Dustienne Miller, CYT, PT, MS, WCS instructed the H&W remote course Yoga for Pelvic Pain. Dustienne passionately believes in the integration of physical therapy and yoga in a holistic model of care, helping individuals navigate through pelvic pain and incontinence to live a healthy and pain-free life. You can find Dustienne Miller on Instagram at @yourpaceyoga
Research demonstrates multiple benefits of a yoga practice that extend beyond the musculoskeletal system. These benefits include improved mood and depression, changes in pain perception, improved mindfulness and associated improved pain tolerance, and the ability to observe situations with emotional detachment.
Do the brains of yoga practitioners vs non-practitioners look different?
A study by Villemure et al looked at the role the insular cortex plays in mediating pain in the brains of yoga practitioners. They included various styles of yoga to capture the essence of yoga across multiple styles - Vinyasa, Ashtanga, Kripalu, Sivananda, and Iyengar.
Rewind back to neuroanatomy class - remember the insular cortex? The insular cortex is responsible for sensory processing, decision-making, and motor control by communicating between the cortical and subcortical aspects of the brain. The outside inputs include auditory, somatosensory, olfactory, gustatory, and visual. The internal inputs are interoceptive (Gogolla).
Villemure et al found several interesting objective differences. The practitioners had increased grey matter volume in several areas of the brain. This increase in grey matter specifically in the insula correlated with increased pain tolerance. The length of time practiced correlated with increased grey matter volume of the left insular cortex. Additionally, white matter in the left intrainsular region demonstrated more connectivity in the yoga group.
Other differences were seen in strategies utilized to manage pain. Most folks in the yoga group expected their practice would decrease reactivity to pain, which it did. The yoga group used parasympathetic nervous system accessing strategies and interoceptive awareness. These strategies were breathwork, noticing and being with the sensation, encouraging the mind and body to relax, and acceptance of the pain. The control group strategies were distraction techniques and ignoring the pain.
The authors determine that the insula-related interoceptive awareness strategies of the yoga practitioners being used during the experiment correlated with the greater intra-insular connectivity. Therefore, the authors conclude that the insular cortex can act as a pain mediator for yoga practitioners.
The more strategies our patients have for pain management, the better! Yoga is one of several non-invasive modalities our patients can add to their healing toolbox.
Yoga for Pelvic Pain was developed by Dustienne Miller to offer participants an evidence-based perspective on the value of yoga for patients with chronic pelvic pain. This course focuses on two of the eight limbs of Patanjali’s eightfold path: pranayama (breathing) and asana (postures) and how they can be applied for patients who have hip, back, and pelvic pain.
A variety of pelvic conditions are discussed including interstitial cystitis/painful bladder syndrome, vulvar pain, coccydynia, hip pain, and pudendal neuralgia. Other lectures discuss the role of yoga within the medical model, contraindicated postures, and how to incorporate yoga home programs as therapeutic exercise and neuromuscular re-education both between visits and after discharge.
References:
Gogolla N. The insular cortex. Current Biology. 2017; 27(12): R580-R586.
Villemure C, Ceko M, Cotton VA, Bushnell MC. Insular cortex mediates increased pain tolerance in yoga practitioners. Cereb Cortex. 2014 Oct;24(10):2732-40. doi: 10.1093/cercor/bht124. Epub 2013 May 21. PMID: 23696275; PMCID: PMC4153807.
