An interview with Frank Ciuba.
Frank Ciuba, co-instructor of Osteoporosis Management< alongside Deb Gulbrandson, explains that practitioners need the information provided in their course. "This course is the latest up-to-date research compiled by my partner Deb Gulbrandson and myself in the management of osteoporosis for clinicians." He shares that similar to learning about the pelvic floor, "when physical therapists go to school they get only a small amount of what osteoporosis is and very little on how to treat a patient."
Frank explains that he became interested in teaching osteoporosis management when he learned "that one in four men statistically will get osteoporosis or an osteoporosis-related fracture in their lifetime and they're really not being identified." Osteoporosis Management provides an exercise-oriented approach to treating these patients and it covers specific tests for evaluation, appropriate safe exercises and dosing, basic nutrition, and ideas for marketing your osteoporosis program.
In pelvic health rehabilitation, it's seen that osteoporosis-related kyphosis (curvature of the spine) can affect pelvic organ prolapse, breathing, and digestion. Patients who go through the osteoporosis management program with Frank and Deb, are shown that they reduce the likelihood of compression fracture by 80%.
A different approach to treating prostatectomy patients.
The Pelvic Rehab Report sat down with Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC to discuss her upcoming courses Rehabilitative Ultrasound Imaging - Orthopedic Topics and Rehabilitative Ultrasound Imaging: Women's Health and Orthopedic Topics scheduled for November 12-14, 2021. Allison specializes in the treatment of the pelvic ring and back using manual therapy and ultrasound imaging for instruction in a stabilization program. She also specializes in women’s and men’s health including conditions of chronic pelvic pain, bowel and bladder disorders, and coccyx pain.
Proper breathing is discussed and taught in many ways and forms. All of this is a step in the right direction, but what if the person physically can not lengthen tissues to expand certain key structures that are essential to the breathing mechanism? In the remote course, Breathing and the Diaphragm, Aparna Rajagopal and Leeann Taptich teach different methods to identify breathing patterns, dysfunctional breathers, and how to determine motor control issues from mobility or strength issues.
Breath is utilized widely in the exercise world. Pilates uses breath for core stability. Yoga utilizes breath to help connect the body. Strength and conditioning coaches and personal trainers emphasize breath to provide power to lift. Breathing mechanics, aka proper breathing, is also core to any type of abdominal exercise.
Respiratory muscles are directly involved in these core abdominal strengthening, stability, and stretching exercises (1). Research led by DePalo, way back in 1985, concluded that the diaphragm is actively recruited during resistance exercises such as sit-ups (2). Inefficient breathing can lead to muscular imbalances, and motor control changes that can affect motor quality. Therapists are taught at length about tissue and joint mobility versus motor control or strength issues. These same principles can be applied to assess and treat the diaphragm, breathing, and abdominals.
Holly Tanner Short Interview Series - Episode 6 featuring Sandra Gallagher
In today’s interview, Sandra discusses some of the intricacies of working with transitioning patients, her path in working with the LGBTQ+ community, and her new course with H&W. Transgender Patients: Pelvic Health and Orthopedic Considerations is a remote course created by Sandra Gallagher and Caitlin Smigelski. This course provides specific content aimed at teaching pelvic health therapists how to expand their skills for working with people of all gender identities.
Sandra Gallagher has served on varied committees and boards at the state and national level, most recently as the chair of the CAPP-OBC committee for the Academy of Pelvic Health of the APTA. She has presented on the role of PT in gender-affirming vaginoplasty at UCSF Transgender Health Summit, APTA Combined Sections Meeting, and at the 2018 international meeting of the World Professional Association for Transgender Health (WPATH).
In a research study that Sandra facilitated with other colleagues, it was concluded that “Pelvic floor physical therapists identify and help patients resolve pelvic floor-related problems before and after surgery. We find strong support for pelvic floor PT for patients undergoing gender-affirming vaginoplasty.”(1)
Holly Tanner Short Interview Series - Episode 5 featuring Sarah Haran
This week The Pelvic Rehab Report sat down with new faculty member Sarah Haran. Sarah instructs the new Weightlifting and Functional Fitness Athletes remote course scheduled for October 16, 2021.
Who are you? Describe your clinical practice.
