Have you ever tried to teach a patient how to isolate their transversus abdominis (TA) contraction or a pelvic floor muscle (PFM) contraction and the patient had difficulty or you weren’t sure how well they were isolating it? Did you ever wish you had the ability to use real-time ultrasound (US) to confirm which abdominal layers they were isolating or use it for visual feedback to assist in your patient’s learning? Could it be helpful to be able to use real-time US to identify if they were isolating the pelvic floor muscles and give your patient visual feedback? Of course!

Real- time US has been used as an assessment and teaching tool to directly visualize abdominal and PFMs. PFM function can be assessed by observing movement at the bladder base and bladder neck. Various studies have used US on women with and without urinary incontinence (UI). These studies usually use transabdominal (TAUS) and transperineal (TPUS) ultrasound to measure if PFM isometrics or exercises are performed correctly or incorrectly, or how the muscles are functioning.
A 2015 study in the International Urogynecology Journal utilized TAUS to identify the ability to perform a correct elevating PFM contraction and assess bladder base movement during an abdominal curl up exercise. Abdominal curl ups are cited to increase intra-abdominal pressure. Activities that increase intra-abdominal pressure have been cited to provoke stress urinary incontinence (SUI). Abdominal curl ups are often completed in group exercise classes and have been found to provoke SUI in up to 16% of women.
Use of PFM exercises and of “the knack” (performing an isometric pelvic contraction before an exertional activity where intra-abdominal pressure increases, such as before lifting or coughing) has been shown to help manage stress urinary incontinence.
The theory is that elevation of the PFMs during activities that increase intraabdominal pressure (like a curl up) assist in urethral closure and counter act the downward movement, therefore stabilizing the urethra and bladder neck. When using TAUS, while performing a correct PFM contraction, one might expect to see an elevating PFM contraction. In the study, TAUS was used on 90 women participating in a variety of group exercise classes. The participants completed a survey and then three attempts of an abdominal curl up exercise in hooklying. During the curl ups, bladder base displacement was measured to determine correct or incorrect activation patterns. It was found that 25% of the women were unable to demonstrate an elevating PFM contraction, and all women displayed bladder base depression on the abdominal curl exercise. It was also found that parous women displayed more bladder base depression than nulliparous women, and overall 60% of the participants reported SUI. Lastly, this study found there was no association between SUI and the inability to perform an elevating PFM contraction or the amount of bladder base depression.
What interesting information. Using real time US in the clinic could help us identify if our patients were completing “the knack” correctly with specific activities. This study is a great example of how we can use real time US to help collect evidence to provide us with more information that can help us answer our own questions, patient questions, and improve our instructional methods to patients when teaching core or PFM exercises.
1) Barton, A., Serrao, C., Thompson, J., & Briffa, K. (2015). Transabdominal ultrasound to assess pelvic floor muscle performance during abdominal curl in exercising women. International urogynecology journal, 26(12), 1789-1795.
Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC is a published researcher and practitioner who has worked in the realms of brain injury, lymphedema, and oncology. Now she's leading the charge to encourage rehabilitation practitioners to utilize ultrasound diagnostic imaging with their patients, and you can learn these techniques in her Rehabilitative Ultrasound Imaging - Women's Health and Orthopedic Topics course taking place May 1 - 3 in Dayton, OH. We've partnered with SonoSite to make the best ultrasound equipment available for participants in this course.
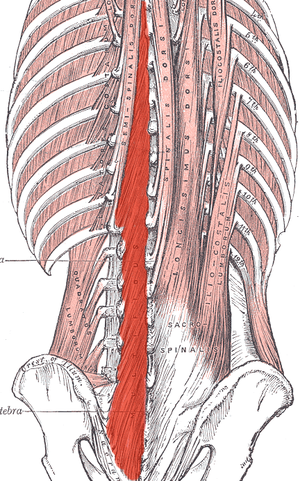
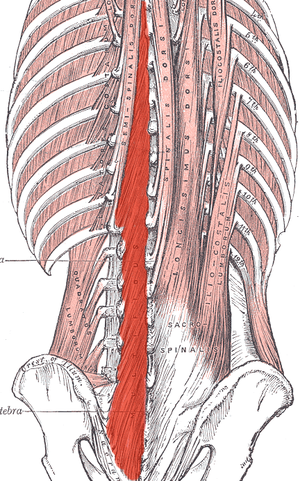 Most of us are treating patients who have back pain of some nature, and we know the importance of the local stabilizing muscles including the transverse abdominis, the lumbar multifidus, and the pelvic floor muscles. These muscles work together to provide tension and create a corset of stability throughout the trunk. A common goal is to rehabilitate these muscles in order to restore motor control and strength, but the muscle depth can make them difficult to assess and palpate.
