Holly Tanner is the Director of Education at Herman & Wallace and has curated and instructs the Male Pelvic Floor course. Male Pelvic Floor was first taught in 2008 and has since been expanded to include 22 contact hours. This current content includes 7 pre-recorded lectures and 2 full days of live lectures and labs, allowing more time for hands-on skills in examination and treatment. The schedule covers bladder, prostate, sexual health, and pelvic pain, and further discusses special topics like post-vasectomy syndrome, circumcision, and Peyronie’s disease.
Post-orgasmic illness syndrome (POIS) is a condition that encompasses a cluster of clinical symptoms. The literature most often reports this presentation in men as a response that occurs shortly after ejaculation and that lasts a period of days or even a week or longer. Symptoms may include transient, flu-like symptoms including, but not limited to headache, sore throat, general myalgia, exhaustion, and cognition that is impacted during the reaction. Understandably, people who experience post-orgasm illness often limit sexual encounters, demonstrate avoidance of sexual function, experience interference in relationships with partners, and report lost time from work and other activities. The diagnosis may be primary (occurring from first ejaculation experience) or secondary (acquired later in life.)
Despite the recognition that clinical presentation can be highly variable, diagnostic criteria have been described by Waldinger and colleagues in 2011 (Part 1) and are based on their study of 45 Dutch Caucasian men with POIS.
Preliminary diagnostic criteria for post-orgasmic illness syndrome include 1 or more of the following:
- Flu-like symptoms, fatigue, muscle weakness, feeling feverish, sweating, mood disturbances or irritation, memory and concentration difficulties, nasal congestion, watery nose, and/or itchy eyes.
- Symptoms occur immediately after or within hours after ejaculation
- Symptoms occur almost always, or in more than 90% of ejaculation events
- Symptoms last for 2-7 days
- Symptoms disappear spontaneously
There are various theories postulating the reason for developing POIS including the autoimmune-allergy hypothesis, cytokine and neuroendocrine disruption, and endogenous m-opioid receptors (orgasm uses large quantities of endogenous opioids). One of the primary reasons that immune reaction to a patient’s own semen has been a strong theory is because sexual activities without ejaculation often do not produce the reaction. Hyposensitization with autologous semen has proven beneficial as a desensitization therapy. (Waldinger et al., 2011, Part 2) Other treatments that may be used include antihistamines, SSRIs, benzodiazepines, and NSAIDs. Comorbidities of POIS reported by Natale and colleagues (2020) include erectile dysfunction, allergies, chronic pelvic pain, autoimmune conditions, and depression and anxiety.
From the standpoint of pelvic rehabilitation, there is much to offer to alleviate symptoms and promote function in patients who have POIS. Genitopelvic pain during or after ejaculation, urinary hesitancy, and difficulty with bowel movements can accompany the syndrome - all complaints that warrant evaluation typical of any patient who has abdominopelvic dysfunction. In the men who have presented to me with this diagnosis, a period of sexual dysfunction including premature ejaculation was described prior to developing POIS. One patient, in particular, described a period of a decade or more of suppressing sexual desires, including masturbation, due to beliefs in his community. When he did masturbate for the first time, he developed post-orgasm illness immediately. I have also observed a tendency to report hypersensitivity to touch, with any palpation to the lower abdomen or groin area causing significant discomfort, and even spontaneous erection or orgasm that was difficult for the patient to manage. In the few cases I have seen, abdominal and pelvic muscle dysfunction was present, and patients responded favorably to manual therapy, education, breathing, and self-management with the use of thermal therapies and self-treatment for soft tissues. It is likely that a combination of medical management, as well as rehabilitation efforts, will provide the best recovery, as anyone who develops fear of an activity usually benefits from learning how to prepare for said activity by addressing concerns prior to, during, and after the activity. Addressing the nervous system response to ejaculation can be part of the rehabilitation process, and a referral to a mental health professional may also prove beneficial in managing the anxiety that often accompanies post-orgasm illness syndrome.
References:
- Abdessater, M., Elias, S., Mikhael, E., Alhammadi, A., & Beley, S. (2019). Post orgasmic illness syndrome: what do we know till now?. Basic and Clinical Andrology, 29(1), 1-6.
- Le, T. V., Nguyen, H. M. T., & Hellstrom, W. J. (2018). Postorgasmic Illness Syndrome: What do we know so far?. Journal of Rare Diseases Research & Treatment, 3(2).
- Nguyen, H. M. T., Bala, A., Gabrielson, A. T., & Hellstrom, W. J. (2018). Post-orgasmic illness syndrome: a review. Sexual Medicine Reviews, 6(1), 11-15.
- Waldinger, M. D., Meinardi, M. M., Zwinderman, A. H., & Schweitzer, D. H. (2011). Postorgasmic illness syndrome (POIS) in 45 Dutch Caucasian males: clinical characteristics and evidence for an immunogenic pathogenesis (part 1). The journal of sexual medicine, 8(4), 1164-1170.
- Waldinger MD, Meinardi MM, Schweitzer DH. Hyposensitization therapy with autologous semen in two Dutch caucasian males: beneficial effects in Postorgasmic illness syndrome (POIS; part 2). J Sex Med. 2011a;8(4):1171–6
- Waldinger, M. D., & Schweitzer, D. H. (2002). Postorgasmic illness syndrome: two cases. Journal of Sex &Marital Therapy, 28(3), 251-255.
Male Pelvic Floor Function, Dysfunction and Treatment - Satellite Lab Course
Price: $695 Experience Level: Beginner-Intermediate Contact Hours: 22
Description:
The course introduces valuable concepts in pelvic health including urinary and prostate function, chronic pelvic pain, and sexual health. For therapists who have taken Pelvic Floor Function, Dysfunction, and Treatment Level 2A, the Men’s Pelvic Health Course expands on the men’s pelvic health topics introduced in Pelvic Floor Level 2A. This continuing education course is also created at an introductory level, covering topics such as internal rectal pelvic muscle examination, so that a therapist who has not taken prior pelvic floor muscle function coursework can attend. It is expected that participants will only register for satellites in which they are within driving distance, and adhere to all state and local COVID guidelines, including wearing a mask at all times during the course.
Urinary dysfunction such as post-prostatectomy incontinence, benign prostatic hypertrophy, urinary retention, and post-micturition dribble are discussed in this class. Because urinary incontinence is a potential consequence following prostate surgery, risk factors, pre-surgical rehabilitation, and post-surgical intervention strategies following prostatectomy are instructed. The medical aspects of prostate cancer testing are also clearly described, including prostate-specific antigen (PSA) testing, Gleason scores, and any recent updates in recommended medical screening.
Although most men diagnosed with prostatitis do not have a true infection, prostatitis remains a common diagnosis within chronic pelvic pain. The Men’s Pelvic Health course explains typical presentations of prostatitis-like pain, evaluation techniques, and evidence-informed intervention techniques. Other pelvic diagnoses are covered, such as Peyronie's Disease, testicular and scrotal pain, penile pain, and pelvic floor muscle-related conditions. Men who experience pelvic muscle dysfunction including pain or weakness are at risk for sexual dysfunction. Participants will be able to describe the relationships between pelvic muscle function and men’s sexual health, including the evidence that demonstrates pelvic muscle rehabilitation's positive impact on erectile function. This continuing education course includes lectures and labs, including external and internal muscle mapping and neuro-myofascial treatment techniques.
Next Course Date: October 22-23, 2022
Satellites:
- Self-Hosted
- Virginia Beach, VA
- Downer's Grove, IL
- Baltimore, MD
- New York City, NY
- Omaha, NE
- Leesburg, FL
- Smyrna, TN
Alyson Lowrey, PT, DPT, OCS is the co-instructor for the H&W course Pain Science for the Chronic Pelvic Pain Population - Remote Course alongside Tara Sullivan, PT, DPT, PRPC, WCS, IF. Alyson treats the pelvic floor patient population through an orthopedic approach, working closely with pelvic floor specialists.
Pain neuroscience education (PNE) is the explanation of the neurophysiological changes in the central nervous system in patients with chronic pain. It includes how the nervous system functions and factors that influence its function such as social, psychological, and environmental factors. Pain neuroscience education aims to increase the patient’s knowledge about pain, decrease the threat of pain, and allow the patient to reconceptualize pain from a biopsychosocial perspective.
As a clinician seeing a patient with chronic and complex pain, it can be very daunting trying to determine how much education you should give the patient. Patients are generally very invested in improving their quality of life and therefore invested in learning how to treat their pain. Using techniques such as motivational interviewing is one way to determine if a patient is receptive to new information about pain and how to deliver that information. Education about pain needs to be varied and tailored to each patient based on their prior knowledge and perceptions, learning styles, their language, and their health literacy.
