Anyone working in pelvic health knows all too well that the symptoms of female pelvic floor dysfunction (PFD) — from bladder leaks and pain with vaginal penetration to anal pain and fecal incontinence — are vastly underreported. Most providers do not screen for pelvic health symptoms and patients are either reluctant to bring them up or assume that they’re ‘just the way it is’ if you own a uterus (and especially if you’ve had kids).
Just how underreported are pelvic health symptoms? That’s one of the questions that the 2024 Origin Pelvic Health Study sought to answer. The consumer-facing study consisted of a 10-minute, double-blinded, online, quantitative survey conducted by the market research firm Ipsos, with a base sample of 612 U.S. women, ages 18-59.
Study participants were asked whether they had experienced bladder, bowel, and sexual symptoms in the past year, how those symptoms had impacted their lives, and whether they had gotten care for their symptoms. Additional questions were asked of those who had given birth within the past five years or who were in peri/menopause to both explore how these major life events impact pelvic health symptoms and reveal gaps in related care and education.
As a clinical reviewer of the study and an APTA Pelvic Health grant recipient working on my own research, I’m excited that companies like Origin are collecting this valuable data, which not only garners media attention that can be hard for pelvic health researchers to attain (the Origin study was written up in Vogue), it can help inspire and steer our research in important new directions.
The study includes too many eye-opening statistics to list here, but below are 3 high-level takeaways:
- The majority of U.S. women ages 18-59 are dealing with multiple pelvic health symptoms.
PFD has most recently been found to impact 1 in 3 women, based on a 2022 study that examined the medical records of 25,425 women seeking primary care. ICD-10 codes were used to determine presence of PFD, including urinary incontinence, pelvic organ prolapse, bowel, dysfunction, and difficult defecation. Other pelvic floor-related conditions like vulvovaginal pain or orgasm difficulty were not included.
In contrast, the Origin study included a long list of pelvic health symptoms described in terms women often use themselves, with the goal to expose just how common these symptoms really are. What they found was that most women had one or more symptoms, and only a tiny minority had received care for them.
75% of U.S. women between the ages of 19 and 58 have dealt with two or more pelvic health symptoms within the past year. The average number of pelvic symptoms reported was 5.
Some of the symptoms experienced most often in the past year by U.S. women ages 18-59:
Bladder sypmtoms:
- 48% report bladder leaks when they cough, sneeze or exercise
- 38% report peeing more than once every 2 hours
- 37% report feeling like they had to pee again right after going
- 33% report feeling like they could barely hold their pee
- 27% report feeling like they couldn’t fully empty their bladder
Bowel symptoms:
- 52% report straining to have a bowel movement
- 48% report feeling like they can’t fully empty their bowels
- 29% report pain with having a bowel movement
- 21% resort leaking gas or poop
Sexual symptoms:
- 33% report inability to orgasm
- 25% report unsatisfying orgasm
- 22% report pain with sex
- 18% report delayed orgasm
Interestingly, the study also found that Millennial women were more likely to report a host of symptoms in the past year, compared to Gen X.
- Pregnant and postpartum patients are left in the dark when it comes to preparing for and recovering from the immense physical strain of childbirth.
As major health organizations seek to improve the current dire state of postpartum care, mentions of pelvic health and pelvic floor physical therapy are often limited to recommendations that postpartum patients be evaluated for urinary and fecal incontinence and referred to pelvic floor PT as needed.
Those of you who are women’s health specialists who focus on prenatal and postpartum PT, know that we have so much more to offer. The Origin Study highlighted the need for the exact guidance and expertise that pelvic floor PTs can provide.
Among women who had given birth with in the past 5 years:
- 85% report receiving no guidance on reducing their risk of tearing during childbirth.
- 65% report receiving no guidance on how to effectively push out a baby.
- 50% report receiving no guidance on how to manage pregnancy pain.
- 86% report receiving no guidance on how to heal their pelvic floor after childbirth.
- 83% report receiving no guidance on how to heal their abdominals after pregnancy and childbirth.
- 71% said they received no guidance on how to exercise safely before or after childbirth.
In addition, 44% of women who had a baby in the past 5 years say providers did not help them understand what is or isn’t normal in terms of their pelvic health systems. And 23% said they felt “not at all supported” by their medical providers during their postpartum recovery.
- Pelvic floor PT continues to be underutilized, resulting in unnecessary pain and suffering for women of all ages.
It’s unlikely to surprise you that, of the Origin study participants who reported pelvic health symptoms within the past year, 96% had not received medical care for their symptoms. Of study respondents who had given birth within the past 5 years, 92% said they had not seen a pelvic floor PT to support their recovery after their most recent delivery.
Without proper screening by providers and referrals to pelvic floor PT, women will continue to suffer in silence, confused about what is and isn’t normal when it comes to their pelvic health.
The Origin study reiterates what pelvic health specialists and their patients already know — pelvic health symptoms significantly disrupt women’s lives. 64% of study respondents who report pelvic health symptoms in the past year say that these symptoms negatively impact their lives. And that number is even higher among women who have given birth within the past 5 years, at 79%.
Despite how discouraging it can be to read through these statistics, it’s important to get loud about them and continue to demand better. I’m grateful to my colleagues at Origin for making research part of their mission and am excited to see this data is used to fuel more research, draw more attention to pelvic health, and drive positive change in our healthcare system.
AUTHOR BIO:
Jessica Swartz, PT, DPT, CCI
 Jessica Swartz, PT, DPT, CCI, is a physical therapist at Origin, a leading provider of pelvic floor and whole-body physical therapy with a special focus on pregnancy and postpartum. She is also working on her PhD in Public Health with an emphasis on Health Behavior in the Joint Doctoral Program of Public Health at UC San Diego/San Diego State University, where the focus of her research is developing ways to use physical therapy as a tool to improve women’s and maternal health outcomes and address health disparities.
Jessica Swartz, PT, DPT, CCI, is a physical therapist at Origin, a leading provider of pelvic floor and whole-body physical therapy with a special focus on pregnancy and postpartum. She is also working on her PhD in Public Health with an emphasis on Health Behavior in the Joint Doctoral Program of Public Health at UC San Diego/San Diego State University, where the focus of her research is developing ways to use physical therapy as a tool to improve women’s and maternal health outcomes and address health disparities.

Did you know that chronic pain affects an estimated 51.6 million adults in the United States alone? That's almost 21% of the population (1). It's a debilitating condition that can disrupt daily life and limit one's ability to function. But what about those with hypermobility? Often individuals with hypermobility are even more susceptible to chronic pain and their treatment may require a unique approach.
There are many variables that make a person more susceptible to developing chronic pain. Some of these include genetics, prior trauma, culture, and health history. Patients with hypermobility are more likely to develop chronic pain and may also need to be treated with a different lens than the rest of the population.
What is Hypermobility
Hypermobility spectrum disorder (HSD) includes joint hypermobility syndrome (JHS) as one of its conditions and is a connective tissue disorder characterized by chronic musculoskeletal pain due to joint hyperextensibility and is a common cause of chronic pain, fatigue, headaches, anxiety, orthostasis, and abdominal pain. Hypermobility spectrum disorder (HSD) is sometimes considered a milder variant of hypermobile EDS (hEDS) and is seen in up to 3% of the general population, with a prevalence rivaling fibromyalgia, gout, and rheumatoid arthritis (2).
Joint hypermobility implies a range of motion of a joint that exceeds the documented “norm.” Norms for each joint are determined by the specific joint anatomy, the person’s age, sex, and ethnicity. Hypermobility is typically scored using the Beighton scale requiring at least a 5 to be classified as systemically hypermobile. The Beighton score is determined by 9 points awarded for each described condition met. The conditions include (3,4):
- Elbow hyperextension of at least 10 degrees (one for each elbow)
- Knee hyperextension of at least 10 degrees (one for each knee)
- Ability to passively extend the pinky finger to 90 degrees or more (one for each hand)
- Ability to touch the thumb to the forearm with wrist flexion (one for each hand)
- Ability to forward flex the trunk at the hips and place both palms on the floor with knees extended.