Most of us are treating patients who have back pain of some nature, and we know the importance of the local stabilizing muscles including the transverse abdominis, the lumbar multifidus, and the pelvic floor muscles. These muscles work together to provide tension and create a corset of stability throughout the trunk. A common goal is to rehabilitate these muscles in order to restore motor control and strength, but the muscle depth can make them difficult to assess and palpate.
I recently read a study that is looking at the development of a test to identify lumbar multifidus function. Herbert et al. found promising results when looking at this “multifidus lift test” for inter-rater reliability and concurrent validity to identify dysfunction in the multifidus. They compared the results of this test with real-time ultrasound imaging of the lumbar multifidus. Inter-rater reliability was excellent and free from errors of bias and prevalence. Concurrent validity was demonstrated through its relationship with the reference standard results at L4-L5, but not so much for L5-S1. This preliminary research supports the reliability and validity of the multifidus lift test to assess lumbar multifidus function at some spinal levels. If this test could be further validated for other spinal levels it would be very beneficial for therapists who are using a specific stabilization program to treat patients.
Until this test is further developed and validated how can therapists know for sure that their patient is truly activating their multifidus? Ultrasound imaging is the answer! Ultrasound imaging gives therapists real-time feedback for whether a patient is able to correctly activate a muscle or not. It is also a wonderful biofeedback tool for patients who are trying to rehabilitate these muscles. Getting your hands on an ultrasound machine can be tough, but therapists who work in a hospital system may have an easier time than you'd think. I have worked with many therapists to help them get access to ultrasound units through “hand me down” units from imaging or labor and delivery departments. I also have helped private practice therapists set up a working relationship with a physician who has an ultrasound in their office. Thinking outside of the box can allow clinicians to gain access to ultrasound units without having to spend a lot of money. Join me in Dayton Ohio this May to hear more about how ultrasound imaging can improve your practice and allow you to incorporate a specific stabilization program into your toolbox.
Herbert JJ, Koppenhaver SL, Teyhen DS, Walker BF, Fritz JM. The evaluation of lumbar multifidus muscle function via palpation: reliability and validity of a new clinical test. Spine J. 2015; 15(6): 1196-202.
One of the dilemmas for many clinicians new to pelvic rehab is trying to figure out which equipment to purchase, and how to convince their employer (or themselves) to purchase the equipment. A common question in relation to equipment for pelvic rehabilitation is “what do I really need?” In a perfect world, and based on both existing and emerging research as well as clinical practice recommendations, we would all have access to pressure biofeedback and real-time ultrasound to help us document and train our patients in best strategies. The truth, however, lies in the fact that when those devices are not available, clinical practice can gain meaningful information from our best tools: our eyes and our hands. Certainly when completing research about pelvic floor generated pressures we might choose pressure biofeedback, and when looking for muscle activation patterns, needle EMG is the right choice, but no one should deny patients the opportunity to learn how to increase or decrease muscle activity, focus on movement retraining, and learn strategies to decrease improve quality of life and function because the latest technology is unavailable.
 Recent research published in the Brazilian Journal of Physical Therapy helps affirm the value of vaginal palpation in an article that assessed the relationship between vaginal palpation, vaginal squeeze pressure, electromyography and ultrasound. Eighty women between the ages of 18 and 35 years old, who had never given birth, and who had no known pelvic floor dysfunction were given a thorough evaluation using a multitude of evaluative methods. These methods included vaginal digital palpation (using Modified Oxford scale), vaginal squeeze pressure, electromyographic activity, diameter of the bulbocavernosus muscles as well as bladder neck movement using transperineal ultrasound. The muscles were assessed in a supine, hooklying position. A strong and positive correlation was found between pelvic floor muscle function and pelvic floor muscle contraction pressure. A less strong correlation was found between pelvic muscle function and pressure and electromyography and ultrasound.