When a patient has an increased understanding of their pain and how their nervous system works, it can change their perspective about their pain by decreasing the threat value of their pain. PNE is the first step in the process of increasing a patient’s pain thresholds during exercise and functional activity. When patients no longer fear their pain as a sign of tissue damage, they can become empowered to re-educate their nervous system and pain processing centers in their brain. As providers, we are able to do this in several ways. We can do this by helping build new coping strategies and thought processes around their pain and dispelling misconceptions about their pain and physical ailments. We can suggest lifestyle and movement modifications that allow for more functional movement that doesn’t increase their pain activation centers. We can also adjust and modify our treatment plan around the patient's needs for success at each session. Consistently being a voice of encouragement, empowerment, and validation is also a very important component of PNE and our treatment as clinicians for our patients with chronic pain.
Pain Science for the Chronic Pelvic Pain Population - Remote Course
Course Date
October 8th-9th
Description
This course provides a thorough introduction to pain science concepts including classifications of pain mechanisms, peripheral pain generators, peripheral sensitization and central sensitization in listed chronic pelvic pain conditions; as well as treatment strategies including therapeutic pain neuroscience education, therapeutic alliance, and the current rehab interventions' influence on central sensitization. The rehab professionals who attend will be provided the understanding and tools needed to identify and treat patients with chronic pelvic pain from a pain science perspective. Lecture topics include the history of pain, pain physiology, central and peripheral sensitization, sensitization in chronic pelvic pain conditions, therapeutic alliance, pain science and trauma-informed care, therapeutic pain neuroscience education, the influence of rehab interventions on the CNS, and specific case examples for sensitization in CPP.

Amanda Davis, PT, DPT, PRPC can be found online at https://www.makeandmanifest.com/. She has generously shared her recent blog with The Pelvic Rehab Report. "Got 30 Minutes? 4 Underestimated Daily Practices to Make Your Lunch Break More Life-Giving" can be found in its original post on her website here: http://www.makeandmanifest.com/blog-lunchbreak/.
Hey there, I'm Amanda. Pelvic rehab therapist, endo warrior, girl mama (despite that whole endo thing), and creator of this space where I'm sharing the story of practicing what I preach and the wins and losses I gather along the way. I love early morning espresso, podcast binging, yoga pants, and scrolling Pinterest for my next obsession (heyyyy fellow libras!). My mission is to help women see the difference between "common" and "normal" and to take their physical, mental, and emotional health beyond the "that's just the way it is" mentality.
Hats off to my fellow 9-5ers who head home after a long day to jump right into their 5-9. If you’re like me, that second “career” includes (but definitely is not limited to) caregiver, dog walker, master gardener, professional organizer, chef, and housekeeper to name a few. Add in friendships that need energy, relationships that need time, those hobbies you swore you’d keep alive, and self-care you promised yourself you’d do…aaaaand the whole multi-passionate, multi-talented, multi-hyphenate thing can get overwhelming quick.
After a glorious five-month maternity leave, I’ve officially been a working mom for a year. I love my job and I love my girl, and while trying to fit both in a 24 day is challenging and exhausting, it’s what’s right for me in the season I’m in. Plus there’s something about pursuing my calling outside of the home and knowing Sloan’s watching me do it.
RELATED POST: 9 Ways to Practice Self-Love as a New Mom on Maternity Leave
We’ve all chased that ultimate goal of a *perfect* balance and ~seamless~ blend between work and home, but in full disclosure, I’ve gotta tell ya— it’s hard for me to do. I’ve found myself coming home drained, dying for a break, wishing I could just lock myself in a quiet room, and feeling guilty for all of the above. Being with my daughter is the best part of my day, but I’m often just too depleted to enjoy it.
Maybe you can relate? Maybe you’re also trying to work to live but find those words flipping themselves around more than you care to admit.
I recently took an online course called Boundaries, Self-Care, and Meditation for the Pelvic Rehab Therapist, Part 1 (part 2 is on June 12). As a PT I’m required to take continuing education to keep my skillset relevant and knowledge fresh, but the pending burnout I shared with you above led me to [this] course instead. To put it simply, it was [insert explosion sound here] mind-blowing; and call me dramatic, but I consider my practice, my patients, and myself as a person and professional forever changed because of it.
While I could write at least ten posts on all the things I learned in this class, the concept that’s been most life-altering for me was how I spend my lunchtime. Yep!…just a few tweaks to those 30 minutes mid-day and not only are my afternoons more pleasant and productive, but I’m going home refreshed, renewed, and ready to spend my time and energy on alllllllllll the other people and things that mean the most to me.
RELATED POST: Your Day Starts at Bedtime: 25 Easy Habits for a Better Night’s Sleep
What you’ll find next is how I structure my lunchtime for life-giving success— a strategy that serves me most. We all have different work environments, different physical and mental needs, and different priorities. As long as your cup feels full(er) at the end of your break, I can confirm you’re doin’ it right.
SHUT YOUR DOOR
I fully realize that not everyone has an office door they can shut during lunchtime, but as long as you can get somewhere semi-quiet and remotely alone, that should do the trick (heck…I’ve been known to go out to my car in a pinch). Creating a calm and centered environment has proven paramount to taking a true “break” from the day and will make all of my recommendations to follow that much more enjoyable.
If you’re worried about appearing “selfish” or “standoffish”…I was too. But after a week’s worth of lunches behind a closed door, I realize the positives of this practice far outweigh the negatives I was creating in my head. I’m still a team player. My coworkers still know where I am if they need me. But I’m a better colleague the other eight hours of the day when I take these 30 minutes to myself, and to my knowledge, there have been no complaints so far.
STOP TO EAT
To my fellow multi-tasking queens— if you only read one part of this post, let [this] be it as I believe this one change has made the biggest difference.
I used to spend my lunch catching up on paperwork, tending to emails, paying bills, online shopping, and then resort to scrolling social media if all of that was done. But I was eating during all of it and realized that not only was it taking me twice as long to complete tasks, but I wasn’t tasting, appreciating, or ultimately enjoying my food, all huge components of appetite, digestion, and ultimately nutrition and health.
My lunches aren’t anything fancy; in fact, 99% of the time they’re leftovers from earlier in the week (helloooooooo my trusty 3-day-old grilled chicken). But stopping to eat with intention and nothing other than a little music or podcast playing in the background has surprisingly, but positively, affected how much I consume, how my gut feels afterward, and the amount of energy I have for the rest of the day.
PS- What you eat can make a huge impact here too. I aim for whole, quality foods full of healthy fats and filling proteins to set me up for success. I’m someone who can eat the same thing again and again, so you’ll typically find my lunchbox full of that good ol’ grilled chicken, boiled eggs, fruit, cheese, and rice noodles if I’m feelin’ feisty.
LEARN
On top of that podcast I have playing while I eat, I’ve started spending ten to fifteen minutes learning during lunch. I literally set a timer, pull out a book, and read about something that fuels my brain.
In order to make these minutes a 10/10, here’s a few tips to uplevel the experience:
- Get comfortable. Find a place to prop your feet up or lean that car seat back (this is in part why I set a timer…juuuuuuuust in case I fall asleep). Have water nearby, a blanket tucked away if it’s cold, and don’t hesitate to indulge in all the ways even if for just a short period of time.
- Read about something unrelated to your occupation. For instance…I’m a pelvic rehab therapist but you won’t see me catching up on the latest research in anatomy and physiology. I typically grab a book on self-improvement, business and marketing, or homesteading, and my brain feels so much more recharged when it gets to focus on something that builds me up as a passionate person outside of my profession.
- Use a physical book. Seriously…no kindle, no phone apps, no audiobooks. Chances are you’re looking at a screen, listening to people talk, or a combo of the two all day long. Digging into an actual hard copy will access other parts of your brain that you may not be tapping into as regularly and result in faaaaaaaar more feel-good-ness.
When I became a mom I went from devouring a few books a month to being able to count my yearly reads on one hand. Reading on my lunch break has made me excited to learn again and reminded me of who I am outside of motherhood too (in turn making me a better mama). Even if reading isn’t your “thing”, at least give this one a try. Bonus if you utilize your local library because their books just smell better and we’re going for indulgent here…remember?
MOVE
Eat…ten minutes. Learn…ten minutes. If you’re like me and have ten more minutes to spare, then I encourage you to move your body with that time. While the options are endless, I try to avoid sweating too much in the middle of the work day, so walking, stretching, and even deep breathing exercises are more my speed. Whatever you decide to do, make sure you have the shoes, yoga mat, or whatever it is you need ready to go.
RELATED POST: Easy + Impactful Ways to Use Your Time Confetti to Improve Your Pelvic Floor Health
Not only does research show that movement improves your mood and elevates your energy, but there are also the physical benefits (duh!) and mental resilience that comes with knowing you’re taking care of yourself when you could be doing something else. Once fearful of wasting precious energy, I now consider my mid-day movement the boost I need to ensure I’m ready to go when I get home because let me tell ya…one year olds don’t quit.