Hypermobility as a problematic condition occurs on a spectrum and ranges from Hypermobility Spectrum Disorder (HSD) to genetic connective tissue disorders such as hypermobile EDS (hEDS). Patients with connective tissue disorders often have other symptoms associated with the syndrome such as fragile blood vessels or cardiac arrhythmias (3). Those with generalized joint hypermobility are less likely to have other associated comorbidities.
Hypermobility and Rehab
A patient with hypermobility must have their hypermobility considered in their treatment plan as their tissues, and force tolerance of tissues, differ from the rest of the population. Patients with hypermobility may present with decreased strength overall and require more strength than typical to perform activities. This is likely due to the extensibility of the tendons and ligaments, changing the force a muscle can produce. Patients with hypermobility also often have decreased proprioception, as their tissue laxity cannot provide as much awareness to the brain. These variables can lead to a higher incidence of injury, with dislocation common for those with hEDS (4).
Hypermobility is also correlated with pelvic pain and dysfunction, especially in female patients. They are more prone to pelvic organ prolapse but also may present with pelvic floor muscle overactivity (3) creating a difficult case to treat, especially if they have chronic pain in addition. This patient will often benefit from rehabilitation to address the prolapse, muscle overactivity, and then coordination of core and pelvic stabilizers. Knowing that the patient has hypermobility can be vital to the successful treatment plan for this presentation. When treating patients with hypermobility, they often have decreased functional tolerances for loading, not only at the joints but also systemically. hEDS especially, is highly associated with autonomic dysfunction such as postural orthostatic tachycardia syndrome (POTS), which may affect your treatment plan as well. A portable pulse oximeter and slow positional changes may be helpful in decreasing and monitoring symptoms (3,4).
 Pain Patterns and Hypermobility (3)
Pain Patterns and Hypermobility (3)
Pain patterns for the hypermobile patient include all 3 subtypes of pain.
- Nociceptive Acute Pain
- Neuropathic Pain
- Nociplastic Pain
Nociceptive acute pain will occur at localized injury sites with frequent dislocations, strains, and sprains. These recurrent injuries can then lead to chronic musculoskeletal changes of the joint that affect function and gait.
Neuropathic pain can also become problematic for this population. Due to the increased laxity of their vertebrae, they may suffer from higher incidences of spinal cord compression and peripheral nerve compression. It is also becoming more common to evaluate this population with a dermal biopsy for small fiber neuropathy. As the patient experiences continued nociceptive and neuropathic pain inputs over and over, their nervous system may also sensitize causing both peripheral and central sensitization with nociplastic pain.
Nociplastic pain may then transform into widespread generalized pain. As their pain patterns progress, they may start to experience more fear avoidance behaviors and may become deconditioned. Deconditioning in turn can lead to more injuries and continues a recurrent cycle for these patients.
Conclusion
Knowing that patients with hypermobility are more susceptible to chronic pain allows us to treat this population more effectively. As rehab practitioners, we can educate the patient, improve strength, improve stability, improve proprioception, and work to desensitize the nervous system. A sensitive nervous system may be the initial hurdle with the hypermobile patient.
Pain neuroscience education is the first step to educate the patient on how their nervous system functions and to decrease fear they may have around pain. After education, there are several physical interventions we can use for the nervous system including dry needling, spinal mobilization, manual therapy, and exercise.
Ready to Learn More?
Expand your knowledge, experience, and treatment in understanding and applying pain science to the chronic pelvic pain population with Alyson Lowrey and Tara Sullivan in their upcoming course Pain Science for the Chronic Pelvic Pain Population on August 17-18, 2024.
This course is not specific to the patient who is hypermobile. However, there are portions of the course that address this population. This course provides a thorough introduction to pain science concepts including classifications of pain mechanisms, peripheral pain generators, peripheral sensitization, and central sensitization in listed chronic pelvic pain conditions; as well as treatment strategies including therapeutic pain neuroscience education, therapeutic alliance, and the current rehab interventions' influence on central sensitization.
Pain Science for the Chronic Pelvic Pain Population is a remote course that will provide you with the understanding and tools needed to identify and treat patients with chronic pelvic pain from a pain science perspective. Lecture topics include the history of pain, pain physiology, central and peripheral sensitization, sensitization in chronic pelvic pain conditions, therapeutic alliance, pain science and trauma-informed care, therapeutic pain neuroscience education, the influence of rehab interventions on the CNS, and specific case examples for sensitization in CPP.
References:
- Rikard, S. Michaela, et al. “Chronic pain among adults — United States, 2019–2021.” Morbidity and Mortality Weekly Report, vol. 72, no. 15, 14 Apr. 2023, pp. 379–385, DOI: https://doi.org/10.15585/mmwr.mm7215a1.
- Kumar, Bharat, and Petar Lenert. “Joint hypermobility syndrome: Recognizing a commonly overlooked cause of chronic pain.” The American Journal of Medicine, vol. 130, no. 6, June 2017, pp. 640–647, DOI: https://doi.org/10.1016/j.amjmed.2017.02.013.
- Syx D, De Wandele I, Rombaut L, Malfait F. Hypermobility, the Ehlers-Danlos syndromes and chronic pain. PubMed. 2017;35 Suppl 107(5):116-122.
- Scheper M, De Vries JE, Verbunt J, Engelbert RHH. Chronic pain in hypermobility syndrome and Ehlers-Danlos syndrome (hypermobility type): it is a challenge. Journal of Pain Research. August 1, 2015:591-601
AUTHOR BIO
Alyson Lowrey, PT, DPT, OCS
Dr. Lowrey attended the University of New Mexico where she received a BA degree in Psychology in 2011. She then attended the University of New Mexico School of Medicine to earn her Doctor of Physical Therapy degree in 2014. Following graduation from UNM, Alyson completed the HonorHealth Orthopaedic Residency program in 2015 and became a board-certified orthopedic specialist (OCS) in 2016. She is now the director of that residency program and lectures about pain and pelvic dysfunction in the curriculum. Alyson treats the pelvic floor patient population through an orthopedic approach, working closely with pelvic floor specialists. This allows for a wholistic style addressing the entire patient from a functional perspective. Alyson’s clinical interests include the evaluation and treatment of chronic pain, lumbar and cervical spine disorders, foot and ankle disorders, pelvic pain, and clinical instruction. She is certified in dry needling and an APTA-certified clinical instructor, regularly taking students from several PT schools. She participates in Creighton’s and Midwestern University’s Doctor of Physical Therapy programs as adjunct faculty assisting in lab and lecturing in Biomechanics, Kinesiology, and Musculoskeletal courses. Outside of the clinic, she enjoys being active, doing yoga, crafting, and spending time with her husband and cats.

I arrived to Pelvic Health Physical Therapy by fruitful exposure and a professional demand to fulfill a new employer’s needs. 10 years later, I am all-in serving women and men with bladder, bowel, sexual dysfunction, and abdominopelvic pain to optimally live their lives well more comfortably.
Throughout my PT education at Washington University in St. Louis, I envisioned specializing in Orthopedics using a Movement Systems Impairment (MSI) diagnostic and treatment approach. While a student in my final 3-month clinical experience at a hospital-based Outpatient Orthopedic Clinic, I had the good fortune to be paired with a clinical instructor who was largely Orthopedic-based but treated Pelvic Health 1 day per week as the sole Pelvic Health PT Provider (shoutout Barb Davis!). The setting was a large community-based safety-net institution, Denver Health, which served Denver residents including underserved populations. Patients presented with chronic pain, complex socioeconomic dynamics, and diverse ethnic backgrounds with Denver historically being a migrant and refugee-welcoming city. My pelvic patients were interesting, and my Pelvic Health interest was sparked.
As a new graduate seeking employment, I secured a job at a hospital-based Outpatient Orthopedic Clinic in San Diego, CA at Scripps Health. My new position was created for an Orthopedic PT who was interested in being mentored in Pelvic Health PT due to a growing need to support Pelvic Health patients and providers in North County San Diego. I was offered mentorship and financial support to pursue continuing education to set a foundation in Pelvic Health. I had an interest, there was a clinical need, I seized the opportunity, ran with it, and I am so grateful I did.
