took this presentation and developed it into a 2 day continuing education course, creating lectures in male anatomy (we definitely did not learn about the epididymis in my graduate training), post-prostatectomy urinary incontinence, pelvic pain, and a bit about sexual health and dysfunction. Although it truly seems like the worst imaginable question, we asked each other “should we allow men to attend?” As strange as this question now seems, it speaks volumes about the world of pelvic health at that time; mostly female instructors taught mostly female participants about mostly female conditions.
Upon recommendation of Holly Herman, we took this presentation and developed it into a 2 day continuing education course, creating lectures in male anatomy (we definitely did not learn about the epididymis in my graduate training), post-prostatectomy urinary incontinence, pelvic pain, and a bit about sexual health and dysfunction. Although it truly seems like the worst imaginable question, we asked each other “should we allow men to attend?” As strange as this question now seems, it speaks volumes about the world of pelvic health at that time; mostly female instructors taught mostly female participants about mostly female conditions.
Make no mistake- women’s health topics were and are deserving of much attention in our typically male-centered world of medicine and research. Maternal health in the US is dreadful, and gone are the days when providers should allow urinary incontinence or painful sexual health to be “normal”, yet it is often described as such to women who are brave enough to ask for help. Times have changed for the better for us all.
The Male Pelvic Floor Course was first taught in 2008, and so far, 22 events have taken place in 18 different cities. 73 men have attended the course to date, with increasing numbers represented at each course. Rather than 20-25 attendees, the Institute is seeing more of the men’s health course filling up with 35-40 participants. In my observations, the men who attend the course are often very experienced, have excellent orthopedic and manual therapy skills, and have personalities that fit very well into the sensitive work that is pelvic rehabilitation.
The course was expanded to include 3 days of lectures and labs, and this expansion allowed more time for hands-on skills in examination and treatment. The schedule still covers bladder, prostate, sexual health and pelvic pain, and further discusses special topics like post-vasectomy syndrome, circumcision, and Peyronie’s disease. In my own clinical practice, learning to address penile injuries has allowed me to provide healing for conditions that are yet to appear in our journals and textbooks. As I often say in the course, we are creating male pelvic rehabilitation in real time.
Because the course often has providers in attendance who have not completed prior pelvic health training, instruction in basic techniques are included. For the experienced therapists, there are multiple lab “tracks” that offer intermediate to advanced skills that can be practiced in addition to the basic skills. Adaptations and models are used when needed to allow for draping, palpation, and education when working with partners in lab, and space is created for those therapists who want to learn genital palpation more thoroughly versus those who are deciding where their comfort zone is at the time. One of the more valuable conversations that we have in the course is how to create comfort and ease in when for most us, we were raised in a culture (and medical training) where palpation of the pelvis was not made comfortable. Hearing from the male participants about their bodies, how they are affected by cultural expectations, adds significant value as well.
We need to continue to create more coursework, more clinical training opportunities so that the representation of those treating male patients improves. If you feel ready to take your training to the next level in caring for male pelvic dysfunction, this year there are three opportunities to study. I hope you will join me in Male Pelvic Floor Function, Dysfunction and Treatment.
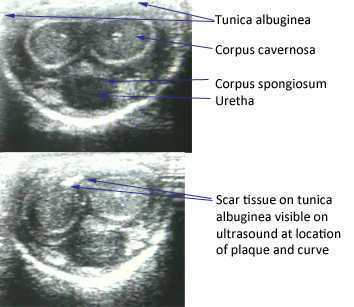
Peyronie’s disease is a condition in which there are fibrotic plaques (sometimes calcified) that can cause a curvature in the penis, most notable during erection. Pain as well as urinary and sexual dysfunction may occur with Peyronie's disease. Increased attention has been given in recent years to the relationship between male hormones, erectile dysfunction, and Peyronie's disease. According to the Mayo Clinic, testosterone, the predominant hormone affecting male physical characteristics, peaks during adolescence and early adulthood. Testosterone gradually decreases about 1% per year once a man reaches age 30-40. Some men experience symptoms from the decline in testosterone and these symptoms can include decreased sexual function, sleep disturbances changes in bone density and muscle bulk, as well as changes in cognition and depression. Because other factors and conditions can cause similar symptoms, patients with any of these changes should talk to their medical provider to rule out diabetes, thyroid dysfunction, depression, sleep apnea, and medication side effects, according to Mayo.
 In an article published in 2012, Iacono and colleagues studied the correlation between age, low testosterone, fibrosis of the cavernosal tissues, and erectile dysfunction. 47 patients diagnosed with erectile dysfunction (ED) were included, with 55% of the 47 men being older than age 65. Having increased fibrosis corresponded to having a positive Rigiscan test- meaning that a nocturnal test of penile rigidity demonstrated abnormal nighttime erections. Low levels of testosterone also corresponded to erectile dysfunction. (This is an open access article with full text available) Another published article agreed with the above in that low testosterone is associated with Peyronie’s disease and/or erectile dysfunction. The authors are cautious, however, in describing the association between the variables, as causation towards plaque formation characteristic of Peyronie’s is not known.