One look at my Pinterest boards and you’ll see I’m a girl who has a lot she wants to accomplish (I see you dream house, list of must-reads, vacation itineraries, and yummy recipes just dyyyyyying to be made). But with a 24-hour day divided in thirds between work, sleep, and “other”, I have to use my time wisely to see success in a life where I’m more often than not choosing the option of (D) ALL OF THE ABOVE.
I don’t mean to be dramatic, but hacking my 30-minute lunch has ~literally~ changed my life and I’m a better physical therapist, caregiver, dog walker, master gardener, professional organizer, chef, and housekeeper (to name a few) because of it. There’s a saying that if you can’t go big, go home, but this is an instance where you can’t underestimate the power of a few minutes spent intentionally where it counts.
I’d love to hear in the comments what you do for work, if these strategies work for you, and ways you’ve made them your own. And don’t hesitate to share this one with a coworker who could use these strategies too! Nothing makes me happier than picturing us all spending half an hour in that 11-2 time frame-filling our cups for full-day success. I have a feeling you’ll be surprised at the impact this can have, and I can’t wait to watch you grow one lunchtime at a time.
Boundaries, Self-Care, and Meditation - Part 2 - Remote Course - June 12, 2022
This course focuses on personal and professional growth for the participant, with a deeper dive into meditation and self-care practices. Yoga is introduced as a means of mindful movement and energy balance. Participants will learn to identify unhealthy relational patterns in patients and others, and skills on how to use language and boundaries to create shifts that keep the clinician grounded and prevent excessive energic and emotional disruptions. There is a lecture on using essential oils for self-care and possibly patient care. Learning new strategies to preserve energy, wellness, and passion while practicing appropriate self-care and boundaries will lead to helpful relationships with complex patients. This course also includes a discussion of energetic relationships with others as well as the concept of a "Higher Power". The discussion will also include refining life purpose, mission, and joy potential, unique to the individual participant. The goal is that the participating clinician will walk away from this experience equipped with strategies to address both oneself and one's patients with a mind, body, and spirit approach.
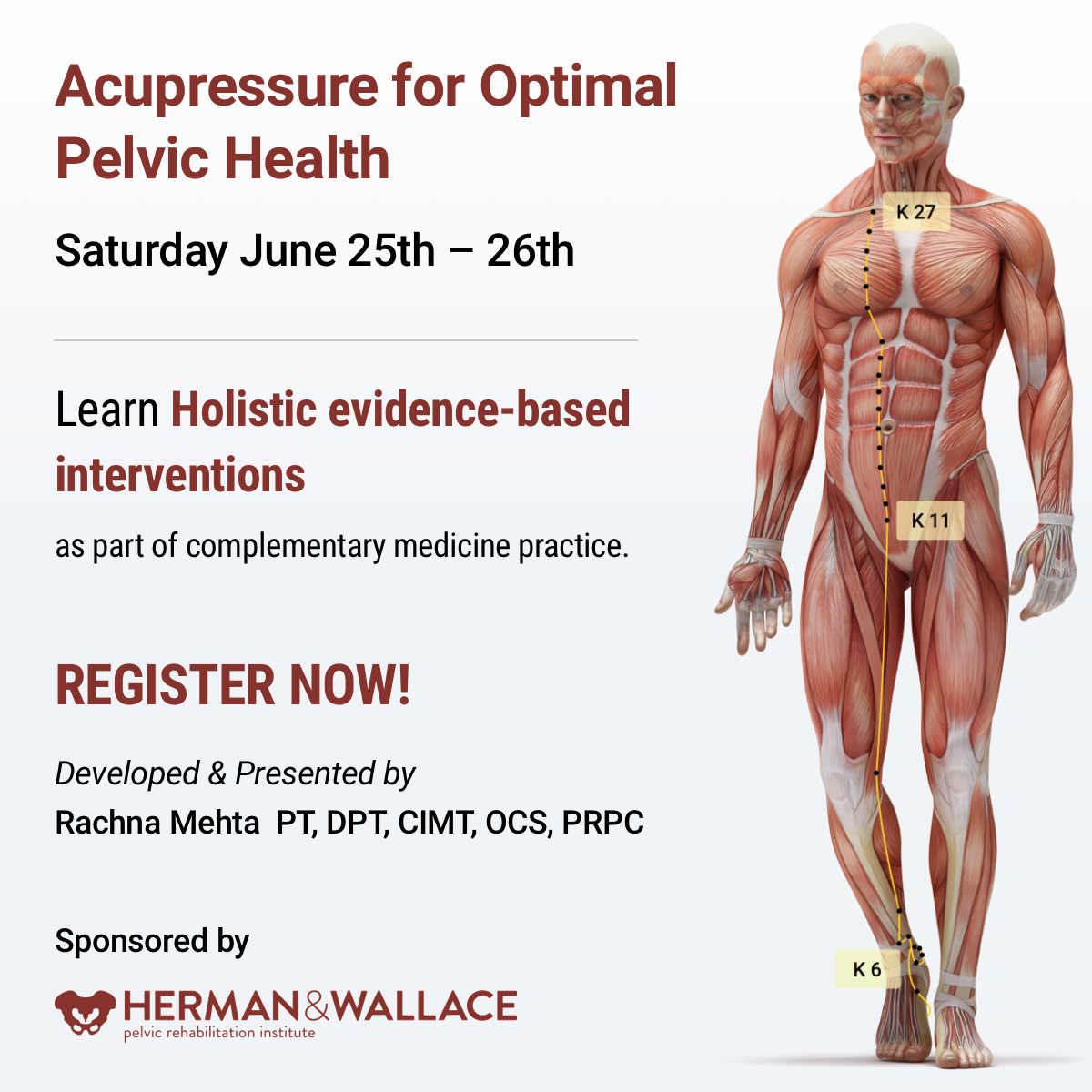
Rachna Mehta PT, DPT, CIMT, OCS, PRPC, RYT 200 has a personal interest in various eastern holistic healing traditions, and she noticed that many of her chronic pain patients were using complementary health care approaches including acupuncture and yoga. Her course Acupressure for Optimal Pelvic Health brings a unique evidence-based approach and explores complementary medicine as a powerful tool for holistic management of the individual as a whole focusing on the physical, emotional, and energy body.
There is worldwide concern over the increasing rates of pharmacologically induced labor, opioid use, and operative birth. Women are seeking holistic non-pharmacologic options to avoid medical and surgical interventions in childbirth which has led to the popularity of Complementary and Alternative Medicine (CAM) therapies. Despite CAM existing outside of conventional heath systems, a substantial number of women have been found to use CAM to manage their health during pregnancy1.
Among CAM therapies, Acupuncture and Acupressure have been found to be helpful for pregnancy-related symptoms such as nausea, breech presentation, and labor induction with post-partum recovery considerations as well. Acupressure has roots in Acupuncture and is based on more than 3000 years of Traditional Chinese Medicine (TCM). TCM supports Meridian theory and meridians are believed to be energy channels that are connected to the function of the visceral organs. Acupoints located along these meridians transmit Qi or the bio-electric energy through a vast network of interstitial connective tissue connecting the peripheral nervous system to the central viscera.
A systematic review published by Smith et al2 looked at the use of Acupuncture or Acupressure for pain management during labor. They noted that the pain women experience during labor can be intense, with body tension, anxiety, and fear making it worse. The data included a total of 3960 women and found that Acupressure may reduce pain intensity in women experiencing labor pain.
Another RCT published by Levett et al included 176 nulliparous women with low-risk pregnancies, attending hospital-based antenatal clinics. They incorporated six evidence-based complementary medicine techniques: Acupressure, visualization and relaxation, breathing, massage, yoga techniques, and facilitated partner support. Randomization occurred at 24–36 weeks’ gestation, and participants attended a 2-day antenatal education program plus standard care, or standard care alone.
The study found a significant difference between the two groups with the study group having decreased epidural use (23.9%) compared to the standard care group (68.7%). The study group participants also reported a reduced rate of cesarean section and length of the second stage among other measures.
An article published by Debra Betts3 discusses several key considerations for promoting physiological Labor with Acupuncture. Multiple studies have cited the effectiveness of Acupressure by stimulating these powerful Acupoints as well. The author states that the suggestion of Acupoints cited below are based on both her clinical practice and midwifery feedback and are by no means an exhaustive list. The practitioner is encouraged to explore Traditional Chinese Medicine to promote efficient physiological labor in women.
Key considerations for promoting natural physiological labor include:
Is the baby in an optimal anterior position? The author states “Women can become involved in their own treatment by learning proactive positioning. This involves a woman keeping her knees lower than her hips when sitting, in order to assist gravity in moving her baby into the best possible position. Bucket‑type seats such as car seats and comfy sofas, therefore, need to be abandoned in favor of birthing balls, sitting astride chairs (with the arms resting on the back).” Key acupuncture points that can be stimulated include Bladder 60 ( BL 60), Spleen 6 (Sp 6), and Bladder 67 (BL 67). Bladder 60 (BL 60) is considered an empirical induction point. Midwifery feedback suggests that this is a useful point for promoting an optimal position of the baby for birth. Bladder 67 (BL 67) is considered an extremely important point if the baby is not in an anterior position.