My astute Pelvic Health Mentors (Alissa Meredith, PT, MPT and Destiny Bochinski, PT, DPT, PRPC) highly encouraged me to take the foundational Pelvic Floor Series (which has been updated to the Pelvic Function Series this year) through Herman & Wallace. I was already familiar with Herman & Wallace through my exposure at Washington University in St. Louis, where they host various Herman & Wallace courses. I am so glad I chose to follow my Pelvic Health educational path with Herman & Wallace Rehabilitation Institute. I was lucky enough to be taught Pelvic Floor Level 1 (now called Pelvic Function Level 1) by the venerable and entertaining Holly Herman & Kathe Wallace. Fast forward 10 years and I have taken the full Pelvic Floor Series, Ramona Horton’s Visceral Fascia Mobilization Series, Male Pelvic Health, Nutritional Perspectives, Pregnancy Course, IC, Rehabilitative Ultrasound, and a myriad of other Herman & Wallace continuing education courses. I have a wide arsenal of didactic information, manual skills, proficiency in biofeedback modalities use, and clinical experiences to treat the gamut of simple to complex pelvic and orthopedic patients. Citing the incredible Ramona Horton, MPT, DPT, I completely agree that Pelvic Health is applying Orthopedics within the pelvic cavity. I am grateful to have a practice that is largely Pelvic Health-based with a smattering of Orthopedics. In reality, I practice ~65-70% Pelvic Health and 30-35% Orthopedics.
Across my professional journey, I started as the third Pelvic Health PT at the clinic where I work, to now being one of eight Pelvic Health PT providers at that same comprehensive outpatient rehab center, Scripps Rehabilitation Services in Encinitas. I am lucky to be part of a burgeoning Pelvic Health Team at our clinic site as well as across the larger health system. I was lucky to be mentored by two amazing colleagues, including now a Herman & Wallace Instructor, Destiny Bochinski, who I continue to work with and collaborate well with. I am appreciative of the opportunity to continue to grow professionally by serving as a Pelvic Health mentor at my clinic and TA for Herman & Wallace, which I’ve been doing since 2020.
Thank you for letting me share my story, which is one of seizing a ripe opportunity and allowing my career path to evolve with an initial spark that I didn’t early on envision would be my path, but I love where I’ve been and my trajectory forward.
AUTHOR BIO
Jackie Castillo, PT, DPT, MSC
 Jackie Castillo, PT, DPT, MSCI is a Board-Certified Orthopedic Clinical Specialist based out of San Diego, CA who practices Pelvic Health and Orthopedic Physical Therapy at Scripps Rehabilitation Services in Encinitas. She received her DPT and MSCI (Master of Science in Clinical Investigation) Degrees from Washington University in St. Louis in 2013. She received her BS in Animal Physiology & Neuroscience from the University of California, San Diego in 2005. She has served as a Teaching Assistant for Herman & Wallace since 2020. She intends to sit for the Herman & Wallace PRPC Exam this year. She enjoys running, yoga, walking her puppy, hiking, biking, and exploring good food and drink with her soon-to-be husband, family, and close friends.
Jackie Castillo, PT, DPT, MSCI is a Board-Certified Orthopedic Clinical Specialist based out of San Diego, CA who practices Pelvic Health and Orthopedic Physical Therapy at Scripps Rehabilitation Services in Encinitas. She received her DPT and MSCI (Master of Science in Clinical Investigation) Degrees from Washington University in St. Louis in 2013. She received her BS in Animal Physiology & Neuroscience from the University of California, San Diego in 2005. She has served as a Teaching Assistant for Herman & Wallace since 2020. She intends to sit for the Herman & Wallace PRPC Exam this year. She enjoys running, yoga, walking her puppy, hiking, biking, and exploring good food and drink with her soon-to-be husband, family, and close friends.

Imagine you’re a provider who has foundational information about the pelvic floor. Maybe you’ve just started taking coursework for adults, you may have taken a pediatric pelvic health class or maybe you’ve been treating adults for years. You know the anatomy, the physiology, and the general treatment practice guidelines.
- Your clinic gets a call about a baby with colic and your supervisor asks you if you could treat it. Do you accept the evaluation?
- You see a post on a “mommy Facebook group” asking for potty training tips for a child who is withholding stool during potty training. Do you tag your business/practice as a resource that can help?
- You have a family friend with a child struggling with voiding during the school day and they ask you for advice as a pelvic health provider. Do you have ideas on how to guide them?
- A patient you are seeing for pelvic floor issues asks you to start treating their teenager because they have “the same issues.” Does this seem scary to you?
Pediatric Pelvic Floor Play Skills is a class written to be a supplement to other pelvic health education classes a pelvic floor therapist has likely taken. This class helps providers take the pelvic health knowledge they have, and learn activities they can perform with different ages of children to help work on their pelvic floor function. The class shows videos of actual treatment sessions of different children in different age groups showing how to integrate stretching, strengthening, coordination, and other fun activities into a therapy visit.
One of the tricky parts of working with children is including the child in their plan of care and coordinating with caregivers. Pediatric Pelvic Floor Play Skills talks about specific concerns and considerations by age, as well as strategies to bring to a provider's practice. This class is for the provider who does not have a lot of experience treating pediatric patients and wants to learn how to make sessions enjoyable and effective.
This class includes sample home programs, equipment purchase lists (with a budget in mind), tips for helping get families on board with the implementation of care, and resources such as outcomes measures, developmental milestone checklists, and recommendations things parents ask for like how to talk about periods and sex.
The next Pediatric Pelvic Floor Play Skills remote course is scheduled for June 29th, come spend a day learning how to integrate what you already know into a playful session for your tiniest of clients to your angstiest teenager.
AUTHOR BIO
Mora Pluchino, PT, DPT, PRPC
 I am a graduate of Stockton University with my BS in Biology (2007) and Doctorate of Physical Therapy (2009). I have experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. I began treating Pelvic Health patients in 2016 and now have experience treating women, men, and children with a variety of Pelvic Health dysfunction. There is not much I have not treated since beginning this journey and I am always happy to further my education to better help my patients meet their goals.
I am a graduate of Stockton University with my BS in Biology (2007) and Doctorate of Physical Therapy (2009). I have experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. I began treating Pelvic Health patients in 2016 and now have experience treating women, men, and children with a variety of Pelvic Health dysfunction. There is not much I have not treated since beginning this journey and I am always happy to further my education to better help my patients meet their goals.
I strive to help all of my patients return to a quality of life and activity that they are happy with for the best bladder, bowel, and sexual functioning they are capable of at the present time. In 2020, I opened my own practice called Practically Perfect Physical Therapy Consulting to help meet the needs of more clients. I have been a guest lecturer for Rutgers University Blackwood Campus and Stockton University for their Pediatric and Pelvic Floor modules since 2016. I have also been a TA with Herman and Wallace since 2020 and have over 150 hours of lab instruction experience.
Rachel Kilgore, DPT, OCS, COMT, PRPC, PPCES graduated from Central Washington University with a Bachelor of Science (BS) in exercise science and a minor in nutrition in 2004 and completed her Doctor of Physical Therapy (DPT) at the University of Washington in 2007. Rachel practices in Seattle at Flow Rehab in the Freemont Neighborhood with Holly Tanner and focuses her patient care on orthopedics, female athletes, and women’s health conditions for bladder & bowel dysfunctions, pelvic, pain, pregnancy, and post-partum issues.
I have always been very particular about the precision of words. I have been known to ruminate about the origin, evolution, and application of words. As my husband always kindly says, I am an overthinker. This leads me to our nomenclature analysis for today, Diastasis.