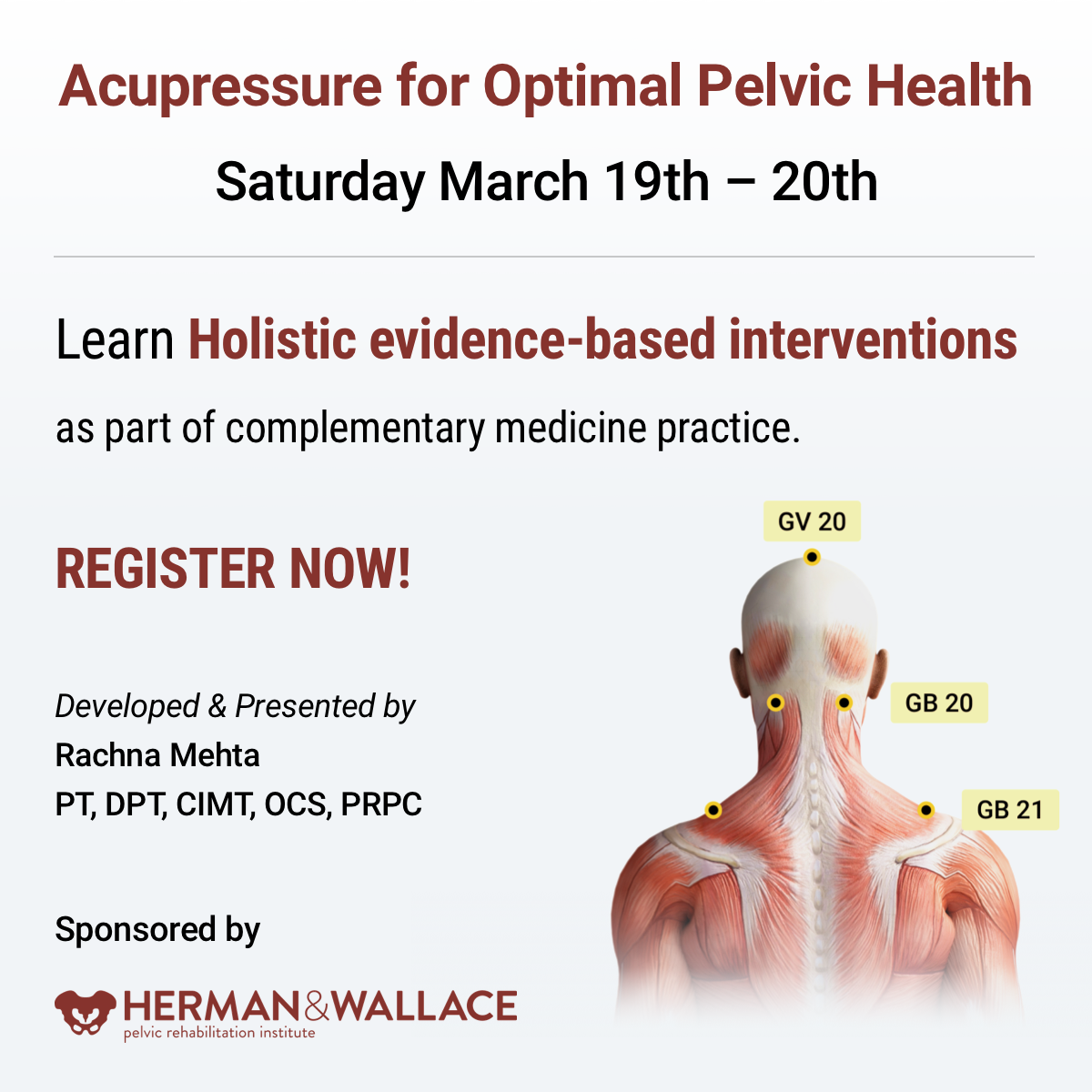
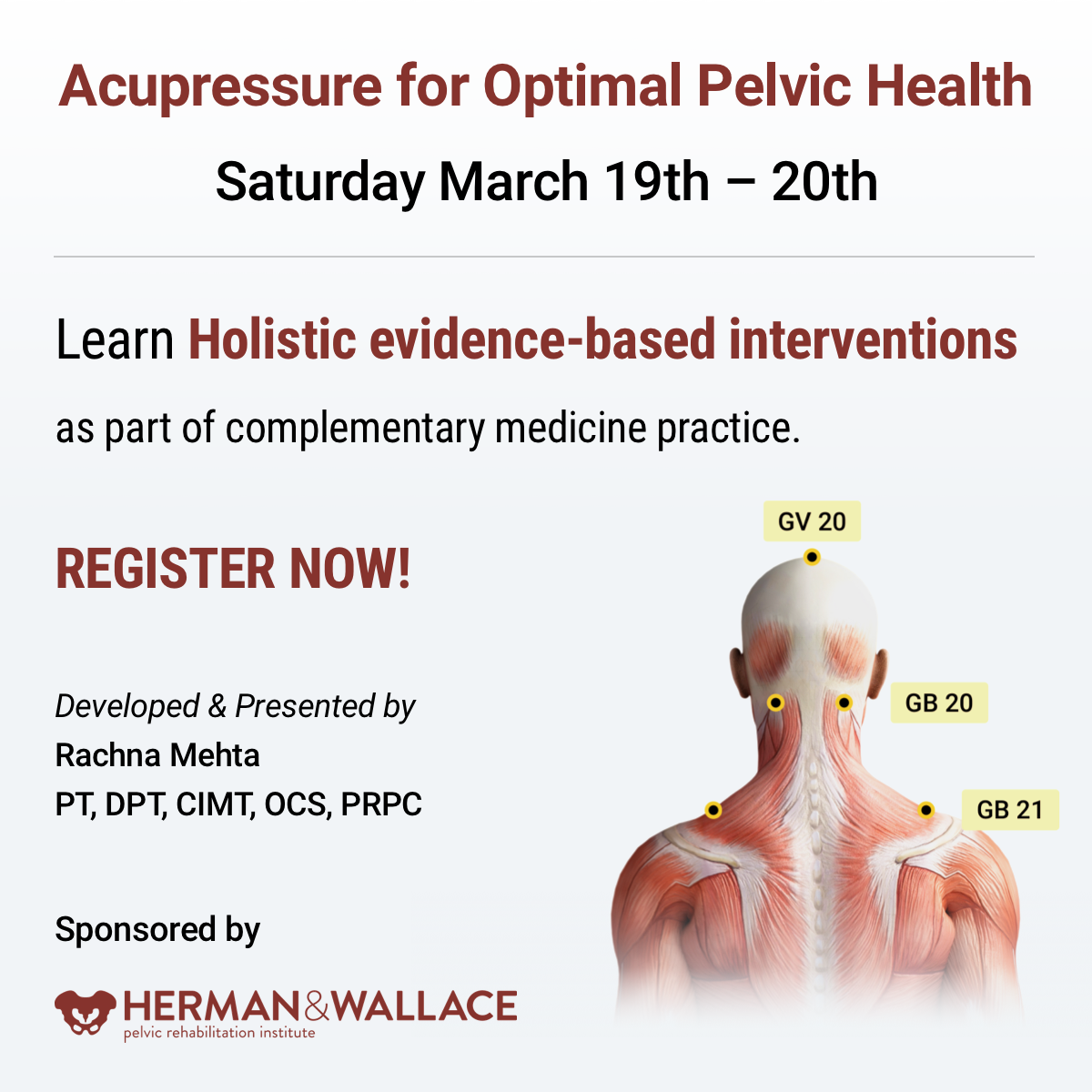
Rachna Mehta, PT, DPT, CIMT, OCS, PRPC is the author and instructor of the Acupressure for Optimal Pelvic Health course. Rachna brings a wealth of experience to her physical therapy practice and has a personal interest in various eastern holistic healing traditions. Her course Acupressure for Optimal Pelvic Health brings a unique evidence-based approach and explores complementary medicine as a powerful tool for holistic management of the individual as a whole focusing on the physical, emotional, and energy body.
What is Acupressure
According to the National Center for Complementary and Integrative Health (NCCIH), a branch of the National Institute of Health (NIH), a recent study by Feldman et al1 in the Journal of Pain showed that patients with newly diagnosed chronic musculoskeletal pain are prescribed opioids more often than physical therapy, counseling, and other nonpharmacologic approaches. A study2 by Elizabeth Monson and colleagues noted that the use of effective nonpharmacologic options is now mandated by Joint Commission Guidelines3 per updated pain management recommendations. The study also noted that there has been a growing clinical interest in Acupressure as a therapeutic modality for symptom management in Western health care.
The scientific literature presents robust evidence supporting Acupressure as an effective non-pharmacological therapy for the management of a host of conditions such as anxiety, insomnia, chronic pelvic pain, dysmenorrhea, infertility, constipation, digestive disturbances, and urinary dysfunctions to name a few.
Acupressure has roots in acupuncture and is based on more than 3000 years of Traditional Chinese Medicine (TCM). TCM supports Meridian theory and meridians are believed to be energy channels that are connected to the function of the visceral organs. Acupoints located along these meridians transmit Qi or the bio-electric energy through a vast network of interstitial connective tissue connecting the peripheral nervous system to the central viscera.