Is the woman emotionally prepared for labor? While most women have some level of underlying anxiety or fear about the approaching birth, it is essential to address any significant emotional disharmony. The hormone oxytocin is released several weeks prior to labor, initially stimulating uterine contractions at night, with increasing production then aiding the transition into labor. Stress hormones such as adrenaline and noradrenaline have a direct inhibiting effect on natural oxytocin release, and therefore play a very significant role in inhibiting contractions2. Key acupuncture points that can be stimulated include Kidney 1 (KD 1), Liver 3 (Liv 3), and Pericardium 6 (P6) among others. Kidney 1 (K1) is useful for women who are experiencing fear of induction or childbirth itself. Liver 3 (Lv 3) is helps in improving Liver chi. Pericardium 6 (P6) is helpful for nausea, regulating the heart and calming.
Is the woman physically prepared for labor? Women may be physically exhausted or have pre-existing physical conditions that, once addressed, will help to promote physiological labor2. Key acupuncture points that can be stimulated include Bladder 43 (BL 43) and Stomach 36 (St 36). Bladder 43 ( BL 43) is A point that tonifies and nourishes the Lung, Heart, Kidneys, Spleen, and Stomach. Stomach 36 (ST 36) is a useful point to reinforce if the woman is exhausted, due to its qi-tonifying and blood-nourishing properties.
Stimulating contractions: Debra Betts also notes that key points of the Bladder meridian that are located on the sacrum are crucial in initiating contractions. While Traditional Chinese Medicine (TCM) does consider some Acupuncture points like Large Intestine 4 (LI 4), Gall Bladder 21 (GB 21), and Spleen 6 (Sp 6) should not be stimulated in pregnant women, the opposite is true when we want to initiate labor and these points can be additionally used to assist in stimulating contractions.
Acupressure can also be used in the post-partum period for overall generalized well-being, promoting a sense of bonding with the baby, calm, and relaxation.
Acupressure can be used to stimulate key energy points also known as Acupoints in various meridians and as hands-on musculoskeletal specialists, we can use and teach this modality to our patients. Acupressure requires no equipment, is easy for clinicians to teach and for patients to self-administer when taught correctly, and is an empowering self-care tool to promote optimal health outcomes.
The course Acupressure for Optimal Pelvic Health focuses on powerful Acupressure points in key Meridians including the Kidney, Bladder, Spleen, and Stomach meridians. It also explores Yin Yoga as an integrative intervention with Acupressure. Yin Yoga, a derivative of Hath Yoga is a wonderful complimentary practice to Acupressure. Yin Yoga is a slow and calm meditative practice that uses seated and supine poses that are held for three to five minutes with deep breathing. It stimulates the energy flow through the meridian channels by creating tension along specific meridian lines.
This course is curated and taught by Rachna Mehta. To learn how to integrate Acupressure into your clinical practice, join the next scheduled remote course on June 25- 26, 2022.
References
- Steel A, Adams J, Sibbritt D, Broom A. The Outcomes of Complementary and Alternative Medicine Use among Pregnant and Birthing Women: Current Trends and Future Directions. Women’s Health. May 2015:309-323. doi:10.2217/WHE.14.84.
- Smith CA, Collins CT, Levett KM, et al. Acupuncture or acupressure for pain management during labour. Cochrane Database Syst Rev. 2020;2(2): CD009232.
- Betts, Debra. Inducing Labour with Acupuncture–Crucial Considerations. Journal of Chinese Medicine. 2009;90: 20-25.
- Atkins KL, Fogarty S, Feigel ML. Acupressure and Acupuncture Use in the Peripartum Period. Clin Obstet Gynecol. 2021;64(3):558-571. doi:10.1097/GRF.0000000000000636.
- Levett, Kate M., Smith, C.A., Bensoussan, A. & Dahlen, H.G. Complementary therapies for labour and birth study: a randomized controlled trial of antenatal integrative medicine for pain management in labour. BMJ Open, 2016 Jul 12;6(7):e010691. DOI: 10.1136/bmjopen-2015-010691.
- Schlaeger JM, Gabzdyl EM, Bussell JL, et al. Acupuncture and Acupressure in Labor. J Midwifery Women's Health. 2017;62(1):12-28. doi:10.1111/jmwh.12545.
Acupressure for Optimal Pelvic Health
Instructor: Rachna Mehta PT, DPT, CIMT, OCS, PRPC, RYT 200
Price: $450
Experience Level: Beginner
Contact Hours: 12.5
Course Dates: June 25-26, 2022 and October 15-16, 2022
Course Description:
This continuing education course is a two-day seminar that offers participants an evidence-based perspective on the application of Acupressure for evaluating and treating a host of pelvic health conditions including bowel, bladder, and pelvic pain issues. The course explores a brief history of Acupressure, its roots in Acupuncture and Traditional Chinese Medicine (TCM), and presents current evidence that supports the use of complementary and alternative medicine as an adjunct to western medicine. TCM concepts of Meridian theory and energy channels are presented with scientific evidence of Acupoints transmitting energy through interstitial connective tissue with potentially powerful integrative applications through multiple systems.
Lectures will present evidence on the use of potent Acupressure points and combinations of points for treating a variety of pelvic health conditions including chronic pelvic pain, dysmenorrhea, constipation, digestive disturbances, and urinary dysfunctions to name a few. Key acupoints for decreasing anxiety, and stress and bringing the body back to a state of physiological balance are integrated throughout the course.
Participants will be instructed through live lectures and demonstrations on the anatomic location and mapping of acupressure points along five major meridians including the spleen, stomach, kidney, urinary bladder, and gall bladder meridians. Key associated points in the pericardium, large intestine, small intestine, lung and liver meridians as well as the governing and conception vessels will also be introduced. The course offers a brief introduction to Yin yoga and explores Yin poses within each meridian to channel energy through neurodynamic pathways to promote healing across multiple systems. Participants will learn how to create home programs and exercise sequences and will be able to integrate acupressure and Yin yoga into their orthopedic and pelvic health interventions.
Special Considerations and Lab materials
The labs for this course will involve external whole-body palpation and mapping of acupressure points. Please wear fitted t-shirt and leggings or yoga pants for acupressure point mapping. Participants should buy a pack of 1-inch diameter white circle stickers to be used in Labs for mapping acupressure points.
Participants are encouraged to use a Yoga mat if available and any other props they may have at home including yoga blocks, small blankets, towels and pillows to be used in the guided Yin Yoga Lab portion of the course.
Recommended resources: It is recommended that participants purchase an Acupressure Point Chart for ease of following the course work and labs in this course. Since the accuracy of points and content may vary on different charts, it is recommended to buy a copy at https://acupressure.com/products/acupressure-charts/
Target Audience:
This continuing education seminar is targeted to rehabilitation professionals who use manual therapy as a treatment modality. Knowledge of acupressure points with specific anatomical landmarks will enable clinicians to add to their toolbox skills for treating a variety of pelvic health conditions related to the bowel, and bladder and treatment of pelvic pain.
Prerequisites:
It is recommended that the participants have a working knowledge of the functional anatomy of pelvic floor muscles as well as various associated pelvic health conditions. Pelvic Floor 1 through Herman & Wallace is strongly recommended.
Sarah Clampett, PT, DPT, is Head of Clinical Operations at Origin, a leading provider of pelvic floor and whole-body physical therapy with a special focus on pregnancy and postpartum. After studying Kinesiology and Psychology at the University of California, Sarah stayed on to earn her Doctorate of Physical Therapy. As a clinical leader at Origin, she’s as passionate about helping PTs love the work they do as she is helping patients feel good in their bodies.

Shortly after I started physical therapy school, I realized that being a physical therapist is a fantastic conversation starter. People’s eyes tend to light up when they hear I’m a PT because almost everyone has had an experience with physical therapy — and even if they haven’t, they’ve had an injury. They want to tell me about the physical therapy they did in high school for their scoliosis or that time they tore their ACL skiing. They even seek advice for that pesky low back pain that hasn’t fully resolved since throwing their back out six months ago.
I love to hear people’s stories and genuinely enjoy engaging in casual conversations about injuries. When I’m done explaining that core strength is important when dealing with back pain, I go on to say that while I started my career in ortho, I’m now a pelvic floor PT. That’s when one of two things happens: 1) They stare at me blankly, then quickly change the subject, or 2) Their eyes light up even brighter and they start asking questions. That’s when the conversation gets really fun. “What exactly do you do?” “What do you treat?” and “How did you get into that?”