In an article published in 2012, Iacono and colleagues studied the correlation between age, low testosterone, fibrosis of the cavernosal tissues, and erectile dysfunction. 47 patients diagnosed with erectile dysfunction (ED) were included, with 55% of the 47 men being older than age 65. Having increased fibrosis corresponded to having a positive Rigiscan test- meaning that a nocturnal test of penile rigidity demonstrated abnormal nighttime erections. Low levels of testosterone also corresponded to erectile dysfunction. (This is an open access article with full text available) Another published article agreed with the above in that low testosterone is associated with Peyronie’s disease and/or erectile dysfunction. The authors are cautious, however, in describing the association between the variables, as causation towards plaque formation characteristic of Peyronie’s is not known.
The larger question about Peyronie’s disease is what a patient can do to improve the symptoms of the condition. Therapists who treat male patients are increasingly interested in this question, and many are working with their patients to address the known soft tissue dysfunction. Interventions may include teaching patients to perform soft tissue mobilizations and stretches to the restricted tissue, and educating the patient in what the available literature tells us about rehabilitation of this condition. Hopefully, as male pelvic rehabilitation continues to grow in popularity, more therapists will contribute case studies and participate in higher levels of research so that more men can add conservative care of Peyronie’s to their list of treatment options.
To learn more about what the literature tells us about Peyronie’s and other male pelvic rehabilitation conditions, the Male Pelvic Floor continuing education course is taking place in Seattle in November, and you won't want to miss it!
The American Urological Association issued new guidelines in May of this year for the diagnosis and treatment of Peyronie's. The disorder, which you can read more about at this link, often leads to a curvature in the penis that can be painful, or that can lead to impaired sexual or urinary function. While the exact mechanism leading to Peyronie's is still being researched, what is known is that plaques (sometimes calcified) may form in a deep layer of thick connective tissue called the tunica albuginea that surrounds the penis.
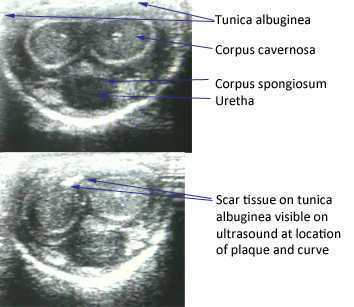
In the clinical guidelines, the authors state that a diagnostic process should include documentation of the signs and symptoms of Peyronie's disease. This can include a careful history (assessing any penile deformity, limitations in sexual function, penile pain, and level of distress). In the medical office, an intracavernosal injection (check here for a Medscape article describing an algorithm) can be completed. The authors also state, in line with expert opinion, that a provider should only evaluate a patient's Peyronie's disease when possessing "…the experience and diagnostic tools to appropriately evaluate, counsel, and treat the condition." In regards to pelvic rehabilitation, understanding the condition and encouraging the patient to visit a medical provider who is appropriately trained to manage Peyronie's is valuable. Establishing a baseline for the amount of dysfunction and curvature aids the patient and physician in determining current and future care planning.
Available treatments include education about possible treatments as well as adverse reactions to medical treatment. Interventions might include oral NSAIDs, intralesional injections (to reduce the amount of scar/thickened tissue or pain), and surgeries. Surgical options include procedures to remove the plaque or scar tissue, remodel the penile tissues after plaque removal, and for more severe cases, to implant a penile prosthesis. (Recommendations for treatments to avoid due to potential for harm or for lack of evidence are also listed in the article.)
The role of pelvic rehabilitation is emerging for men who present with genital pain, deformity, or pelvic dysfunction. There are certainly comorbid dysfunctions that we can address, such as pelvic muscle dysfunction, bowel and bladder issues if present, and we can provide a significant amount of education about pelvic health. Therapists are also teaching patients to perform connective tissue mobilization on the penile tissues, and some therapists are directing manual therapy, dry needling, and other modalities to the tissues. Rehabilitation lacks, at this time, compelling evidence to support direct treatment to the tissues, and hopefully that research will be seen in the near future. The authors of the new guidelines conclude that "…The most effective approach for a particular patient is best determined by the individual clinician and patient in the context of that patient’s history, values, and goals for treatment." This sounds to me like an effective approach for every patient who struggles with a condition that lacks a clear understanding of etiology and best treatments. These guidelines are a step forward in management of patients who deal with the frustrating condition, and the guidelines will be updated, according to the article, as the science advances.
If you would like to learn more about the rehabilitation implications of Peyronie's, and the potential and current roles of therapists in male pelvic health, you have two opportunities this year to attend the Male Pelvic Floor course , August in Denver, and November in Seattle. We expect the Seattle to course to sell out, and it's filling up fast, so check your calendar and come join us at the Male course.