Acupressure has demonstrated the ability to improve heart rate variability, and thus decrease sympathetic nervous system activity. By decreasing sympathetic nervous system stimulation, the release of stress hormones such as epinephrine and cortisol is decreased, and the relaxation response can be augmented, which may correlate with decreasing levels of pain, stress, and anxiety2.
The Sanyinjiao (SP6) Acupoint

Sanyinjiao (SP6) acupoint is one of the most extensively researched points in the literature. It is located four finger-widths above the tip of the medial malleolus. Studies have found Sp 6 to be effective in relieving pain associated with primary dysmenorrhea, premenstrual syndrome (PMS), labor pain as well as symptoms of menopause. Ancient and modern acupuncture charts map the Spleen meridian as part of the principal 12 meridians which are connected to the physiological functions of key organs.
A recent systematic review published by Abarogu et al4 reviewed the available evidence for SP6 (Sanyinjiao) acupressure for the relief of primary dysmenorrhea symptoms, as well as patients' experiences of this intervention. The review included six studies with a total of 461 participants. The primary outcome was pain intensity. They found that:
- SP6 acupressure delivered by trained personnel significantly decreased pain intensity immediately after the intervention (effect size = -0.718; CI = -0.951 to -0.585; p = 0.000)
- Pain relief remained up to 3 h after the intervention (effect size = -0.979; CI = -1.296 to 0.662; p = 0.000)
The review concluded that SP6 acupressure appears to be effective when delivered by trained personnel for Primary Dysmenorrhea symptoms.