Where My Passion for Ortho Started
I decided to go to PT school for a couple of reasons. I’ve always loved sports and consider sports a large part of my upbringing. (Fun fact: I only listened to AM sports radio until I was about 13). And, like many PTs, I discovered physical therapy as a patient. In my case, it was after injuring myself in high school playing volleyball.
I loved going to PT, not only because I was getting better — I loved seeing all the other patients getting better around me. It was a very sports-oriented PT clinic and my first and only experience with PT, so when I declared Kinesiology as my major and started my pre-PT coursework in college, I had my heart set on being a sports/ortho PT. It felt like the perfect fit at the time. I was a student athletic trainer for 2.5 years in college to learn as much as I could about the sports rehab world before heading into PT school.
Fast forward to my final semester and clinical rotation at PT school: I was at an ortho clinic with a large population of athletes. I loved it. After I graduated, I was hired as a PT at that same clinic and started my career as a working PT. I began working a few days a week to build my caseload with the plan to transition to full-time as my schedule filled. That clinic happened to also own a women’s health clinic that treated primarily prenatal and postpartum patients. A few weeks after starting, I was asked if I wanted to work additional days by filling in at the women’s health clinic. As a new grad who needed to pay rent, I said yes because more days meant more money. It was supposed to be temporary.
My Journey to Becoming a Pelvic Floor PT
As soon as I walked into the women’s health clinic, something clicked. I fell in love with the patient population and helping them feel better. I remember early on, a patient with such severe pelvic pain that they could barely walk to the bathroom. At their next visit, they said they could walk without pain again. The ability to help people going through pregnancy and postpartum felt especially meaningful. I spent a year and a half working in both clinics and then transitioned to treating women’s health full time.
After working in women’s health for a couple of years, I eventually got tired of referring my patients with pelvic floor conditions to colleagues who treated pelvic floor and decided it was time to start treating it myself. To be honest, I was hesitant at first and definitely nervous about taking my first course. But as soon as I started treating the pelvic floor, something clicked again.
Even more so than in the past, I connected deeply with my patients and their goals. Giving someone the confidence to leave the house without wearing a maxi-pad or carrying extra underwear because they’re no longer worried about leaking was amazing. So many people suffer in silence from pelvic floor disorders and are resolved to just live with them. I’m lucky enough to provide a safe space to talk about it and assure them that it can get better. How cool is that?
Advice for an Ortho PT Curious About Pelvic floor
Take a course! Just because you take the course does not mean you are committing to a career change. Even if you decide it’s not the right time to switch or you didn’t enjoy it as much as you thought you would, you’ll still learn valuable information that you can immediately incorporate into your practice. That overworked, stressed patient with lingering hip pain might need pelvic floor lengthening to get that last bit of pain to resolve.
Most ortho PTs who make the shift are nervous they won’t be able to use their ortho skills when treating the pelvic floor, and that simply isn’t true. My time in ortho has definitely shaped the pelvic floor PT I am today.
In ortho, you treat the whole body. If your foot hurts, you look at the knee, the hip, the low back, and how everything works together to figure out what’s causing the foot pain. Pelvic floor PT is no different. You must look at the whole body and figure out how all the parts are working together to get the results you need. I continue to use many of the same exercises now that I used back when I was working as an ortho PT.
Lastly, the pelvic floor is a group of muscles. If it’s weak, it needs to strengthen. If it’s overactive, it needs to lengthen. If it’s uncoordinated, it needs to be retrained. Yes, treating pelvic floor dysfunction requires special training, but at the end of the day, muscles are muscles.

This article was originally posted on the Medbridge Blog site: https://www.medbridgeeducation.com/blog/2021/11/six-actionable-ways-to-be-a-better-lgbtq-ally/.
Brianna Durand, PT, DPT earned her Doctor of Physical Therapy at Texas Woman’s University in Houston, TX. During graduate school, she led and co-founded PT Proud, a Catalyst Group within the Health Policy and Administration Section of the APTA, to improve the education, equity, and inclusion of LGBTQ+ patients, students, and clinicians. Brianna owns and operates Empower Physiotherapy, a private practice in Seattle. As a competitive powerlifter, Brianna enjoys working with strength athletes who experience pelvic floor dysfunction, especially stress incontinence. She is passionate about providing care to individuals in the LGBTQ+ community, including those undergoing hormonal/surgical transition. Brianna's additional clinical interests include prenatal/postpartum care for trans and gender-nonconforming folx and pelvic floor care for patients that are intersex. Brianna curated and teaches LGBTQ+ cultural competency for practitioners in her course - Inclusive Care for Gender and Sexual Minorities.
LGBTQIA2S+. Does it seem like that acronym is ever-growing? That’s because it is!
As our society evolves, more people are feeling safe and comfortable to live as their authentic selves, and every day there is more evidence to support that.
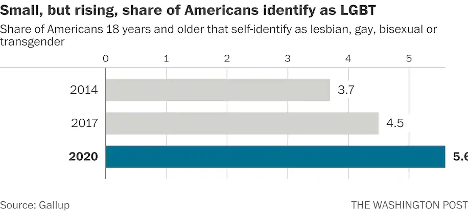
According to Gallup polls, the percentage of people in the U.S. that identify as lesbian, gay, bisexual, or transgender has increased to 5.6 percent.3 That is three times the entire population of Colorado! These numbers are even higher amongst younger generations—up to 20 percent in Gen Z and millennials by some estimates. In 2019, nearly 80 percent of surveyed Americans state that they personally know someone who identifies as LGBTQIA2S+ or queer.2 And while the word “queer” has a nasty history as a derogatory slur, it is increasingly used by folks in the LGBTQIA2S+ community to describe those who do not identify as cisgender or heterosexual.
What Is the Importance of Sexual Orientation or Gender Identity in Healthcare?
Recent years have provided a groundswell of awareness building around this community—from representation in entertainment, discussion about participation in athletics, and changes occurring at the legislative level. However, one area of society in which awareness is still lacking is in modern-day medicine, so let’s explore the significance of sexual orientation and gender identity (SOGI) as it pertains to healthcare.
As a medical professional, you may wonder “Can’t I simply treat all people the same?” While this idea may be filled with good intentions, the unfortunate reality is that we do not yet have access to this utopian future. There are real, measurable differences in the health of all marginalized communities, including gender and sexual minorities (GSM).
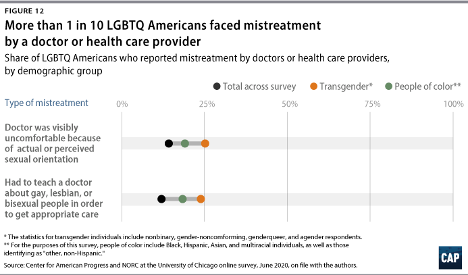
In 2020, 1 in 10 LGBTQIA2S+ Americans faced some form of mistreatment from a healthcare professional.1 These negative experiences strongly correlate with postponing or altogether avoiding medical care in the future, further contributing to the collective LGBTQIA2S+ fear of discrimination. The statistics are even worse when specifically looking at queer and trans people of color.
What Can You Do as a Healthcare Provider?
While the system and the education that trains our clinicians could benefit from a renovation, here are six actionable steps you can take now to facilitate a safer space for your LGBTQIA2S+ patients:
1. Recognize your own potential to cause harm.
As healthcare professionals, we have some degree of inherent privilege. With this privilege comes the capacity to inflict harm, intentional or not. While intentions matter, they do not supersede the impact your words or actions have on another. Assumptions matter, too. While assumption making is common and normal—an evolutionarily advantageous adaptation of the brain—they are not facts, and they are not harmless. Erroneous assumptions about a person’s gender or sexual identity by a medical professional can lead to behaviors that cause discomfort in and discrimination towards LGBTQIA2S+ patients and clients, even if inadvertently.
By recognizing the power differential that exists in the patient/provider relationship and the implications that come with it, we are likely to be more aware of our words and actions when they come up, and more willing to address them when they do. And by taking a position of genuine care and curiosity rather than assumption, we can affirm the relationship between the person whom we are helping and their body.
2. Update your language.
Always use the correct pronouns and name of the person with whom you are working. One easy way to do this is simply by mirroring the language they use when describing themself. However, if you are meeting someone for the first time, you may unintentionally use language that is not in line with your patient or client’s identity. For example, you may use someone’s dead name (the name assigned to them at birth) which may still be listed on their legal and medical documentation.
You can preempt this kind of unintentional harm by including areas for clarification on intake paperwork. This will allow you the opportunity to affirm the pronouns of the person in your care upon your first interaction. While pronoun affirmation may seem like a small action, it has shown to be effective in reducing suicidal ideation and depression.4 Another way to update your language for greater inclusivity is by using the term “spouse” or “partner” when inquiring if a patient has someone at home that can help with their activities of daily living or rehabilitation. Additionally, when referring to pregnancy, birthing, and postpartum care, practice saying “pregnant person” or “birthing parent” rather than “pregnant woman” or “mother.”