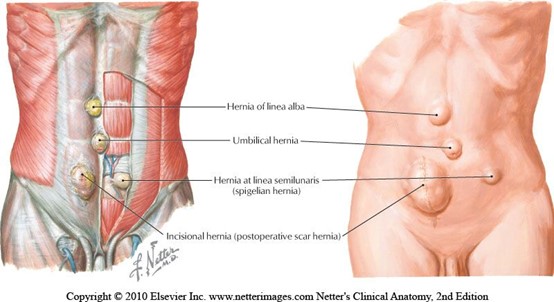 When teaching pregnancy and post-partum courses we always have healthy discussions about Diastasis Rectus Abdominus (DRA) as this is an important topic in the peripartum world. One question that always comes up is what is the difference between a hernia and DRA? If DRA is not a condition you deal with often in the clinic, it can be a bit confusing. According to the Merriam-Webster Dictionary diastasis means “an abnormal separation of parts normally joined together,” so DRA is often defined as a separation of the Rectus Abdominus muscles. I think the word separation is what causes the confusion. This word may lead some people to think there is an actual disruption of the abdominal tissue which is not the case. The rectus abdominus halves remain joined together by the linea alba. The linea alba is the tendinous raphe formed by interdigitating fascia of external/internal obliques and Transversus Abdominis. A DRA is an increase in the distance between the right and left Rectus Abdominus halves. If you stretch connective tissues (increase the distance between two ends), they may become thinner, lengthened, or weakened. A DRA is an increased distance between the right and left Rectus Abdominus halves that may result in lengthened, thinner, weaker tissue. In contrast, a hernia is an actual defect in the connective tissue. DRA and hernias are not the same thing; however, they can exist together.
When teaching pregnancy and post-partum courses we always have healthy discussions about Diastasis Rectus Abdominus (DRA) as this is an important topic in the peripartum world. One question that always comes up is what is the difference between a hernia and DRA? If DRA is not a condition you deal with often in the clinic, it can be a bit confusing. According to the Merriam-Webster Dictionary diastasis means “an abnormal separation of parts normally joined together,” so DRA is often defined as a separation of the Rectus Abdominus muscles. I think the word separation is what causes the confusion. This word may lead some people to think there is an actual disruption of the abdominal tissue which is not the case. The rectus abdominus halves remain joined together by the linea alba. The linea alba is the tendinous raphe formed by interdigitating fascia of external/internal obliques and Transversus Abdominis. A DRA is an increase in the distance between the right and left Rectus Abdominus halves. If you stretch connective tissues (increase the distance between two ends), they may become thinner, lengthened, or weakened. A DRA is an increased distance between the right and left Rectus Abdominus halves that may result in lengthened, thinner, weaker tissue. In contrast, a hernia is an actual defect in the connective tissue. DRA and hernias are not the same thing; however, they can exist together.
Let’s contrast these two conditions. Hernias can occur anywhere in the abdominal wall, whereas DRA is only at the midline. Hernia can strangulate intestines, but DRA does not as there is no hole or defect in the connective tissues. The only way to truly diagnose a hernia is by ultrasound. The only definitive treatment of a hernia involves surgery with closure of the hole, sometimes supported by mesh. Patients may elect to not have surgery if the hernia is small, is not painful, or if other conditions make surgery too risky. For diastasis, treatment rarely involves surgery. Hernias are disrupted fascia. Diastasis is lengthened, thinning, or weakened fascia.
 Diastasis Rectus Abdominus occurs commonly towards the end of pregnancy, with 66-100% of women having DRA by the end of the third trimester (Boissonnault & Blaschak, 1988; Mota et al, 2015). Mota et al. 2018 measured the distance between the two rectus halves in 84 primiparous women in the third trimester 2 cm below the umbilicus and found the average to be 49-79 mm. In contrast, a study of 150 nulliparous women (Beer et al.) showed the inter recti distance at that same point (2 cm below umbilicus) to be 16mm. However, DRA is not exclusive to the pregnant or postpartum person, they can exist in children and men as well.
Diastasis Rectus Abdominus occurs commonly towards the end of pregnancy, with 66-100% of women having DRA by the end of the third trimester (Boissonnault & Blaschak, 1988; Mota et al, 2015). Mota et al. 2018 measured the distance between the two rectus halves in 84 primiparous women in the third trimester 2 cm below the umbilicus and found the average to be 49-79 mm. In contrast, a study of 150 nulliparous women (Beer et al.) showed the inter recti distance at that same point (2 cm below umbilicus) to be 16mm. However, DRA is not exclusive to the pregnant or postpartum person, they can exist in children and men as well.
Another example of the word diastasis, where separation does not mean disruption, is with pubic symphysis diastasis. The words may be confusing. When a patient hears the word diastasis and is told it means separation, they may conclude they have a disrupted pubic joint. I think the definition of it from Stolarczyk et al. is much more descriptive and less likely to cause angst in a patient. “A pubic symphysis diastasis (PSD, diastasis symphysis pubis) is defined as excessive widening of the system of anatomical structures that make up the pubic symphysis (above the physiological norm of 10 mm), occurring during pregnancy or postpartum.”
This is another instance where the word separation may imply disruption when it just means increased distance.
Let’s return our thoughts to the title of this blog. I hope we are thinking about how the words we choose make our patients feel. Many of our patients receive a diagnosis and turn to the internet, where they may find confusing and even scary descriptions of their condition. If you were told that your abdominals had separated, doesn’t that sound scary? Would you feel nervous that your organs may fall out from your separated abdominals? I would have so many questions and fears! How will they get back together, what activities should I refrain from, can I even move? Wouldn’t the term separated make you feel scared to do anything? Think about the term separated shoulder, we hear it all the time in sports, we know it is a torn AC joint. There is an actual disruption of tissue, but DRA is not. As health care providers it is important that we use safe and encouraging words with our patients. Our role should be to educate them on their condition and make sure they understand the anatomy, physiology, and functional implications. We need to empower. The more a patient knows about their condition, the better choices they make regarding activity and lifestyle. Words are powerful.
References:
- Boissonnault, J. S., & Blaschak, M. J. (1988). Incidence of diastasis recti abdominis during the childbearing year. Physical Therapy, 68(7), 1082-1086.
- Mota, P., Pascoal, A. G., Carita, A. I., & Bø, K. (2018). Normal width of the inter-recti distance in pregnant and postpartum primiparous women. Musculoskeletal Science and Practice, 35, 34-37.
- Beer, G. M., Schuster, A., Seifert, B., Manestar, M., Mihic‐Probst, D., & Weber, S. A. (2009). The normal width of the linea alba in nulliparous women. Clinical anatomy, 22(6), 706-711.
- Stolarczyk, A., Stępiński, P., Sasinowski, Ł., Czarnocki, T., Dębiński, M., & Maciąg, B. (2021). Peripartum Pubic Symphysis Diastasis—Practical Guidelines. Journal of clinical medicine, 10(11), 2443.
Kelly Sammis, PT, OCS, CLT, AFDN-S is a physical therapist, educator of dry needling and all things pelvic, Pilates instructor, wife, and mama living and working in Parker, Colorado. She specializes in the treatment of male and female pelvic floor dysfunction, athletic injury/return to sport, sports performance, and persistent pain. Her formal education took place at Ohio University (2007) and The University of St Augustine for Health Sciences (2010). Kelly serves as the lead faculty developing and teaching dry needling and pelvic health courses nationwide. Kelly co-instructs the Herman & Wallace Dry Needling courses along with fellow faculty member Tina Anderson, MS PT.
Pelvic floor dysfunction (PFD) is a common and relevant condition that affects many patients worldwide. According to our evidence, PFD can affect approximately 20-25% of women and men in the United States1, contributing to decreased participation in preferred daily, work and recreational activities due to high incidences of lumbopelvic pain, abdominopelvic pain, incontinence, prolapse, and/or other urologic and urogynecologic symptoms.2 These symptoms have a significant impact on a person’s quality of life and mental health status.2
While PFD is common, the general public has not been fully educated that these dysfunctions are not normal. As clinicians, we have a duty to educate our patient population that PFD is not a normal, nor acceptable, part of the postpartum experience or aging process. These dysfunctions are very debilitating but are also very treatable.
Common, not normal. Common, but treatable.
Pelvic floor pathology comes to us as clinicians in a variety of diagnoses, etiologies, and presentations2. Patients are often referred to physical therapy with medical diagnoses such as chronic pelvic pain syndrome (CPPS), interstitial cystitis, irritable bowel syndrome, endometriosis, dyspareunia, pudendal neuralgia, bowel and urinary incontinence, and chronic prostatitis.3-5 Symptom presentation is quite varied but often will include bowel, bladder, and sexual dysfunctions. That being said, a multidisciplinary approach is crucial to tailor treatment specific to each patient’s pathology, symptomatology, and clinical presentation.6 Many of these patients have seen a variety of gynecologists, urologists, and gastroenterologists without successful symptom mitigation and are being referred to pelvic health practitioners as a last resort. This is unfortunate, as a primary contributor to these symptoms is the neuromusculoskeletal system…and who better to treat the neuromusculoskeletal system than rehabilitative clinicians?!
