Tibial nerve stimulation has been shown in the literature to be effective for individuals experiencing idiopathic overactive bladder in randomized controlled trials. A systematic review was performed by Schneider, M.P. et al. in 2015 looking at safety and efficacy of its use in neurogenic lower urinary tract dysfunction. Many variables were examined in this review, which included 16 studies after exclusion. The review looked at:
- Acute stimulation (used during urodynamic assessment only)
- Chronic stimulation (6-12 weeks of daily-weekly use)
- Percutaneous or transcutaneous (frequencies, pulse widths, perception thresholds, durations)
- Urodynamic parameter changes baseline to post treatment
- Post void residual changes
- Bladder diary variables
- Patient adherence to tibial nerve stimulation
- Any adverse events
The exact mechanism of these types of neuromodulation stimulation procedures remains unclear, however it does appear to play a role in neuroplastic reorganization of cortical networks via peripheral afferents. No specific literature is currently available for the mechanism on action related to neurogenic lower urinary tract dysfunction. Different applications of neuromodulation however have been studied in the neurogenic populations.
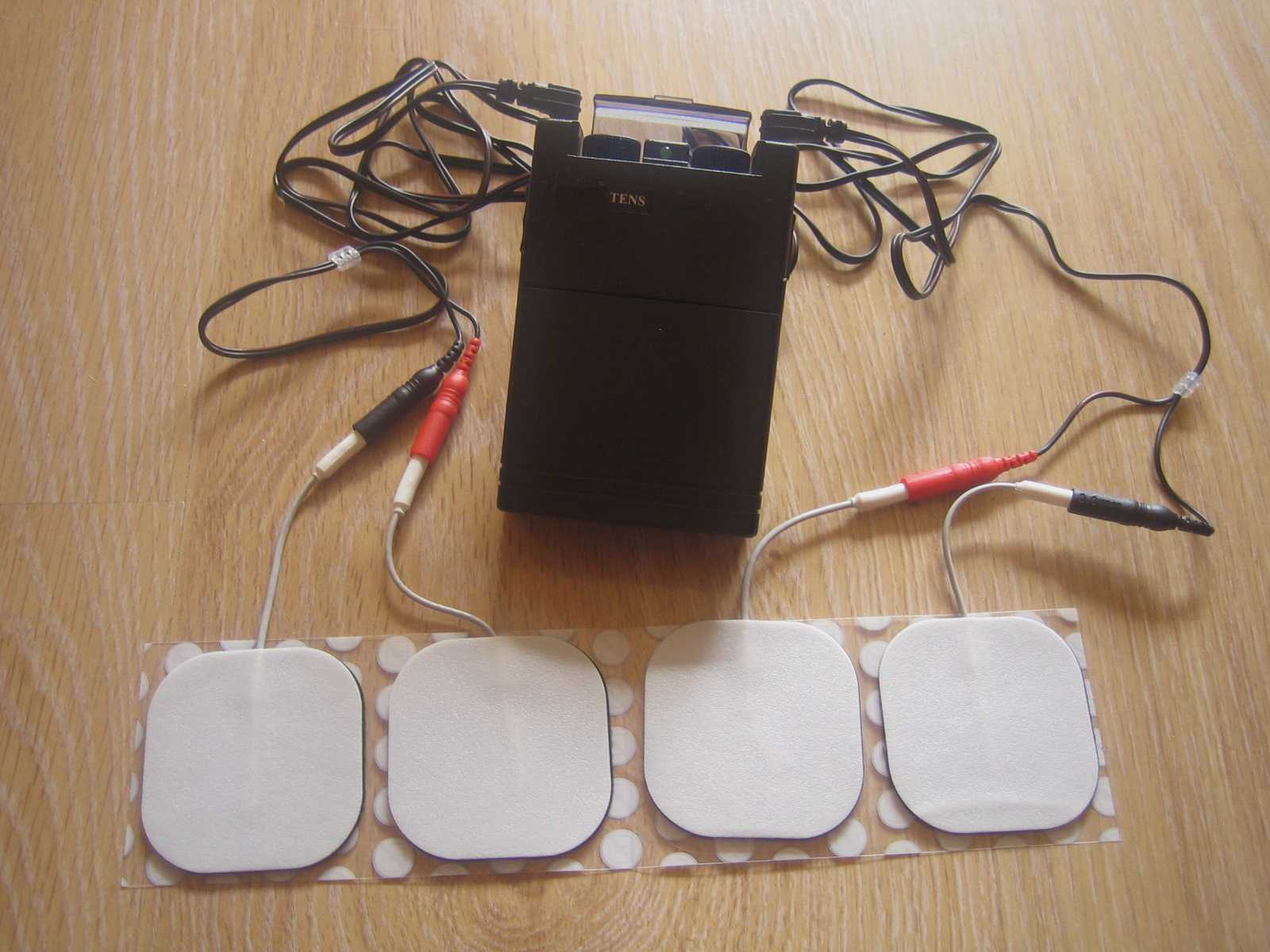
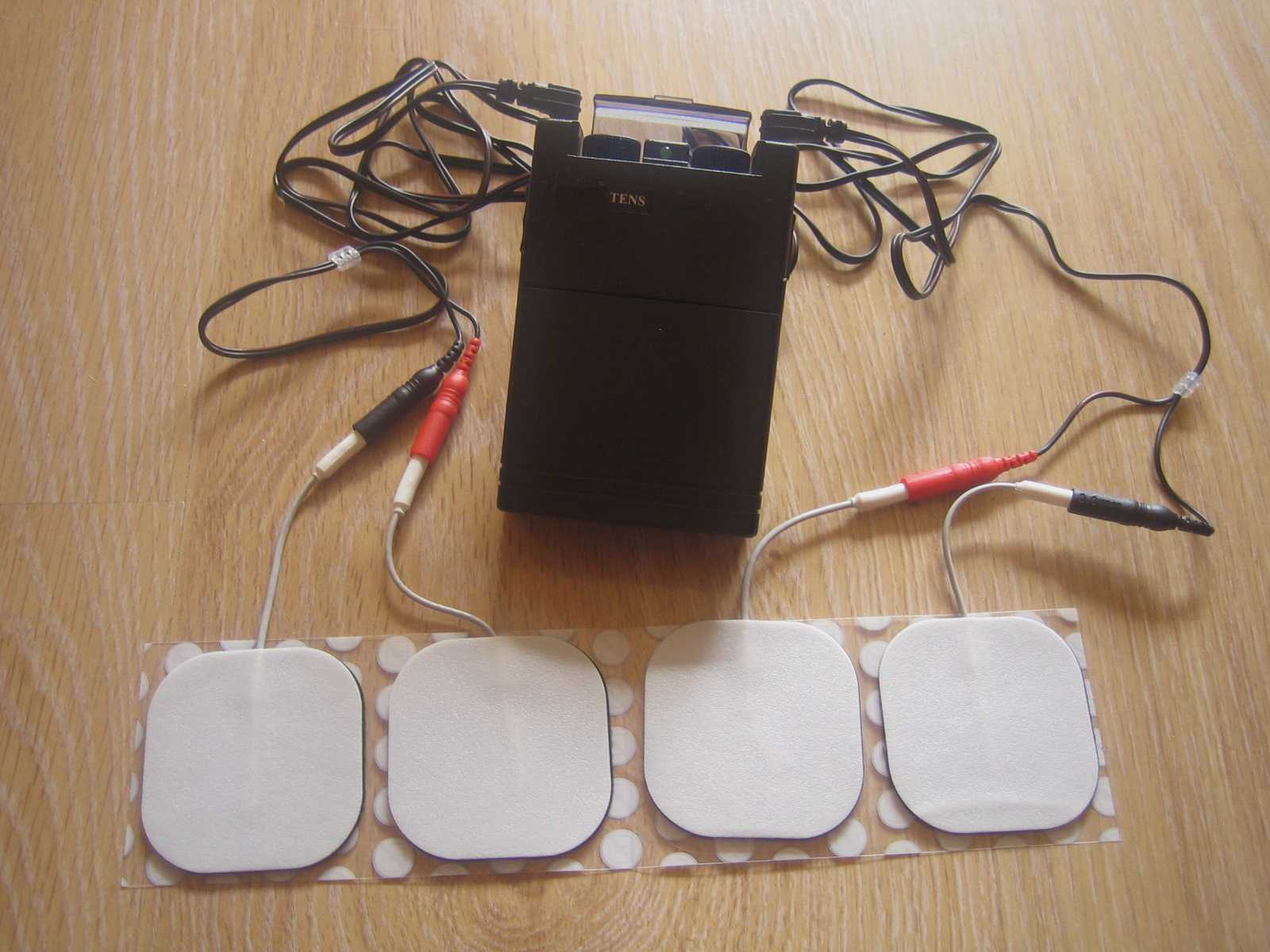
One of the randomized controlled trials they report on included 13 people with Parkinson disease. The researchers looked at a comparison between the use of transcutaneous tibial nerve stimulation (n = 8) and sham transcutaneous tibial nerve stimulation (n=5). Transcutaneous tibial nerve stimulation (TTNS) or sham stimulation was delivered to the people with Parkinson disease 2x/week for 5 weeks, 30-minute sessions (10 total sessions). Unilateral electrode placement was utilized, first electrode applied below the left medial malleolus and second electrode 5 cm cephalad. Confirmation of placement was obtained with left great toe plantar flexion. It is important to note the use of the stimulation intensity is reduced to below the motor threshold during the active treatment to direct the stimulation via peripheral afferents.