My name is Sarah Haran and I have been a PT in Seattle, WA since 2007. I graduated from the University of Washington and have been working in outpatient orthopedics ever since. I opened my private, cash practice, Arrow Physical Therapy in 2016 and we specialize in CrossFit athletes, weightlifters, dancers, and patients with hip impingement. I also teach courses on practice development and coach physical therapist entrepreneurs alongside Dr. Kate Blankshain through our business consulting company, Full Draw Consulting.
Holly Tanner Short Interview Series - Episode 4 featuring Brianna Durand
Inclusive Care for Gender and Sexual Minorities is a remote course created by faculty member Brianna Durand. This course is for anyone, even if you are unsure about the pronouns or the terminology to use. Brianna created this course to provide the basic foundational knowledge around inclusive and gender-affirming care. The second day of the course provides detailed physiological considerations from the pelvic health and general health standpoint for folx undergoing medical transition.
Brianna became interested in pelvic health research pertaining to the LGBTQ+ community when she was in grad school. She was struck by how the community was not mentioned in most formal education and wanted to meet this knowledge gap.
Gender-affirming care describes ideal medical, surgical, and mental health services sought by transgender, non-binary, and gender non-conforming people. This can range from hormone therapy, to top or bottom surgery, facial hair removal, modification of speech, reduction thyrochondroplasty (tracheal cartilage shave), and voice surgery (1). Also common is the practice of genital tucking or packing, and chest binding. All of which the World Professional Association for Transgender Health lists as medically necessary procedures(2).
Aparna Rajagopal, co-author of the Breathing and the Diaphragm: Orthopedic Therapists remote course, shares "I have used breathing and evaluation of the diaphragm as a part of pelvic care for several years now...Through my interactions, I have come to realize that although many of the therapists are aware that the diaphragm and breathing are important, they are unsure of how to assess for dysfunctions and address those dysfunctions."
Pelvic floor patients who may benefit from diaphragmatic breathing exercises include those who present with pelvic pain, incontinence, prolapse, and cervical/thoracic/scapular/lumbar pain. The Breathing and the Diaphragm: Orthopedic Therapists remote course will expand the participant's knowledge of the diaphragm and breathing mechanics. This course offers a different perspective on back pain and alignment, along with the ability to assess and connect breathing and the diaphragm to core stability, continence issues, and the autonomic nervous system.
The autonomic nervous system is in charge of those bodily processes that do not require conscious thought. These include digestion, temperature, blood pressure, and breathing. The autonomic nervous system can be hacked or manipulated with deep breathing exercises such as diaphragmatic breathing.
Holly Tanner Short Interview Series - Episode 3 featuring Lauren Mansell
Lauren Mansell shares, "We're never ready to do this work. We're never ready to be perfect." Her course, Trauma Awareness for the Pelvic Therapist, is for all practitioners, not just physical therapists. Anyone licensed who works with patients can benefit from this topic. However, it can be offputting to put ourselves into a vulnerable position by registering for a course on this topic. Lauren understands this and comes prepared to teach other practitioners about trauma-informed care in the gentlest way possible.
Lauren Mansell, DPT, CLT, PRPC, CYT curated and instructs this course. Lauren worked in counseling and advocacy for sexual assault survivors before becoming a physical therapist. She also brings her experience as a 2017 Fellow of the Chicago Trauma Collective to teach trauma-informed care to medical providers. Trauma-informed care is especially important as the field of pelvic rehabilitation becomes more inclusive.