Multimodal practice is key.
A well-rounded, multimodal treatment approach that is tailored to meet the patient’s specific goals is an important step in successfully treating PFD. Patient education can be a very powerful modality, which many clinicians tend to overlook. Research suggests education may help to address central nervous system upregulation and may help to retrain the brain in how it is processing input.7,8 While it is incredibly powerful to be able to influence pain processing, it doesn't stop with education. As clinicians, we also need to provide non-threatening, nourishing input to the tissues.
Manual therapies may help to desensitize the peripheral nervous system and surrounding soft tissues by providing neural input to alter the source of the pain and disruption.9,10 These techniques, including joint mobilization, soft tissue release, myofascial techniques, tool-assisted therapies, or any other manual approach, are likely addressing local tissue issues that may be perpetuating chronic pain or tissue dysfunction.
Dry needling is another effective and efficient technique that pelvic health practitioners can utilize to modulate the central nervous system, peripheral nervous systems and local tissues, including the pelvic floor directly.10 Dry needling encompasses the insertion of solid filament, non-injectate needles into, alongside or around muscles, nerves or connective tissues with or without mechanical and/or electrical stimulation for the management of pain and dysfunction in neuromusculoskeletal conditions.
While the detailed mechanisms of dry needling are not well known, we have seen more and more evidence that has provided us with an understanding on how to best utilize this technique in our clinical practice. Overall, it is thought that dry needling may address hypersensitive neural structures and spinal segments5, enhance treatment of myofascial pain and trigger points in the pelvic floor and surrounding musculature, and assist in the facilitation and/or inhibition of abnormal muscle tone and motor recruitment patterns.10-23 Dry needling has the ability to assist in addressing bladder, bowel, and sexual dysfunction alongside addressing pain syndromes in our patient population that is impacted by PFD.
Dry needling is one of the most effective tools we have as rehabilitative practitioners to reset dysfunctional tissue, providing effective and efficient functional changes for our patients. Ultimately, we are able to facilitate a more balanced resting tone, healthy motor recruitment patterns, and optimal neuromuscular utility to re-establish ideal function in our patients. The power of the tissue reset that dry needling provides has changed my clinical outcomes for the better and has also positively impacted and changed the lives of many of my clients. Want to add this tool to your clinical practice? Check out our course offerings with Herman & Wallace:
- Dry Needling and Pelvic Health - Waco, TX - June 11-12, 2022
Dry Needling and Pelvic Health - Milwaukee, WI - September 17-18, 2022
Dry Needling and Pelvic Health - Hatfield, PA - October 1-2, 2022
Dry Needling and Pelvic Health - Madison Heights, MI - October 8-9, 2022
Dry Needling and Pelvic Health - Worcester, MA - November 12-13, 2022 - Dry Needling and Pelvic Health: Advanced Concepts and Neuromodulation - Salt Lake City UT - November 5-6 2022
References:
- Hallock JK. The epidemiology of pelvic floor disorders and childbirth: an update. Obstet Gynecol Clin North Am. 2016 March;43(1):1-13
- Messelink et al. Standardization of Terminology of Pelvic Floor Muscle Function and Dysfunction: Report from the Pelvic Floor Clinical Assessment Group of the International Continence Society. Neurology and Urodynamics. 2005;24:374-380
- Anderson R, Sawyer T, Wise D, Morey A and Nathanson B. Painful Myofascial Trigger Points and Pain Sites in Men with Chronic Prostatitis/Chronic Pelvic Pain Syndrome. The Journal of Urology. 2009;182:2753-2758
- Hahn L. Chronic Pelvic Pain in Women. Lakartidningen. 2001;98:1780-5
- Kotarinos R. Myofascial Pelvic Pain. Curr Pain Headache Rep. 2012;16:433.438
- Srinivasan A, Kaye J, Moldwin R. Myofascial Dysfunction Associated with Chronic Pelvic Floor Pain: Management Strategies. Current Pain and Headache Reports. 2007;11:359-364
- Moseley G. Widespread Brain Activity During An Abdominal Task Markedly Reduced After Pain Physiology Eduction: fMRI Evaluation of a Single Patient with Chronic Low Back Pain. Australian Journal of Physiotherapy. 2005;51(1):49-52
- Moseley G. A Pain Neuromatrix Approach to Patients with Chronic Pain. Manual Therapy. Aug 2003;8(3):130-140
- Baron et al. Peripheral Input and Its Importance for Central Sensitization. Ann Neurol. 2013;74(5):630-6
- Chou L, Kao M, Lin J. Probably Mechanisms of Needling Therapies for Myofascial Pain Control. Evidence-Based Complimentary and Alternative Medicine. 2012;11
- Chen J, Chen S, Kuan T, et al. Phentolamine Effect on the Spontaneous Electrical Activity of Active Loci in a Myofascial Trigger Spot of Rabbit Skeletal Muscle. Archives of Physical Medicine and Rehabilitation. 1998;79(7):790-4
- Cummings T and White A. Needling Therapies in the Management of Myofascial Trigger Point Pain: A Systematic Review. Archives of Physical Medicine and Rehabilitation. 2001;82(7):986-992
- Gerber L, Shah J, Rosenberger W et al. Dry Needling Alters Triggers Points in the Upper Trapezius Muscle and Reduces Pain in Subjects with Chronic Myofascial Pain. Physical Medicine and Rehabilitation. 2015;7(7):711-718
- Gunn C, Milbrandt W, Little A et al. Dry Needling of Muscle Motor Points for Chronic Low Back Pain: A Randomized Clinical Trial with Long-Term Follow-Up. Spine. 1980;5(3):279-291
- Hsieh Y et al. Dry Needling to a Key Myofascial Trigger Point May Reduce Irritability of Satellite MTrPs. American Journal of Physical Medicine and Rehabilitation. 2007;86(5):397-403
- Lewit K. The Needle Effect in the Relief of Myofascial Pain. Pain. 1979;6(1):83-90
- Shah J. Uncovering the Biochemical Milieu of Myofascial Trigger Points Using In Vivo Microdialysis. Journal of Musculoskeletal Pain. 2008;16(1-2):17-20
- Shah J, Danoff J, Desai M et al. Biochemicals Associated with Pain and Inflammation are Elevated in Sites Near to and Remote from Active Myofascial Trigger Points. Archives of Physical Medicine and Rehabilitation. 2008;89(1):16-23
- Sterling M, Valentin S, Vicenzino B, et al. Dry Needling and Exercise for Chronic Whiplash - A Randomized Controlled Trial. BMC Musculskeletal Disorders. 2009;10:160
- Tough E, White A, Cummings T, et al. Acupuncture and Dry Needling in the Management of Myofascial Trigger Point Pain: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. European Journal of Pain. 2009;13(1):3-10
- Tuzun E, Gildir S, Angın E, et al. Effectiveness of Dry Needling Versus a Classical Physiotherapy Program in Patients with Chronic Low-Back Pain: A Single-Blind, Randomized, Controlled Trial. Journal of Physical Therapy Science. 2017;29(9):1502-1509
- Hong C and Torigoe Y. Electrophysiological Characteristics of Localized Twitch Responses in Responsive Taut Bands of Rabbit Skeletal Muscle Fibers. Journal of Musculoskeletal Pain. 1994;2(2):17-43
- Puentedura E, Buckingham S, Morton D, et al. Immediate Changes in Resting and Contracted Thickness of Transversus Abdominis After Dry Needling of Lumbar Multifidus in Healthy Participants: A Randomized Controlled Crossover Trial. Journal of Manipulative and Physiological Therapeutics. 2017;40(8):615-623

My name is Christina Trautman, and I am the Owner of The Pelvic Floor Place in Vancouver, WA. I am 39 years old and have been a practicing Pelvic Floor Physical Therapist for almost 14 years. I did not just stumble upon this career, it saved me.