3. Speak up….even if the LGBTQIA2S+ person or target of the harm isn’t present.
Shaming someone’s behavior is unlikely to result in positive change or self-reflection. Instead, we can follow the steps of stopping, educating, and being proactive to foster learning in our colleagues. This kind of dialogue offers the opportunity for the individual to participate in the discussion by learning about their behavior, rather than feeling pushed out of the conversation which could limit their chance to grow.
- First, STOP the discussion or action taking place by intervening with “Those words can be hurtful.”
- Next, EDUCATE in lieu of asserting judgment. Proceed from a lens of curiosity. Asking the person “Do you know what those words mean?” or genuinely inquiring about their intention and understanding. Doing this will facilitate conversation and enhance one’s knowledge of their damaging actions, reducing the chance that they will repeat the harmful behavior.
- Finally, BE PROACTIVE by following up with resources for further learning such as GLMA, WPATH, or The Fenway Institute.
It is important to note the significance of taking this action even if the LGBTQIA2S+ person was not present for the encounter. This breaks the notion that harmful language is acceptable so long as the subject of the harm is not privy to it. If the LGBTQIA2S+ person is present for the encounter, it is best to first pull them aside to check in with them, make sure they are alright, and ask if they want your help. Some folks prefer to avoid drawing attention to themselves. It is also a skill of allyship to know when not to talk.
4. Be receptive to feedback.
When an LGBTQIA2S+ person, or a person from any marginalized group for that matter, corrects your language or behavior, practice saying “thank you” rather than “sorry” and avoid explaining yourself. It is a privilege to learn about oppression rather than to experience it for yourself. When someone corrects you, not only are they bravely honoring their authentic identities, but they are doing emotional labor on your behalf, and in the age of freely available information, it is never the responsibility of marginalized folks to educate others for free. These interactions are opportunities for personal growth—don’t let them pass you by!
5. Suggest practical changes to make the workplace more inclusive.
Does your workplace have gender-neutral bathrooms? Many LGBTQIA2S+, queer, and trans people avoid using public restrooms to avoid harassment and violence. Such aggressions can have very tangible consequences to their physical health, such as pelvic floor dysfunction. If there aren’t any inclusive restrooms in your workplace, make a suggestion to change that.
How inclusive are the brochures in your waiting room? Do the patient education materials that you provide to a patient after evaluation use language and imagery that include the LGBTQIA2S+ community? These are areas that can be improved upon with the suggested language updates we discussed above in action step two.
Are there symbols or graphics that will welcome GSM, such as safe space signs, flags depicting an upside-down rainbow triangle, or “all-gender” verbiage in lieu of gender-specific? Both would make easy additions that signal to patients they are in an inclusive space. However, it is important to distinguish the difference between saying a space is safe, and actually making a space safe. A space can only be safe if the entire team of providers and office staff are on board. Labeling a space as safe when it is not has the propensity to cause further harm. Be sure before these indicators are put up in your practice, everyone is ready to support such efforts.
6. Be prepared to mess up—but don’t let that deter you from trying.
Any etymologist will tell you that languages are living things that are constantly evolving. Developments such as these can make it challenging to stay current on which terminology is most beneficial to our growing society. Sometimes just the fear of making a mistake can be intimidating enough to discourage people from trying. What is most important is not how well you use updated language but that you are trying. Your effort matters, and it is what will move the needle in the right direction. Cultural responsiveness is not knowing every nuanced detail of every demographic group. Cultural responsiveness is being willing to reflect and modify your viewpoints when presented with information that differs from what you previously held to be true. Try to accept that just with learning any new skill, mistakes are bound to happen. When they do be prepared to learn, and then move forward with that new knowledge in mind.
References:
- Cusick Director, J., Seeberger Director, C., Woodcome, T., Oduyeru Manager, L., Gordon Director, P., Shepherd, M., Parshall, J., Santos, T., Medina, C., Gruberg, S., Mahowald, L., Bleiweis, R., Graves-Fitzsimmons, G., & Zhavoronkova, M. (2021, November 7). The State of the LGBTQ Community in 2020. Center for American Progress. Retrieved November 23, 2021, from https://www.americanprogress.org/article/state-lgbtq-community-2020/.
- Ellis, S. K. (2019). GLAAD Accelerating Acceptance 2019 Executive Summary. GLAAD.
- Jones, J. M. (2021, November 20). LGBT identification rises to 5.6% in latest U.S. estimate. Gallup.com. Retrieved November 23, 2021, from https://news.gallup.com/poll/329708/lgbt-identification-rises-latest-estimate.aspx.
- Russell, S. T., Pollitt, A. M., Li, G., & Grossman, A. H. (2018). Chosen name use is linked to reduced depressive symptoms, suicidal ideation, and suicidal behavior among transgender youth. Journal of Adolescent Health, 63(4), 503–505. https://doi.org/10.1016/j.jadohealth.2018.02.003
Additional resources:
- Schmidt, S. (2021, February 26). 1 in 6 Gen Z adults are LGBT. and this number could continue to grow. The Washington Post. Retrieved November 23, 2021, from https://www.washingtonpost.com/dc-md-va/2021/02/24/gen-z-lgbt/.
- Who Are We? Consortium. (n.d.). Retrieved November 23, 2021, from https://www.consortium.lgbt/intersex-inclusive-flag/.
Inclusive Care for Gender and Sexual Minorities
with instructor Brianna Durand, PT, DPT
When it feels overwhelming and nuanced, it can be tempting to avoid uncomfortable topics altogether. However, attendees for this course can expect to be gently guided into the sometimes confusing realm of gender and sexual orientation, and identity. This course will provide a safe space to ask all the questions about caring for LGBTQ+ patients and practicing the skills needed to help advance your practice. Although this course will cover pelvic floor physical therapy specifically, it is appropriate and useful for any medical professional as we all have patients in the LGBTQ+ community.

Blog by Deanna Vaughn, PT, DPT who practices at Core and Pelvic Physical Therapy Clinic in Conway, Arkansas, this article was originally located at https://whatsupdownthere.info/colorectal-cancer-the-gut-and-the-butt/.
Colorectal cancer refers to cancerous cells within the colon or rectum. Need a quick anatomy review? Keep reading then!
The colon is another name for the large intestine, which is the long tube (nearly 5 FEET!) surrounding the small intestines (that snaky, jumbled tube in the middle of our bodies, which you can see below in the picture). It’s comprised of segments: the cecum (the little pouch that joins the small intestine to the large intestine) in the right lower abdomen, the ascending colon starting at the right lower part of your abdomen (coming off the cecum), and up to about the right side of your ribcage; the transverse colon that loops underneath the stomach and ribcage from right to left; the descending colon that extends down from the left side of your ribcage to the lower part of your left abdomen; and then the sigmoid colon that loops (in an s-shape) along the lower abdomen to the center of the body. At the end of the colon is the rectum, which pretty much connects the colon to the actual anus/anal opening for wastes to leave the body.
That being said, colorectal cancer can affect any part or segment of the colon and the rectum. If you have a family history of colorectal cancer, or if you have an inflammatory bowel disease (like Crohn’s disease or ulcerative colitis), then you may be at a higher risk for colorectal cancer. Other risk factors are the same for virtually any other health condition – genetics, no regular physical activity, poor diet, tobacco use, high alcohol consumption, etc.
So how would we know if it’s colorectal cancer – or precancerous cells, and how do we decrease our risk?
That’s where screening comes into play! Just like how someone may see their gynecologist annually and undergo the PAP smear every 1-3 years to check for any gynecological cancer (like cervical or labial cancer), someone may see their colorectal or gastrointestinal (GI) provider to check for colorectal cancer or disorders. Regular screening takes place around age 45 (although a person may be screened earlier if they are at higher risk or had a previous history of cancer).
What does screening look like?
There are a few tests that screen for colorectal cancer. These tests include stool tests, flexible sigmoidoscopy, and colonoscopy.
Stool tests – This pretty much involves you taking a sample of your stool via test kit provided to you, and returning it to your doctor/lab, where your stool is checked for any blood or other abnormal findings.
Flexible sigmoidoscopy – A thin, short tube with a light is inserted into the rectum. This allows your doctor to see any polyps or cancer within the rectum and lower part of the colon.
Colonoscopy – This is like the sigmoidoscopy, but with a longer tube. The longer tube allows your doctor to check for polyps/cancer inside the rectum and the entire length of the colon. Your doctor can also remove some polyps during this procedure if indicated.
Most people without any symptoms, abnormal findings or outstanding personal or family history of colorectal cancer will have these screening tests performed anywhere from 5-10 years.
What are the symptoms?
This is not an exhaustive list, but some symptoms may include:
- Bleeding, pain, and/or discomfort within the rectum/anus
- Blood in stool
- Abdominal pain and bloating
- Nausea/vomiting
- Difficulty or incomplete bowel evacuation
- Hemorrhoids
- Altered bowel habits (such as sudden constipation, diarrhea, change in stool consistency)
Now what are our treatment options?
