“My butt hurts.” This is such a common subjective complaint in my practice as a manual therapist, and many patients insist it must be a muscle problem or jump to the conclusion it must be “sciatica.” I often tell patients if they did not get shot or bit directly in the buttocks, the pain is most likely referred from nerves that originate in the spine. Although blunt trauma to the buttocks can certainly be the culprit for pain in the gluteal region, a basic understanding of the neural contribution is essential for providing appropriate treatment and a sensible explanation for patients.
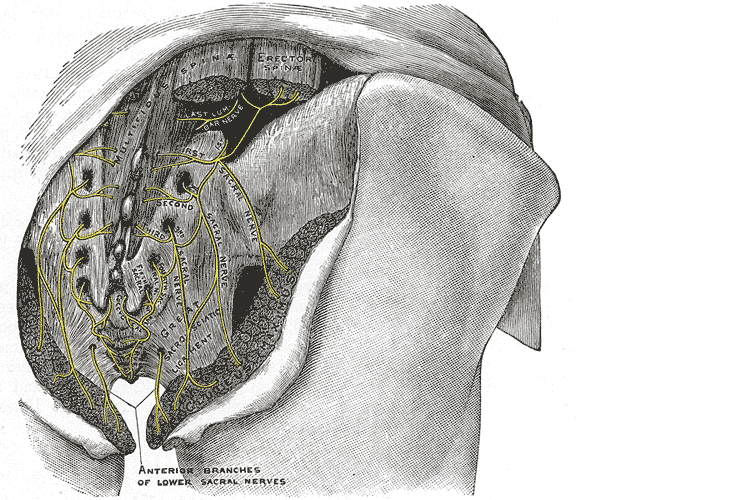
A publication by Lung and Lui (2018) describes the superior gluteal nerve. It comes from the dorsal (posterior) divisions of the L4, L5, and S1 nerve roots of the sacral plexus and innervates the gluteus medius, gluteus minimus, and tensor fasciae latae muscles. When this nerve is damaged or compressed, a Trendelenburg gait results because of paralysis of the gluteus medius muscle. The gluteus minimus and tensor fascia latae muscles are also innervated by the superior gluteal nerve and form the “abductor mechanism” together with the gluteus medius to stabilize the pelvis in midstance as the opposite leg is in swing phase. The superior gluteal nerve courses with the inferior gluteal nerve, sciatic nerve, and coccygeal plexus, but it is the only nerve to exit the greater sciatic foramen above the piriformis muscle.
Iwananga et al., (2018) presents a very recent article regarding the innervation of the piriformis muscle, which has been suspected to be the superior gluteal nerve, by dissecting each side from ten cadavers. Often the piriformis muscle can be compromised through total hip replacements with a posterior approach, hip injuries, or chronic pain disorders. This particular study verifies there is no singular nerve that innervates the piriformis muscle, and the most common innervation sources are the superior gluteal nerve (70% of the time) and the ventral rami of S1 (85% of the time) and S2 (70% of the time). The inferior gluteal nerve and the L5 ventral ramus were each found to be part of the innervation only 5% of the time.
Wang et al., (2018) focused on what causes gluteal pain with lumbar disc herniation, particularly at L4-5, L5-S1. They emphasize the important factor that dorsal nerve roots have sensory fibers and ventral roots contain motor neurons, and spinal nerves are mixed nerves, since they have ventral and dorsal roots. They discuss other contributing nerves, but continuing our focus on the superior gluteal nerve, it stems from L4-S1 ventral rami and not only allows movement of gluteus medius, gluteus minimus, and gluteus maximus, it also provides sensation to the area. This nerve can certainly produce pain in the gluteal region when irritated. In lumbar disc herniation of L4-5 or L5-S1, the ventral rami of L5 or S1 can be comprised or irritated at the level of the nerve root and provoke gluteal pain because they mediate sensation in that area.
Once the superior gluteal nerve (or any sacral nerve) is implicated as the root of pain, should we just shrug our shoulders and send them to pain management? I strongly suggest we learn how to address the issue in therapy using our hands with manual techniques and appropriate exercises. The Sacral Nerve Manual Assessment and Treatment course should be a priority on your bucket list of continuing education to help alleviate any further pain in the butt.
Lung K, Lui F. Anatomy, Abdomen and Pelvis, Superior Gluteal Nerve. [Updated 2018 Dec 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2018 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535408/
Iwanaga J, Eid S, Simonds E, Schumacher M, Loukas M, Tubbs RS. (2018). The Majority of Piriformis Muscles are Innervated by the Superior Gluteal Nerve. Clinical Anatomy. doi: 10.1002/ca.23311. [Epub ahead of print]
Wang, Y., Yang, J., Yan, Y., Zhang, L., Guo, C., Peng, Z., & Kong, Q. (2018). Possible pathogenic mechanism of gluteal pain in lumbar disc hernia. BMC musculoskeletal disorders, 19(1), 214. doi:10.1186/s12891-018-2147-y