I started having pelvic floor issues at the age of 7, peeing my pants when I would laugh. I had no physical trauma or incident as to why this was happening so as a 7-year-old, this was obviously humiliating and so embarrassing. This continued throughout elementary and went into middle school. When I was 13 and first got my period, I literally could not put in a tampon because my pelvic floor and vagina was so tight. This was frustrating and very inconvenient for an active sport-playing high schooler especially because all my friends could. What was wrong with me? I often felt alone and had no one I could talk to about my issues. After pleading with my mom to take me to a gynecologist for this difficulty and debilitating periods, I finally went as a sophomore in high school. It was the worst pain and experience of my life. Not only was I cramping for days and sobbing from the pain, but she told me, “You just need to have a kid and all your pain and issues will go away.”
Thankfully, I didn’t listen to her as getting pregnant at 14 wasn’t exactly the story I wanted and literally I probably couldn’t have sex if I tried. I continued to leak with laughing, couldn’t use a tampon, had debilitating periods, and was scared to death to date anyone. No one I knew had any of the same issues I had, and it wasn’t really a conversation my mom wanted to have with me. So, I continued to feel alone and in a lot of pain.
I compensated with my body throughout high school and college and couldn’t see improvement until I had Pelvic Floor Physical Therapy in my sophomore year in college. I was working as an aide in a PT clinic and luckily, they had a great Women’s Health PT there who noticed I had some pelvic floor symptoms. I was treated by her for a few years on and off and saw a huge improvement in my pain, leaking, and weakness. She connected the dots on all my issues that really stemmed from anxiety and an out-of-whack nervous system that started as a young kid after my parents divorced at the age of 3. After several treatments, I could put a tampon in, I didn’t leak with laughing, and was starting to get stronger in my core and pelvic floor.
I knew I had to go to PT school to treat women who had similar issues, so they too didn’t feel alone, embarrassed, humiliated, and frustrated.
My first job out of PT school was with that same therapist who treated me during college in Beaverton, OR. I took a Herman & Wallace Women’s Health class on a weekend before graduating from PT school and started studying all about the pelvic floor along with studying for my boards. She mentored me and I started seeing Women’s Health clients on day 1 of work. I loved it. This was my calling.
I split my time at that fast-paced office and a smaller clinic in Scappoose, OR. I was there for 2 years treating about 25-30% of women’s health clients. During that time, I took 3 different Herman & Wallace courses along with other classes dealing with Women’s Health. Every time I took a class, I wanted more. I wanted more complex clients and more time to treat them. I started dating a guy who lived in Vancouver WA, who is now my amazing husband, and I was ready for a change, so I took a job at a Chronic Pain clinic working as their Pelvic PT Specialist in Vancouver WA. I learned a ton and got to work with a good friend of mine. However, every day on my schedule, I would get so excited for my Pelvic clients and bored with my other orthopedic clients. So, I started looking for a full-time Pelvic PT position.
My best friend was working at a Pilates-based PT/Chiropractic office in Portland and they were looking for a Pelvic Floor PT. Despite the early morning hours and the long commute, I took the job. I was there for about 2 years and loved it. It was so fun working with chiropractors and skilled PTs. It was slow-paced but challenging and I was trained in Pilates Based PT. After getting pregnant, I decided the commute at 5 am to Portland was going to be too much so I took part-time jobs in Vancouver where I lived. This is when I opened my clinic.
I knew I always wanted to be a business owner; it was just so daunting. So, during my pregnancy, I slowly started seeing a couple of clients a week at my house while working part-time at other clinics in the area. This was amazing. I loved being in control of my own schedule and treating how I wanted to. I was mostly treating incontinence, prolapse, and pelvic pain but due to being pregnant, I started to get more interested in pregnancy and postpartum.
On December 25, 2017, I had my first baby, a 5-hour labor that I worked my tail off for. I had a great pregnancy and was highly active and ended up having a quick first vaginal birth with a very quick recovery. I owe that to all the exercises, breathing, and meditation I did during my pregnancy. I had a small tear with a natural vaginal birth but healed quickly with treatments I did on myself and was able to have sex within a few months with a supportive partner. Thinking about where I started to this point was miraculous. I did suffer from a grade 1 rectal prolapse about 5 weeks post-partum as I was struggling with constipation and a crying infant. As you can imagine, this was very frustrating as a Pelvic Floor PT, but those symptoms improved after I applied what I knew to my diet and exercises for my pelvic floor to help with strength and support. I owe all my success to having a supportive team to help me through my pelvic floor issues, pelvic floor PT, and a supportive partner. After recovering and getting back to work, I started taking more classes and getting certifications in pregnancy and postpartum classes. Ooh, this was my happy place. Starting to treat clients when the issues were really starting for most women was what I wanted to do.
I continued to slowly grow my business over the next few years as well as work at clinics in the area. It was a nice split. Enter my second pregnancy and covid. I had a great pregnancy and tried to keep as active as I could and the stress as low as I could. I had a 3-hour labor with no complications and a very fast recovery. How did I go from not being able to put a tampon in to delivering an 8 lb. baby without tearing? Pelvic PT is how! I truly was so proud and amazed at what my body could do. After I had Noah, I slowly started increasing my clientele and eventually decided to go full-time with my business.
During the last 5-6 years, I kept thinking about the Pelvic Rehab Practitioner Certification (PRPC) and kept putting it off for different reasons. After my son was about 2 and no longer requiring as much of my attention, I started studying for the test and passed in November of 2022. Woohoo!
I was still seeing clients at my house 4 days and week and in January of 2023 decided I needed to be in a real office. So, I joined forces with a prenatal chiropractor and a midwife group, and we opened up all 3 of our women-owned businesses in Felida, a small neighborhood and up-and-coming area near where I live. I am now mostly full-time, but I am as busy as I want to be while keeping a flexible schedule with the kids. I still have to work on my exercises and am aware of my pelvic floor, but I am no longer suffering with pain with sex, leaking, or weakness. I rewrote my story and yes while having kids did help (I will never tell that gynecologist that however), it really was Pelvic Floor Physical Therapy that has allowed me to live a normal life.
BIO:
Christina Trautman, PT, DPT, PRPC received her bachelor’s degree in Life Science from the University of Portland and her Doctorate in Physical Therapy from Pacific University. Through her personal experience with pelvic floor dysfunction and her extensive training, she found a passion for Women’s Health therapy and went on to take the Pelvic Floor Series courses (now Pelvic Function) through Herman & Wallace and holds her Pelvic Rehabilitation Practitioner Certification (PRPC).
Christina has been treating and aiding women with pelvic floor dysfunction for over 12 years and recently received her PRPC certification, making her one of the most sought-after pelvic floor rehab specialists in the area. She has also received her Postpartum Corrective Exercise Specialist Certification, Pre- and Post-Natal Corrective Exercise Specialist Certification, STOTT Rehab Pilates Mat and Reformer, and is pursuing more classes in pregnancy and postpartum care. She also treats orthopedic conditions and has a background in NAIOMT, ASTYM, and other manual therapy and exercise certifications.
Christina specializes in treating pregnancy and postpartum care, pain syndromes, pelvic organ prolapse, incontinence, and how to restore balance in the pelvic floor. She focuses on holistic care with a gentle approach to treating the pelvis and structures within the body that alter the mechanics of the pelvic floor. She also offers pregnancy and postpartum training programs.
Christina is the creator of The Pelvic Floor PlacePelvic Floor Place, and her desire is to treat women dealing with pelvic floor issues as well as helping pregnant and postpartum moms rehabilitate after having babies.
In her free time, she enjoys spending time with her family, getting outside, and enjoys working out with pilates, yoga, barre 3, and CrossFit.

It's been four years since my pelvic floor bestie (fellow Lead TA Carly Gossard) convinced my introverted self to try my hand at teaching assistant. I was hesitant, to say the least. I had taught small lab groups at Stockton University and mentored many of my colleagues in different areas, including pelvic health, but a class of 50 people relying on me to guide them through their first pelvic exam experience…I was terrified. It was the weekend before the world shut down for COVID, so there was this underlying current of “What does the future hold” and “Should we steal the gloves and hand sanitizer?”