Recent research published in the Brazilian Journal of Physical Therapy helps affirm the value of vaginal palpation in an article that assessed the relationship between vaginal palpation, vaginal squeeze pressure, electromyography and ultrasound. Eighty women between the ages of 18 and 35 years old, who had never given birth, and who had no known pelvic floor dysfunction were given a thorough evaluation using a multitude of evaluative methods. These methods included vaginal digital palpation (using Modified Oxford scale), vaginal squeeze pressure, electromyographic activity, diameter of the bulbocavernosus muscles as well as bladder neck movement using transperineal ultrasound. The muscles were assessed in a supine, hooklying position. A strong and positive correlation was found between pelvic floor muscle function and pelvic floor muscle contraction pressure. A less strong correlation was found between pelvic muscle function and pressure and electromyography and ultrasound.
Vaginal pelvic muscle assessment via palpation has been shown to be more accurate when assessed by more experienced therapists, and use of multiple methods may be most valuable in gaining the most accurate data. In addition to validating the usefulness of pelvic muscle palpation as an evaluative tool, the authors point out that transperineal ultrasound may also be the most appropriate tool for pediatric patients or patients who are otherwise not appropriate for internal pelvic muscle assessment.
Pereira, V. S., Hirakawa, H. S., Oliveira, A. B., & Driusso, P. (2014). Relationship among vaginal palpation, vaginal squeeze pressure, electromyographic and ultrasonographic variables of female pelvic floor muscles. Brazilian journal of physical therapy, 18(5), 428-434.
The following post comes to us from Herman & Wallace faculty member Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC. Allison authored "Use of transabdominal ultrasound imaging in retraining the pelvic-floor muscles of a woman postpartum" and is a leading expert in the use of ultrasound imaging for pelvic rehab. She is the author and instructor of the Rehabilitative Ultrasound Imaging: Women’s Health and Orthopedic Topics offered with Herman & Wallace.
In the pelvic floor series we learn how to perform examinations for cystoceles and rectoceles. It can be more difficult for therapists to examine and quantify the degree of uterine descent. In the last few years translabial ultrasound imaging has also been used to identify what is happening in the anterior compartment upon Valsalva and pelvic floor contraction, including the uterus. This is helpful when trying to determine the degree of uterine prolapse. Degree of pelvic organ descent visible on by ultrasound has been shown to have a near-linear relationship with measures on the POPQ.
 Clinically we see that some patients with severe prolapses have few symptoms, while other patients with smaller prolapses will have more severe complaints of symptoms. This can be puzzling to the clinician who is trying to treat prolapse patients. Shek and Dietz performed a study to set cutoff measures of uterine descent that will predict symptoms of prolapse. Translabial ultrasound imaging was performed on 538 women with 263 women reporting prolapse symptoms. Seventy-five percent of the women presented with grade two or greater prolapse on the POPQ, with most of being cystoceles or rectoceles. The women with more complaints of symptoms of prolapse were more likely to have uterine prolapse. There was a strong association between degree of uterine descent and symptoms of prolapse. They determined that an optimal cutoff to predict symptoms of prolapse due to uterine descent is a cervix descending to 15 mm above the pubic symphysis.
Clinically we see that some patients with severe prolapses have few symptoms, while other patients with smaller prolapses will have more severe complaints of symptoms. This can be puzzling to the clinician who is trying to treat prolapse patients. Shek and Dietz performed a study to set cutoff measures of uterine descent that will predict symptoms of prolapse. Translabial ultrasound imaging was performed on 538 women with 263 women reporting prolapse symptoms. Seventy-five percent of the women presented with grade two or greater prolapse on the POPQ, with most of being cystoceles or rectoceles. The women with more complaints of symptoms of prolapse were more likely to have uterine prolapse. There was a strong association between degree of uterine descent and symptoms of prolapse. They determined that an optimal cutoff to predict symptoms of prolapse due to uterine descent is a cervix descending to 15 mm above the pubic symphysis.
This study intrigues me and makes me wonder how much we are focusing on cystoceles and rectoceles and not looking at uterine prolapses. Using translabial ultrasound imaging is a nice tool to allow the clinician to see what is going on with all of the pelvic organs. With one Valsalva maneuver you are able to assess a lot of information including support of the pelvic organs. It also gives the clinician another way to quantify the degree of prolapse. Ultrasound imaging is a wonderful tool that clinicians can use for assessment as well as a biofeedback tool. If you are interested in learning how to perform this type of assessment, I will be teaching Rehabilitative Ultrasound Imaging: Women’s Health and Orthopedic Topics May 1-3 in Dayton, OH.