Urodynamic testing was performed at baseline and post treatment and revealed statistically significant differences with greater volumes at strong desire and urgency in the TTNS group. Additionally, the TTNS group experienced a 50% reduction in nocturia whereas in the sham group nocturia frequency remained the same. A three-day bladder diary completed by each of the groups also revealed significant positive changes in frequency, urgency, urge urinary incontinence and hesitancy only in the TTNS group.
Conservative management of neurogenic bladder in populations such as Parkinson disease is very important. These individuals experience lower quality of life ratings related to lower urinary tract dysfunction, higher risk of falling with needs to rush to the bathroom, their caregivers experience a higher level stress and burden of care, and tolerance to anticholinergic medications is very poor with multiple unwanted side effects that compound and worsen other symptoms that might be present from the disease process.
Please join us for Neurologic Conditions and Pelvic Floor Rehab to learn how you can help your patients using this modality as one option. Participate in a lab session to learn electrode placement and other parameters to achieve best clinical results for your patients.
1. Perissinotto, M. C., D'Ancona, C. A. L., Lucio, A., Campos, R. M., & Abreu, A. (2015). Transcutaneous tibial nerve stimulation in the treatment of lower urinary tract symptoms and its impact on health-related quality of life in patients with Parkinson disease: a randomized controlled trial. Journal of Wound Ostomy & Continence Nursing, 42(1), 94-99.
2. Schneider, M. P., Gross, T., Bachmann, L. M., Blok, B. F., Castro-Diaz, D., Del Popolo, G., ... & Kessler, T. M. (2015). Tibial nerve stimulation for treating neurogenic lower urinary tract dysfunction: a systematic review. European urology, 68(5), 859-867.
Researchers in Brazil assessed the effects of low-frequency and high-frequency TENS, or transcutaneous electrical stimulation on post-episiotomy pain. This randomized, controlled, double-blind trial included the two electrotherapy interventions as well as a control group. TENS was applied for 30 minutes to the three groups: the high-frequency TENS (HFT) (100 Hz, 100 ms) the low-frequency TENS (5 Hz, 100 ms), and the placebo group. Electrode placement was near the episiotomy in a parallel pattern, and pain evaluations were completed before and after TENS application in resting, sitting, and ambulating. (Electrode placement specifics can be found in the article that is available within the above link.) The interventions and pain evaluations were carried out between six and 24 hours after vaginal delivery.
The intensity of the HFT and LFT was controlled by the participants, with instructions to allow the sensation to be both strong and tolerable. A total of 33 participants completed the study, with 11 in the HFT group, 13 in the LFT group, and 9 in the placebo therapy group. The researchers found that for HFT and LFT, pain improved following application of the electrotherapy, and the effects of the pain reduction lasted one hour after the intervention. Because TENS is a low-cost, low-risk modality, TENS use may be a welcome addition for postpartum care following an episiotomy. The women using high or low-frequency TENS in this study reported that TENS was comfortable and that they would opt to use it again.
If you are interested in learning more about postpartum care and issues such as episiotomies which can interfere with return to function, join faculty member Jenni Gabelsberg in Santa Barbara in January. In addition to discussing a wide variety of common musculoskeletal conditions, she will discuss pelvic floor issues following childbirth that can impact a woman's postpartum recovery. Click here to view the learning objectives for Care of the Postpartum Patient as well as additional dates and locations for this course.