Besides preventative measures – such as getting regular physical activity, improving our diet, etc., treatment looks similar to any other cancer treatment. This may look like chemotherapy, radiation therapy, immunotherapy, and/or surgery. Surgery may be indicated to remove polyps/tumors, or parts of the colon or rectum to eliminate cancerous growths. Thankfully though, regular screening of the colorectal region can find precancerous/cancerous cells early. Oftentimes, such as during a colonoscopy, your colorectal provider may go ahead and remove polyps that are abnormal or deemed precancerous at that time!
Now what about pelvic physical therapy? Can it possibly help?
Well, this is another condition (like Pelvic Congestion Syndrome in the previous blog post), where pelvic physical therapy is not the initial go-to or main treatment option. Individuals with colorectal cancer vary in several ways depending on staging/severity and overall health. Once again, pelvic therapy is a nice resource to utilize if you’re needing or wanting ways to manage your bowel symptoms.
Ways that pelvic PT CAN help may include: Teaching appropriate toileting – positioning to straighten out the anorectal angle and allow stool to pass more easily from the rectum; mechanics, such as exhaling smoothly when pushing for a bowel movement to prevent straining; Improving pelvic floor muscle function (strength, endurance, coordination) so that your body can delay defecation as needed and calm down bowel urges; and overall promoting health bowel habits by supporting your nutrition and keeping bowel movements regular.
Whether or not you (or someone you know) have colorectal cancer, developing healthy and safe bowel habits is key to a better quality of life. Working with your doctor and/or your team of providers is important in making sure your needs are addressed, but feel free to reach out to your local pelvic PT if you want more resources or guidance – even things like, “So, how SHOULD I be pooping??”
References & Resources
Brenner H, Chen C. The colorectal cancer epidemic: challenges and opportunities for primary, secondary and tertiary prevention. Br J Cancer. 2018;119(7):785-792. doi:10.1038/s41416-018-0264-x
https://www.cancer.org/cancer/colon-rectal-cancer.html
https://my.clevelandclinic.org/health/diseases/14501-colorectal-colon-cancer
Kuipers EJ, Grady WM, Lieberman D, et al. Colorectal cancer. Nat Rev Dis Primers. 2015;1:15065. Published 2015 Nov 5. doi:10.1038/nrdp.2015.65
Leslie A, Steele RJC. Management of colorectal cancerPostgraduate Medical Journal 2002;78:473-478. http://dx.doi.org/10.1136/pmj.78.922.473
Mármol I, Sánchez-de-Diego C, Pradilla Dieste A, Cerrada E, Rodriguez Yoldi MJ. Colorectal Carcinoma: A General Overview and Future Perspectives in Colorectal Cancer. Int J Mol Sci. 2017;18(1):197. Published 2017 Jan 19. doi:10.3390/ijms18010197
You YN, Lee LD, Deschner BW, Shibata D. Colorectal Cancer in the Adolescent and Young Adult Population. JCO Oncol Pract. 2020;16(1):19-27. doi:10.1200/JOP.19.00153
This is the second installment in our 3 part pediatric blog series written by Amanda Moe DPT, PRPC treats women, men, and children with disorders of the pelvis and pelvic girdleAmanda enjoys assistant teaching with the Herman & Wallace Pelvic Rehabilitation Institute in her free time as well as working out, practicing yoga, and spending time with her family. You can find Amanda online at www.pelvicphysicaltherapyandmore.com and on Instagram @amandampelvicpt.
Just as Mora from @PracticallyPerfectPT mentioned in the previous blog post, Big Issues for Tiny Humans, pelvic health specialists treat pelvic floor and pelvic girdles for all humans of all ages. This blog post aims to introduce why pre-teens and teenagers could need pelvic floor therapy for pee problems!
Pelvic girdle-related dysfunction in young children often manifests as bowel or bladder complaints such as constipation, poo leakage (fecal incontinence or encopresis), and day or nighttime pee leakage (incontinence or nocturnal enuresis). Young children can be potty-trained with NO pee or poo complaints for several years then suddenly develop these very same symptoms in the pre-teen or teenage years! Occasionally there is a cause for the change in pee or poo symptoms such as trauma, the birth of a sibling, moving to a new city, divorce, or other changes in family situation. However, oftentimes there isn’t a signifying event attributed to the onset of these symptoms—which is where assessment and treatment from a skilled Pelvic Physical Therapist (or Occupational Therapist) may be beneficial!
Pediatric Pelvic Physical/Occupational Therapy
Pelvic Physical and Occupational Therapy in pre-teens and teenagers focuses on a whole-body assessment and treatment. Specifically, the Pediatric Pelvic Therapists will look at pelvic girdle influences on bowel and bladder complaints such as:
- Pelvic muscle tension
- Pelvic muscle strength
- Pelvic muscle coordination
- Abdomino-pelvic pressure management
- Load transfer
- Breathing
- Pelvic girdle strength
- Core coordination and strength
- Bladder and bowel habits
- Food and fluid contributors
Common Urinary Complaints in Pre-Teens and Teenagers
Potty-training regression can occur and is commonly seen in Pediatric Pelvic Therapy. Below is a list of other pee problems commonly seen in pre-teens and teenagers (often addressed in Pelvic Therapy).
- Strong urge to pee (urinary urgency)
- Frequent peeing
- Chronic UTI’s
- Urinary stream changes
- Nighttime bedwetting (nocturnal enuresis)
- Daytime leakage (urinary incontinence)
- Leakage with activity or sport (stress urinary incontinence or SUI)
Urinary leakage during sport or physical activity (SUI) can commonly arise in the pre-teen and teenage years. A recent systematic review determined that SUI occurs in 18-80% or an average of 48.58% of adolescent female athletes (7). While stress incontinence is common in women after childbirth, it doesn’t have to be considered “normal” for women OR children. This is where Pediatric Pelvic Therapy comes into play to determine the factors (such as those listed above) that are impacting a child's leakage during sport or activity!
The Lower Urinary Tract (LUT) symptoms listed above and specifically daytime pee leakage are prevalent in 10–17% of children (2, 4, 8). Gastrointestinal (GI) dysfunction such as constipation is commonly associated with these LUT dysfunctions in pre-teens and teenagers. Research has shown constipation in 22-37.5% of children with LUTS (3, 5) with an additional study reporting that greater than 50% of children with LUT symptoms had some type of functional defecation disorder (1). This is why Pediatric Pelvic Therapists often address the GI system when pre-teens and teenagers present with pee problems!
To learn more about the GI systems in adolescents and how these symptoms influence pee problems in Pediatric Pelvic Therapy, check out Dawn Scandalcidi's interview on Friday! Herman & Wallace also offers two pediatric courses featuring assessment and treatment of urinary and bowel functioning:
- Pediatric Incontinence and Pelvic Floor Dysfunction Remote Course - August 27-28th
- Pediatric Functional Gastrointestinal Disorders Remote Course - May 14-15th and November 12-13th
Resources
- Burgers R, de Jong TP, Visser M, Di Lorenzo C, Dijkgraaf MG, Benninga MA. Functional defecation disorders in children with lower urinary tract symptoms. J Urol. 2013 May;189(5):1886-91. doi: 10.1016/j.juro.2012.10.064. Epub 2012 Oct 30. PMID: 23123369.
- Kajiwara M, Inoue K, Usui A, Kurihara M, Usui T. The micturition habits and prevalence of daytime urinary incontinence in Japanese primary school children. J Urol. 2004; 171(1):403–7. [PubMed: 14665943]
- Loening-Baucke V. Prevalence rates for constipation and faecal and urinary incontinence. Arch Dis Child. 2007; 92(6):486–9. [PubMed: 16857698]
- Malykhina AP, Brodie KE, Wilcox DT. Genitourinary and gastrointestinal co-morbidities in children: The role of neural circuits in regulation of visceral function. J Pediatr Urol. 2017;13(2):177-182. doi:10.1016/j.jpurol.2016.04.036
- Muhammad S, Nawaz G, Jamil I, Ur Rehman A, Hussain I, Akhter S. Constipation in Pediatric Patients with Lower Urinary Tract Symptoms. J Coll Physicians Surg Pak. 2015 Nov;25(11):815-8. PMID: 26577968.