Flash forward to the present day. I consider myself so lucky to wear many hats for Herman & Wallace. That first TA experience sparked this love of being with the Level 1 students as they embark on their pelvic health provider journeys. When HW needed to shift to the satellite model, I was one of the first TAs to jump into that role. When Megan Chamberlain (herder of the TAs) asked for help building a Lead TA program, I gave her my list of suggestions (I may consider Leslie Knope from Parks & Rec a role model). One of my favorite things about HW is that they take feedback seriously. At one point, they realized they needed someone to track the patterns of that feedback and guess who got that job….ME!
In 2023, the HW team decided it was time to take that feedback and update the main series to be more…more inclusive, more advanced, more hands-on, more to take home immediately to clinical practice. I was quick to chime in as I had a lot of subjective data from years of review synthesis. We have been organizing, researching, considering, consulting, and revamping the main series, and the first two classes of the series launched in January 2024! As the series rolled out, I decided I needed to TA each class to feel and experience the changes.
I spent January 14th and 15th at Hunter College in NYC with 30+ students during the second run of Pelvic Function Level 1. It went just as amazing as I had hoped as I helped the content team build it. The precourse work laid the foundation for more inclusive providers, reviewed the basics, and set students up to be ready for more advanced and hands-on content in class. There was penile-scrotal anatomy in this course instead of participants having to dive deeper into the pelvic floor series to learn these structures exist. It took about 2 years of my pelvic health career for that to happen in a class for ME! Students came in with more comfort on what they were going to do in person. They also confirmed that the workbook was the thing that hands-on, visual learners dream of. They even noticed we used bigger fonts and included closed captioning.
If you’ve interacted with me at all, through TA experiences, classes, or watching me mic run at HWConnect 2023, you’ll see I’ve come a long way from being the shy wallflower in the back of a PF1. This January, in addition to being one of the teaching assistants for Pelvic Function Level 1 in NYC, I’m also one of the first “TA Takeover” guinea pigs. What does this mean? Probably more videos of me dancing with pelvic organs from iHeartGuts joining the internet! I do hope to show you a little glimpse into what it's like to take a class with HW. In all seriousness though, HW’s goal and mission to bring quality, accessible, and inclusive care to all individuals makes it easy for me to say yes and sign up for any adventure they propose.
In this brief blog, I hope to explore several lifestyle medicine strategies (sleep hygiene, stress management, social connectedness) and how they may be included in therapeutic interventions to improve clinical outcomes. Frates and colleagues define lifestyle medicine as "The use of evidence-based lifestyle therapeutic approaches, such as a predominately whole-food and plant-based diet, regular physical activity, adequate sleep, stress management, avoidance of risky substance use, and other non-drug modalities to treat, oftentimes reverse, and prevent the lifestyle-related, chronic disease that's all too prevalent."1 Figure 1, adapted from the American College of Lifestyle Medicine, outlines the six pillars of lifestyle medicine.

Figure 1. Components of lifestyle medicine
Sleep Hygiene in Patient Education
The following are some simple patient education strategies that may help patients improve sleep:2-5
- Establish a regular bedtime and waking hours (avoid or minimize "social jet lag" that may be due to work, school, or your personal schedule).
- Create a comfortable room that is cool, dark, and quiet.
- Sleep in a comfortable bed and make sure it's not too old.
- Use a supportive and comfortable pillow and ensure it's not too old.
- Eliminate nighttime caffeine and limit daytime caffeine.
- Do not wear tight or restrictive clothing during sleep
- Avoid alcohol within 3 hours of bedtime.
- Do not smoke or use nicotine.
- Eliminate/limit after-dinner and late-night snacking.
- Limit or avoid computer use and smartphone use near bedtime.
- Avoid intense exercise near bedtime. However, do exercise and be physically active during the day.
- Maintain a healthy body mass index (BMI).
- Avoid watching intense television shows before bedtime.
- Turn off the radio and television before going to sleep.
- Avoid bright light near bedtime, but do increase daytime exposure to sunlight.
- Consider reducing your fluid intake near bedtime to avoid (or minimize) getting up to go to the bathroom, but maintain adequate hydration during the day.
- Minimize sugar and salt intake near bedtime as it may cause increased trips to the bathroom.
- Learn strategies to reduce daily stress so it does not result in poor quality and quantity of sleep.
- Minimize a tense or stressful lifestyle since this may carry over into sleep.
- Embrace mindfulness before bedtime
- Consider meditating close to bedtime or using a body scan or progressive muscle relaxation technique.
- Consider tai chi, qigong, or yoga later in the day.
- Establish a bedtime ritual such as:
- One hour before going to sleep, shut down all phone and computer devices. Then you can either read a book or watch a funny television show (drama may be too stimulating).
- Five minutes before you go to sleep, brush your teeth and floss, wash your hands and face with lavender soap, and shut off all the lights before slipping into your cozy bed with gratitude and pleasant thoughts.
Stress Management Patient Education
The following are some simple patient education strategies that may help patients manage stress:6
- Try yoga, tai chi, qigong
- Use aromatherapy (such as lavender)
- Engage in outdoor physical activities such as walking, hiking, and biking
- Engage in outdoor activities such as gardening
- Participate in hobbies such as reading, pottery, painting, and playing music
- Play with pets
- Get a massage
- Get involved in social activities such as volunteering, coaching, and community dancing
- Listen to music
- Smile and laugh more by watching comedy movies or television shows
Social Connectedness Patient Education
The following are some simple patient education strategies that may help patients improve socialization and social connectedness to form nurturing and constructive relationships:7-13
- Attend local sporting events, music performances, or art and museum exhibits.
- Connect with family and friends locally or on Zoom.
- Connect with your physician, therapist, wellness, or fitness professional via telehealth-delivered services.
- Create or join a community garden club.
- Create or join a lunchtime walking, yoga, or tai chi club.
- Engage in conventional group exercises such as softball, volleyball, basketball, pickleball, paddle tennis, or tennis.
- Engage in mind-body exercises such as yoga, tai chi, or Pilates.
- Engage in work-related community activities and fitness programs.
- Engage in small conversations with cashiers and employees at various stores you visit.
- Engage with members at your community place of worship.
- Enroll in art-based community activities, such as art, dance, drama, music, poetry, pottery, or expressive writing classes.
- Enroll at a local or community college to take cooking, history, or astronomy classes.
- Get a library card and participate in book club events.
- Get involved in nature-based activities, such as bird watching, botanical garden and park visits, farmer's market shopping, forest bathing or hiking, gardening, or walks at a lake, river, or beach.
- Join a group, such as a local bicycling club, chess, or table tennis club, or participate in your favorite hobby.
- Join a gym or fitness center.
- Join self-help groups.
- Join social media platforms like LinkedIn, Facebook, Twitter, Instagram, or TikTok.
- Play with your pets.
- Volunteer at a community center, hospital, school, or library.
- Volunteer to coach sports or mentor students.
- Walk with a mall club or create one in your neighborhood
If you are interested in learning more about these topics and others, please see my course Integrative and Lifestyle Medicine Toolbox for Rehab and Pain Management with Herman & Wallace.
Resources for Clinicians:
Learn how to include integrative and lifestyle medicine into your clinical practice with these resources:
- Academy of Integrative Health & Medicine
- American College of Lifestyle Medicine
- American College of Preventive Medicine
- Institute of Lifestyle Medicine
- National Center for Complementary and Integrative Health
Instructor Bio:
 Ziya "Z" Altug, PT, DPT, MS, OCS is a board-certified doctor of physical therapy with 32 years of clinical experience treating musculoskeletal injuries. Z currently provides outpatient physical therapy in the home setting in Los Angeles, California, and serves as a continuing education instructor.
Ziya "Z" Altug, PT, DPT, MS, OCS is a board-certified doctor of physical therapy with 32 years of clinical experience treating musculoskeletal injuries. Z currently provides outpatient physical therapy in the home setting in Los Angeles, California, and serves as a continuing education instructor.
Z received his Bachelor of Science in Physical Therapy at the University of Pittsburgh in 1989, Master of Science in Sport and Exercise Studies in 1985 and Bachelor of Science in Physical Education in 1983 from West Virginia University, and a Doctor of Physical Therapy from the College of St. Scholastica in 2015. Z is a long-standing member of the American Physical Therapy Association and a member of the American College of Lifestyle Medicine. He has attended workshops in yoga, tai chi, qigong, Pilates, Feldenkrais Method, and the Alexander Technique.