Shek KL, Dietz HP. What is abnormal uterine descent on translabial ultrasound? Int. Urogynecol J. 2015; 26(12)1783-7.

What are you saying when giving directions to men during pelvic floor muscle training, and how do those instructions affect the effectiveness of a contraction? These questions are tackled in a study that is very interesting to therapists working in pelvic dysfunction. 15 healthy men ages 28-44 (with no prior training in pelvic floor training) were instructed to complete a submaximal effort pelvic muscle contraction. Tools utilized to acquire data in the study include those below:
| Assessment tool | Measuring |
| Transperineal ultrasound | displacement of pelvic floor landmarks |
| Surface EMG (electromyography) | abdominal, anal sphincter muscle activation |
| Nasogastric transducer | intra-abdominal pressure (IAP) |
| Fine wire electromyography (3 participants only) | puborectalis, bulbocavernosus muscles |
Participants sat upright on a plinth (backrest reclined at ~20 degrees with their knees extended). Directions for the submaximal efforts were given by telling the men to produce a level 3/10 effort with 10 being a maximal contraction. The men were instructed to hold the contraction for 3 seconds, and they were given 10 seconds rest between each of the 4 contractions using different verbal cues. (This series of 4 contractions was repeated with randomization for verbal cues, with a 2 minute rest in-between.) Verbal instructions were intended to target specific contractile tissues as described below- some of this theory could be validated via the fine wire EMG.
| Verbal cue | Targeting |
| "tighten around the anus" | anal sphincter |
| "elevate the bladder" | puborectalis |
| "shorten the penis" | striated urethral sphincter |
| "stop the flow of urine" | striated urethral sphincter, puborectalis |
Displacement, IAP, and abdominal/anal EMG were compared for the different verbal instructions. The greatest dorsal displacement of the mid-urethra and striated urethral sphincter activity was noted with the instruction to "shorten the penis." "Elevate the bladder" encouraged the greatest increase in abdominal EMG and IAP, while "tighten around the anus" induced the greatest anal sphincter activity. Displacement of pelvic landmarks correlated with EMG readings of the muscles thought to produce the targeted movement. The authors conclude that the therapist's choice of verbal instructions can influence the muscle activation and urethral movement in men. They suggest "shorten the penis" and "stop the flow of urine" for optimal activation of the striated urethral sphincter. They also point out the fact that by using the fine wire EMG and correlating muscle activation to observations with the transperineal ultrasound, the study validates the use of the less invasive method. If you are ready to jump into more education about male pelvic rehabilitation, join us in Denver in early August, or Seattle in November.
Today’s contribution to the Pelvic Rehab Report comes from Allison Ariail, the instructor for Herman & Wallace’s Rehabilitative Ultrasound Imaging courses. Join Allison and others this June 12-14 at Rehabilitative Ultra Sound Imaging: Women's Health and Orthopedic Topics - Baltimore, MD!
Is an Ultrasound that provides images of the pelvic floor and other deep musculature a cool gadget to have in the office or something that is truly essential? That depends on who you are asking! If you know how to use Ultrasound imaging properly and market yourself and your practice accordingly, it can become a tool that is not only fun to have and handy to use clinically, but also essential to providing your most efficient and thorough care!
Using an ultrasound (US) machine allows you to view the deeper musculature to assess how the muscles are functioning. The most common muscles assessed with US imaging are the transverse abdominis, the multifidus, and the pelvic floor. The patient then can use what is seen on the US screen as biofeedback to retrain their strategy and timing of recruitment. The therapist can also assess the patient’s ability to activate and maintain a contraction in various positions and even during motor tasks as well. This type of biofeedback is not only useful for pelvic floor patients, but is also important for patients with back and sacroiliac joint pain. Research is showing that using this type of stabilization program is making a difference in athletes. Julie Hides has published two articles recently showing that this type of stabilization program has helped with low back pain in professional cricket players, as well as to decrease the rate of lower extremity injury in Australian professional football players. (1,2) (see my post on The Local Stabilizing Muscles and Lower Extremity Injury.