Pelvic rehabilitation and pelvic therapists really do treat the whole patient. Patients can present with pain, long-term issues, and undisclosed trauma that can be compounded when it includes sex, bladder, or bowel issues. Trauma Awareness for the Pelvic Therapist addresses several topics under this umbrella and spends time on each of the following:
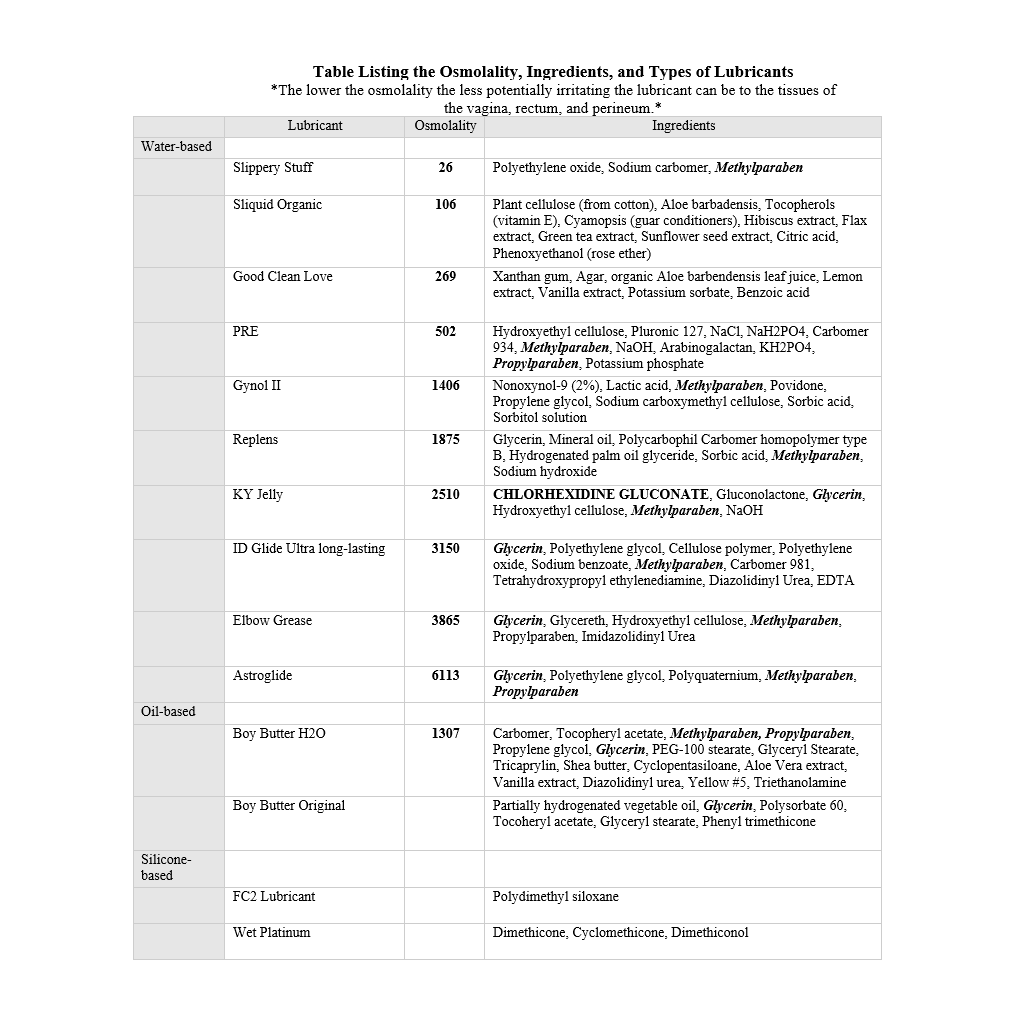
Lubricant use can be a difficult conversation to bring with a patient. There are so many different brands and types of lubricants on the market that it can be overwhelming. Since personal lubricants are available over-the-counter, many users may end up taking home a product that does more harm than good.
Lubricant varieties include water-based, oil-based, organic or natural, silicone, fertility, and specialty lubricants. Each is made with different ingredients and can be utilized in different situations for personal and medical use. When looking at lubricants, it is important to be mindful of components that can be harmful to pelvic health. These include preservatives, glycerin, petrolatum, warming agents, and osmolality.
Preservatives are commonly added to food and other products to increase shelf life and can affect the microflora of the gastrointestinal, vaginal, and rectal areas (similar to how changes in pH can affect microflora). When this balance becomes disrupted infections can occur.
When looking through past blogs from The Pelvic Rehab Report, I ran across this gem submitted by Lauren Mansell explaining Trauma-Informed Approach and her course Trauma Awareness for the Pelvic Therapist. While it is not policy to recycle past articles, this was too good not to share again. Lauren succinctly explains the Trauma-Informed Approach that is instructed in her remote course, Trauma Awareness for the Pelvic Therapist, and it is as pertinent today as it was when first published in 2018.
[as written by Lauren Mansell]…
In my experience, trauma creates the trauma, and the body responds in characteristically uncharacteristic ways.





