Z is the author of the books Integrative Healing: Developing Wellness in the Mind and Body (2018), The Anti-Aging Fitness Prescription (2006), and Manual of Clinical Exercise Testing, Prescription, and Rehabilitation (1993). In 2020, he published the chapter Exercise, Dance, Tai Chi, Pilates, and Alexander Technique in The Handbook of Wellness Medicine. In 2021, he published the article Lifestyle Medicine for Chronic Lower Back Pain: An Evidence-Based Approach in the American Journal of Lifestyle Medicine.
References:
- Frates, B., Bonnet, J.P., Joseph, R., & Peterson, J.A. (2019). Lifestyle Medicine Handbook: An Introduction to the Power of Healthy Habits. Monterey, CA: Healthy Learning.
- Altug Z. Integrative Healing: Developing Wellness in the Mind and Body. Springville, UT: Cedar Fort, Inc.; 2018.
- Kryger MH, Roth T, Goldstein CA. Principles and Practice of Sleep Medicine (2 Volume set), 7th ed. Philadelphia, PA: Elsevier; 2021
- Matsuo T, Miyata Y, Sakai H. Effect of salt intake reduction on nocturia in patients with excessive salt intake. Neurourol Urodyn. 2019;38(3):927-933.
- Vitale KC, Owens R, Hopkins SR, Malhotra A. Sleep hygiene for optimizing recovery in athletes: review and recommendations. Int J Sports Med. 2019;40(8):535-543.
- American College of Lifestyle Medicine. Handout: Lifestyle stress reduction. American College of Lifestyle Medicine; 2019.
- Leavell MA, Leiferman JA, Gascon M, Braddick F, Gonzalez JC, Litt JS. Nature-based social prescribing in urban settings to improve social connectedness and mental well-being: a review. Curr Environ Health Rep. 2019;6(4):297-308.
- National Institutes of Health. Social Wellness Toolkit. Bethesda, MD: National Institutes of Health. Accessed on June 2022.
- Roland M, Everington S, Marshall M. Social prescribing - transforming the relationship between physicians and their patients. N Engl J Med. 2020;383(2):97-99.
- Choi NG, Pepin R, Marti CN, Stevens CJ, Bruce ML. Improving social connectedness for homebound older adults: randomized controlled trial of tele-delivered behavioral activation versus tele-delivered friendly visits. Am J Geriatr Psychiatry. 2020;28(7):698-708.
- Davidson KW, Krist AH, Tseng CW, et al. Incorporation of social risk in US Preventive Services Task Force recommendations and identification of key challenges for primary care. JAMA. 2021;326(14):1410-1415.
- Eder M, Henninger M, Durbin S, et al. Screening and interventions for social risk factors: technical brief to support the US Preventive Services Task Force. JAMA. 2021;326(14):1416-1428.
- Steinman L, Parrish A, Mayotte C, et al. Increasing social connectedness for underserved older adults living with depression: a pre-post evaluation of PEARLS. Am J Geriatr Psychiatry. 2021;29(8):828-842.
Integrative and Lifestyle Medicine Toolbox for Rehab and Pain Management

Course Dates:
January 21, 2023
Price: $125
Experience Level: Beginner
Contact Hours: 4.5
Description: This course was written and developed by Ziya “Z” Altug, PT, DPT, MS, OCS, a board-certified doctor of physical therapy with 32 years of experience in treating musculoskeletal conditions, Brief lectures on the research and resources and labs will cover a toolbox approach for creating clinically relevant pain, anxiety, depression, and stress management strategies using lifestyle medicine, integrative medicine, expressive and art-based therapies, and the impact of nature on health. Participants will be able to practice Tai Chi/Qigong, expressive and art-based therapies including Music, Dance, and Drama Therapy, nature and aromatic therapies, self-hypnosis, and self-massage.
Kristina Koch, PT, DPT, is a board-certified clinical specialist in women’s health physical therapy and a certified lymphedema therapist. Kristina has been treating pelvic health conditions in individuals of all ages and genders since 2001 and works in private practice in Colorado Springs, CO. She has served as a guest lecturer for the pelvic health curriculum at Regis University in Denver and for the 3rd year medical students at the University of Colorado, Colorado Springs campus. She is the creator of Pharmacologic Considerations for the Pelvic Health Provider.
Although it is not within the scope of practice for rehab therapists to manage medications, it’s important that we review patient medications during the initial evaluation and on an ongoing basis. Therapists have a duty to assess medications impact on treatment and patient outcomes and to ensure patient safety. The population is aging and many patients over the age of 65 are on more than 5 medications, increasing the risk of medication side effects, adverse drug reactions, and drug interactions.
Primary care providers spend approximately 14-17 minutes with a patient during a visit, and the patient gets about 5 minutes to discuss their concerns, leaving little time for medication reconciliation or discussion regarding medication side effects (Tai-Seale, McGuire & Zhang, 2007). As therapists, we tend to see our patients for longer periods of time and more frequently, giving the patient more of an opportunity to discuss their signs and symptoms. Additionally, patients referred for pelvic health issues are often seeing multiple specialty providers (Ob/Gyn, urology, urogynecology, pain management, etc.) for their care, and each one is typically prescribing medications, potentially leading to polypharmacy. Understanding a medication’s actions, its impact on therapy, the side effects, and potential adverse drug reactions, can help guide treatment and improve patient outcomes.
A recent patient example is a post-menopausal cisgender female, referred by her primary care physician, for urinary urgency and nocturia. Her past medical history was significant for breast cancer. Her medications included an aromatase inhibitor, antihistamine due to seasonal allergies, and Vitamin C. After reviewing her medications and history, I recommended a non-hormonal vaginal lubricant and within 2 weeks her symptoms were 80% improved. Understanding the side effects of her medications allowed me to educate the patient about the effects of her medication and how to manage her symptoms.
More and more patients are attending therapy through direct access. As the first point of contact for patients, it's imperative that rehab professionals have a foundational knowledge of the medications often prescribed to treat pelvic floor conditions, GI, GU, and reproductive health issues. The ability to have educated conversations with our patients and other healthcare providers involved in their care can greatly improve the quality of care and outcomes, and maintain patient safety. The ability to discuss medications, vitamins, and supplements or complementary alternatives, that can minimize side effects, have fewer impacts on quality of life, and enhance function is an integral part of comprehensive patient care.
Join Kristina on Saturday, January 7, 2023, for Pharmacologic Considerations for the Pelvic Health Provider. This one-day, remote course will discuss the importance of understanding pharmacology and medication review, the current research regarding the pharmacologic treatment of numerous pelvic and reproductive health conditions and their side effects, drug interactions, and non-pharmacologic alternatives that are available for pelvic and reproductive health. Registration information and additional details are available at www.hermanwallace.com. #hermanwallacepelvicrehab, @hermanwallacepelvicrehab
References:
Ciccone, C. D. (2007). Pharmacology in Rehabilitation. (4th ed.). F.A. Davis Company.
Tai-Seale, M., McGuire, T.G., & Zhang, W. (2007). Time allocation in primary care office visits. Health Services Research. 42(5), 1871-1894. Doi: 10.1111/j.175-6773.2006.00689.x
Janes, M., & Kornetti, D. (2017). Medications: defining the role and responsibility of physical therapy practice. https://www.fsbpt.org/Portals/0/documents/free-resources/WinterForum2017Medications.pdf?ver=pf8bn4ZwoorAAg1PECZLfw%3D%3D
Pharmacologic Considerations for the Pelvic Health Provider

Course Dates:
January 7, 2023
Price: $200
Experience Level: Beginner
Contact Hours: 7.5
Description: This seven-and-a-half hour, one-day remote learning course will discuss medications used for the treatment of pelvic floor and genitourinary conditions as well as common side effects of medications routinely used for pelvic floor dysfunction. This course will be taught by Kristina Koch, PT, DPT via Zoom. Medications for constipation and GI dysfunction, as well as pelvic pain conditions such as Vulvodynia, Chronic Prostatitis, and Endometriosis, will be covered. The course will also cover medications and side effects in Gender-Affirming Care for patients who are transitioning.