You may be saying to yourself that you can save a lot of money and just palpate the transverse abdominis (TA), and the multifidus. However I would ask you… are you really feeling a transverse abdominis contraction, or some of the internal obliques? I have had 2 patients referred to me from very capable therapists that I respect and look up to. They were referred to me due to a lack of progress in their treatment. The therapist was addressing a local stabilization program, but their back pain was not getting better. To their credit, the therapist was able to train both patients to perform a proper TA contraction in supine, however one patient was unable to hold a contraction beyond 1 second, and another one was not able to activate it in sitting, or standing. This would explain why they were not progressing with respect to their pain. After treating each patient for 1 or 2 visits using US imaging, and sending them back to their referring therapist, they made rapid progress. Both therapists were so convinced on the usefulness of US imaging that they both went out and bought a machine to use in their clinic. Additionally, you would be surprised how many physical therapists (I can’t count the number on two hands anymore) I have seen that think they are properly performing a TA contraction and want to see how they are doing on the US. However, once we used the US imaging to assess their TA contraction, they realized they were overcompensating with their internal obliques. This is with physical therapists who have more knowledge than the general public regarding the importance of these muscles and how to activate them!
If you are knowledgeable in using ultrasound imaging, you open your doors to a number of possible patients you may not be currently accessing as referrals. There are numerous women and men who would like to receive treatment for pelvic floor weakness issues, but do not want to have to disrobe each treatment. Using ultrasound imaging is a wonderful option for these patients. It also is a way to treat younger patients that you have not been able to treat in the past as well (I would recommend taking the Pediatric Incontinence and Pelvic Floor Dysfunction course prior to treating pediatric patients). By using ultrasound imaging you not only gain an edge over your competing clinics that specialize in pelvic floor therapy, but you can gain an edge for back patients and sacroiliac joint patients as well. For the reasons I stated above when discussing a stabilization program centered on the use of US imaging, you could become very busy with referrals from spine surgeons, and ortho docs. In my office we have six therapists trained in using ultrasound imaging and two ultrasound machines. One of our most limiting factors is not the lack of patients to use ultrasound on, but that we only have two US units available to use! We have several spine physicians that send all of their patients to us because they have seen the difference using ultrasound imaging and the stabilization program can make in patients’ lives. We are eagerly awaiting a third machine and know it will be immediately used and allow us to further grow our clinic.
Now you may be saying, “Yes this would be handy but the pricing makes it impossible!” I would say think outside of the box! Some machines are going down in price making them more affordable. Plus, the settings we as therapists use are pretty basic, so we do not need to purchase a unit with a lot of bells and whistles that makes it more expensive. However there are other ways to acquire a unit other than purchasing one brand new. You could look into the price of refurbished units or look to your referring physician groups that you have a good relationship with. You may be surprised to find out how much physician’s offices get for machines when they are upgrading; hardly anything! If you work for a hospital system you may be able get the old machine transferred to your department for no cost to you! Or if you work in a private practice, you could offer to match the little amount the office would get from the vendor when upgrading. I guarantee you it would not be as much as a new unit. You also might be able to share a unit with another department, office, or clinic. In the past, I have shared ultrasound units with a surgical department, and a gynecology office. I would use the ultrasound some days of the week, and they would other days of the week. It worked out well! There are a lot of possibilities of ways to acquire an ultrasound unit if you think outside of the box! It may take a little effort coordinating things in order to get an US unit, but with proper knowledge, proper marketing, and word of mouth your business will grow and you will not regret the decision to invest in your practice!
Join me to discuss more ideas of how to use US imaging to grow your practice in both clinical skill as well as business growth this June in Baltimore!
1. Hides, Stanton, Wilson et al. Retraining motor control of abdominal muscles among elite cricketers with low back pain. Scand J Med Sci Sports. 2010; 20: 834-842.
2. Hides JA, Stanton WR. Can motor control training lower the risk of injury for professional football players? Med Sci Sports Exec. 2014; 46(4): 762-8.
Today's post on the Pelvic Rehab Report comes from faculty member Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC. Allison instructs the ultrasound imaging courses, the next of which will be Rehabilitative Ultra Sound Imaging: Women's Health and Orthopedic Topics in Baltimore, MD on Jun 12, 2015 - Jun 14, 2015.