- Neveus T, von Gontard A, Hoebeke P, Hjalmas K, Bauer S, Bower W, et al. The standardization of terminology of lower urinary tract function in children and adolescents: report from the Standardisation Committee of the International Children's Continence Society. J Urol. 2006; 176(1): 314–24. [PubMed: 16753432]
- Rebullido TR, Gómez-Tomás C, Faigenbaum AD, Chulvi-Medrano I. The Prevalence of Urinary Incontinence among Adolescent Female Athletes: A Systematic Review. Journal of Functional Morphology and Kinesiology. 2021; 6(1):12. https://doi.org/10.3390/jfmk6010012
- Sureshkumar P, Jones M, Cumming R, Craig J. A population based study of 2,856 school-age children with urinary incontinence. J Urol. 2009; 181(2):808–15. discussion 815–806. [PubMed: 19110268]

This week The Pelvic Rehab Report is featuring faculty member (and senior TA) Mora Pluchino, teaching assistant Amanda Moe, and faculty member Dawn Sandalcidi on the topic of pediatric issues from infancy through adolescence. Our first guest blogger, Mora Pluchino, PT, DPT, PRPC has published two books. The first of which is titled The Poop Train: Helping Your Child Understand Their Digestive System. This is a rhyming, kid-friendly book to help children understand how their poop is made. It has resources in the back to help parents and caregivers manage a child's digestive system for optimal function including proper voiding positions, ideas for activities to help voiding, fiber recommendations, fiber-filled food options, and belly massage instructions. Her second book, Practically Perfect Pelvic Health 101: A Visual Tour of the Pelvic Floor is a visual tour of the pelvic floor to help all genders and all ages understand general pelvic health. You can find Mora online at https://www.practicallyperfectpt.com/ and on Instagram @practicallyperfectpt.
As a pelvic health specialist, I treat the pelvic floors for all humans of all ages. I am frequently asked the question “Why would a child need pelvic floor therapy?” The response is “So many reasons!”
Colic, gastroesophageal reflux disorder (GERD), and constipation are the top reasons for visits to a pediatrician in the first year (Indrio Et Al, 2014). As the mother of a child that struggled with all of these things, I can attest to the quality of life impact these diagnoses can create. A pelvic health specialist can help caregivers to manage these conditions with manual therapy, gross motor development assistance, and other infant care ideas to help manage the infant’s gastrointestinal system for better comfort and function.
Sillen (2001) reports that the neonatal bladder is controlled by neuronal pathways connecting with the cerebral cortex. The neonatal bladder function is characterized by small, frequent voids of varying volumes (Sillen 2001). Preterm infants had slightly different results thought to be due to an immature nervous system and this interrupted voiding disappeared for most as the children approached potty training age (Sillen, 2001). Still, infants born prematurely may be more at risk for pelvic floor issues!
What does this mean? There is a certain point in every child’s life where the bladder function, nervous system, and cognitive awareness match up. Ideally, this allows them to learn to hold and then void waste on a toilet. When toddlers are seen for pelvic floor issues, it is usually due to problems that arise during the potty training phase if they haven’t carried along with another pelvic floor issue from infancy. Pediatric pelvic floor issues, if not addressed early on, can continue on into preschool and elementary-aged children.
Pediatric Incontinence and Pelvic Floor Dysfunction, instructed by Dawn Salicidi, reviews the basics of pediatric pelvic floor treatment. Pediatric pelvic floor issues can be divided into three categories: storage, voiding, and “other.” Storage issues include things like: increased or decreased voiding frequency, continuous incontinence, intermittent incontinence, enuresis, urgency, nocturia, constipation, and encopresis. Voiding dysfunctions present with hesitancy, straining, weak stream, intermittency, and dysuria. Other pediatric pelvic floor issues include symptoms like excessive holding, incomplete emptying, post micturition dribble, spraying, and pain in the bladder/ urethral/ genital areas.
Pediatric pelvic health requires the knowledge and skills used for treating adults with the additional abilities to relate to the child and their caregivers to help them manage and improve their symptoms. There is no age limit on the benefits of pelvic floor treatment!
Join us on Wednesday for the next installment of the pediatric pelvic floor three-part series: Pee Problems in Pre-Teens and Teens by Amanda Moe, DPT, PRPC. Amanda has written a book, Pelvic PT for ME: Storybook Explanation of Pelvic Physical Therapy for Children. You can find Amanda on Instagram @amandampelvicpt. The series will conclude on Friday with an interview with long-time faculty member, Dawn Sandalcidi PT, RCMT, BCB-PMD. Dawn Sandalcidi is a trailblazer in the field of Pediatric Bowel and Bladder Disorders and can be found on Instagram @kidsbowelbladder.
References:
- Indrio F, Di Mauro A, Riezzo G, et al. Prophylactic Use of a Probiotic in the Prevention of Colic, Regurgitation, and Functional Constipation: A Randomized Clinical Trial. JAMA Pediatr. 2014;168(3):228–233.
- Sillén U. Bladder function in healthy neonates and its development during infancy. J Urol. 2001 Dec;166(6):2376-81.
Faculty member Christine Stewart, PT, CMPT began her career specializing in orthopedics and manual therapy and became interested in women’s health after the birth of her second child. Christine joined Olathe Health in 2010 to further focus on women’s health and obtain her CMPT from the North American Institute of Manual Therapy. She also went through Diane Lee's integrated systems model in 2018. Her course, Menopause Transitions and Pelvic Rehab is designed for the clinician that wants to understand the multitude of changes that are experienced in the menopause transition and how they affect the aging process.
Menopause. The M-word, the second puberty, is the final frontier of a hormonal roller coaster when there are twelve consecutive months with no menstruation. A time of celebration, right? No more cramps, hygiene products, menstrual cups, or moodiness – FREEDOM! Not so fast my fellow clinician!
The body goes through some serious, hormonal loop-the-loops leading up to the cessation of ovulation. Perimenopause is the stretch leading up to the final cycle and this stretch can feel like yoga on steroids. It can last TEN years, not including symptoms experienced after the transition takes place. Changes in cycle length, flow, anovulation, and yes, even ovulating twice are all stages of perimenopause. (Hale et al., 2009). These changes translate into symptoms: sleeplessness, brain fog, anxiety, palpitations, fatigue, painful intercourse, and joint stiffness are just a few things that can be experienced during this time (Lewis, 2021).
This transition can begin for patients during their mid-thirties, more commonly it begins during their forties, but eventually, all people that ovulate will experience it. For some, perimenopause can be much more challenging than after menopause. The perimenopause hormone guessing game begins. Some months, progesterone makes an appearance. The next month, mostly estrogen, and some months - neither are around very much at all. If there is an abrupt change in ovulation, such as with a complete hysterectomy, the symptoms will most likely be intensified due to the abrupt loss of hormones. (Gunter, 2020). Dealing with the changes of menopause can be challenging in a variety of ways (like a two-year-old wailing for a candy bar in the checkout line), but many things can help ease this transition.
With fluctuating hormones also comes changes to many systems in the body. Estrogen receptors are everywhere, and when hormone levels are changing, so does the body’s internal workings. Glucose metabolism, bone physiology, brain, and urogenital function are just some of the systems affected (Shifren et al., 2014). Perimenopause is not just a time of altered periods. It is also a critical time in a person’s health where an increased incidence of heart disease, diabetes, and bone loss can begin (Lewis 2021).
Preparing for menopause should be on our radar for patients in their twenties, thirties, and early forties before the process starts. Establishing healthy habits earlier instead of later can help for a more successful transition, however, it is never too late! Knowing the signs and symptoms of this phase can help us guide patients and ourselves to a better understanding of what is happening with the body in this adaptation. We can make recommendations on lifestyle, exercise, and meditation, as well as refer them to other knowledgeable providers when needed.
I have had countless patients sent to me for urinary frequency, incontinence, or painful intercourse who are in this transition, but no one has talked to them about what is happening to their bodies. You may be thinking to yourself, these patients have doctors. Why aren’t they getting the information from their physician? After all, these providers have had years of training. The reality is sometimes doctors do not receive the necessary education to treat menopausal patients.
In a survey of postgraduate trainees in internal medicine, family medicine, and obstetrics/gynecology, 90% felt unprepared to manage women experiencing menopause (Reid, 2021). Insert jaw drop here. As pelvic health providers, we can help to fill this knowledge gap and be a conduit to explaining the process. We can empower patients with education, treatments, and recommendations to flourish in this critical phase of life.
The menopause transition can be a time of great uncertainty. Not only are patients’ lives transforming as their children grow and their parents age, but their bodies are changing as well. We can ease their burden in this period of adaptation. By calming their fears through education, we can assure them that indeed, they are not losing their minds.
Knowledge is power, and I am all in when it comes to empowering patients. They can learn that menopause is a phase and does not define who they are as a person. It is possible to survive and come out on the other side still thriving, while learning how to cope during the process. There is hope!
Menopause Transitions and Pelvic Rehab is an excellent opportunity to understand the physiological consequences to the body as hormones decline, in order to assist our patients in lifestyle habits for successful aging. Lecture topics include cardiovascular changes, metabolic syndrome, bone loss and sarcopenia, neurological changes (headache, brain fog, sleeplessness), Alzheimer’s risk, urogenital changes, as well as symptoms and treatment options. These include hormone replacement, non-hormonal options, dietary choices, and exercise considerations.
Menopause Transitions and Pelvic Rehab course dates include April 9-10th and August 27-28th.