In the past several decades there has been quite a bit of research regarding stabilization of the low back and pelvic ring. We as therapists have changed our focus from working more of the global stabilization muscles to the local stabilizing muscles; the transverse abdominis, the lumbar multifidus, and the pelvic floor. Both research studies and clinical experience has shown us what a positive difference working on these muscles can makes for back pain and pelvic ring pain, as well as for the risk of injury in the back and pelvic ring. However, what does it do for risk of injury for the lower limb? In 2014, Hides and Stanton published a study looking at the effects of motor control training on lower extremity injury in Australian professional football players. A pre- and post-intervention trial was used during the playing season of the Australian football league as a panel design. Assessment included magnetic resonance imaging and measurements of the cross-sectional area of the multifidus, psoas, and quadratus lumborum, as well as the change in trunk cross-sectional area due to voluntary contraction of the transverse abdominis muscle. A motor control program included training of the multifidus, transversus abdominis, and the pelvic floor muscles using ultrasound imaging for feedback that then progressed into a functional rehabilitation program was used with some of the players. Injury data was collected throughout the study. Results showed that a smaller multifidus or quadratus lumborum was predictive of lower limb injury during the playing season. Additionally, the risk of sustaining a severe injury was lower for players who received the motor control intervention.
This is interesting and intriguing information. Yes, there are many factors that are involved in sustaining an injury during a sport. However, it would be a good idea to do a quick screen of the local stabilizing muscles before a playing season, whether it is a professional player or an adolescent player. Do adolescents really have issues with weakness in their local stabilizing muscles? Yes! Clinically I have seen adolescent players who display back pain and other issues related to weakness in their core muscles. Usually this occurs after they have gone through a growth spurt, but some of these adolescent athletes did not recover, even several years after the large growth spurt.
What a nice community service it would be to screen a local sports team for strength of the local stabilizing muscles in order to decrease injuries! It would also be nice to see additional research regarding this topic! To learn more about recent research and how to use ultrasound imaging to accurately assess and treat the local stabilizing muscles, join me at Johns Hopkins in Baltimore this June for the Rehabilitative Ultrasound Imaging for the Pelvic Girdle and Pelvic Floor course.
Hides JA, Stanton WR. Can motor control training lower the risk of injury for professional football players? Med Sci Sports Exec. 2014; 46(4): 762-8.
Today's post is written by faculty member Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC. You can join Allison in her Rehabilitative Ultrasound Imaging: Women's Health and Orthopedic Topics course, which takes place in Baltimore this year, June 12-14.
Since the mid 1990’s the POP-Q has been used to quantify, describe and stage pelvic organ prolapse. A series of 6 points are measured in the vagina in relation to the hymen. In a recent years, translabial ultrasound imaging has been used to look at the pelvic organs and the pelvic floor. A skilled practitioner can view pelvic floor muscle contractions, as well as Valsalva maneuvers and the effects each of these have on the pelvic organs. For example funneling of the urethral meatus, rotation of the urethra, opening of the retrovesical angle, and dropping of the bladder neck and uterus can be viewed using ultrasound imaging of the anterior compartment during Valsalva maneuvers. Pelvic organ descent seen on ultrasound imaging has been associated with symptoms of prolapse.

Until now the relationship between ultrasound and clinical findings has not been examined. A recent study by Dietz set out to see if there is an association between clinical prolapse findings and pelvic descent seen on ultrasound. Data was obtained on 825 women seeking treatment at a urogynecological center for symptoms of lower urinary tract or pelvic floor muscle dysfunction. Five coordinates of the POP-Q scale were measured and compared to ultrasound measures of descent. All data was blinded against other data obtained. Clinically, 78% of the women were found to have a POP-Q stage of 2 or greater. It was found that all coordinates were strongly associated with ultrasound measures of descent. The association was almost linear, particularly for the anterior compartment. This means that ultrasound measures can be used to quantify prolapse and be comparable to the POP-Q. Proposed cutoffs have been made for the bladder, uterus, and rectum in relation to the pubic symphysis.
It is exciting to see ultrasound use in the quantification and identification of more gynecological disorders. The use of translabial ultrasound imaging is growing and continuing to be researched. It is an exciting field to be a part of and I look forward to seeing where this research goes. I believe it will be used to help improve surgical procedures as well candidate selection for surgery. Join more for more discussion regarding translabial ultrasound imaging and learn how to view these images in Rehabilitative Ultrasound Imaging for the Pelvic Girdle and Pelvic Floor in Baltimore this June!
Dietz HP, Kamisan Atan I, Salita A. The association between ICS POPQ coordinates and translabial ultrasound findings: implications for the definition of ‘normal pelvic organ support’. Ultrasound Obstet Gynecol. 2015; April.