Acupressure has also been used with various types of mindfulness and breathing practices including Qigong and Yoga. Yin Yoga, a derivative of Hath Yoga is a wonderful complimentary practice to Acupressure. Yin Yoga is a calm meditative practice that uses seated and supine poses, held for three to five minutes with deep breathing. Yin poses supportively align the body to stress connective tissues along specific meridian lines thereby activating potent acupressure points that lie along those meridians. Mindfulness-based holistic interventions are the key to empowering our patients by giving them the tools and self-care regimens to lead healthier pain-free lives.
The course Acupressure for Optimal Pelvic Health brings a unique evidence-based perspective by integrating Acupressure and Yin Yoga into traditional rehabilitation interventions. It is curated and taught by Rachna Mehta. To learn how to integrate Acupressure into your practice, join the next scheduled remote course on March 19-20, 2022.
References
- Feldman DE, Carlesso LC, Nahin RL. Management of Patients with a Musculoskeletal Pain Condition that is Likely Chronic: Results from a National Cross-Sectional Survey. J Pain. 2020;21(7-8):869-880.
- Monson E, Arney D, Benham B, et al. Beyond Pills: Acupressure Impact on Self-Rated Pain and Anxiety Scores. J Altern Complement Med. 2019;25(5):517-521.
- Pain assessment and management standards for hospitals. Online document at: https://www.jointcommission.org/standards/r3-report/r3-report-issue-11-pain-assessment-and-management-standards-for-hospitals/
- Abaraogu UO, Igwe SE, Tabansi-Ochiogu CS. Effectiveness of SP6 (Sanyinjiao) acupressure for relief of primary dysmenorrhea symptoms: A systematic review with meta- and sensitivity analyses. Complement Ther Clin Pract. 2016;25:92-105.
- Chen MN, Chien LW, Liu CF. Acupuncture or Acupressure at the Sanyinjiao (SP6) Acupoint for the Treatment of Primary Dysmenorrhea: A Meta-Analysis. Evid Based Complement Alternat Med. 2013;2013:493038.
- Mehta P, Dhapte V, Kadam S, Dhapte V. Contemporary acupressure therapy: Adroit cure for painless recovery of therapeutic ailments. J Tradit Complement Med. 2016;7(2):251-263.

Part 1: Burnout
Let’s get real for a minute.
You are a highly educated professional. If you are reading this blog, I can assume you are invested in your career and your continued education. You are probably pretty skillful, and you help a lot of people.
BUT
How are you doing once you leave work?
Does your life outside of work give you joy and fulfillment?
Or do you leave your work setting completely drained, snippy with your loved ones, and too tired to care for yourself?
You have at least one advanced degree, probably some certifications, but did anyone ever teach you how to get your paperwork done on time?
Or how to leave work at work and not have your patients popping into your head day and night?
What about energy conservation? In fact, we may have been taught to give our ALL to work, to our patients, to strive for productivity and accomplishment. But where does that leave us?
BURNED OUT.
Part 2: Mindset
Taking continuing education classes was my pathway to becoming a better physical therapist.
But I had to go to therapy to learn how to survive as a physical therapist.
There were struggles.
Paperwork. I could NEVER finish in a timely way.
Timeliness. I was OFTEN running behind for patients.
Discharge. I had some patients for YEARS because I did not know how to discharge them even though they weren’t getting better. They depended on me, and I also depended on them.
Boundaries. I had none.
And here’s something that surprised me.
I had to change the way I THOUGHT before I could change my BEHAVIOURS.
I had to change my mindset.
I used to show up at work with the idea of Helping People. I felt responsible for their outcomes. If they weren’t doing well, I assumed I was missing something.
The shift looked like this:
I can show up at work to coach people who are responsible for their own outcomes. If they aren’t doing well, we can have honest communication about next steps (medical or otherwise), discharge, or resistance.
My patients are not my family, they are not my friends. I show up as a coach who is very interested in understanding their story and helping them reach their goals through a shared responsibility model of care.
My free time is sacred. I need to protect it for my mental, physical, spiritual, and emotional health. Because I am a priority, I will use 5 minutes of each treatment session to complete the patient’s treatment by doing paperwork.
Now, therapy is INVALUABLE. Don’t get me wrong, but paperwork, timeliness, discharge, and healthy boundaries are things MANY of us struggle with. So Nari Clemons and I designed a Continuing Education COURSE. We believe that therapists deserve to learn skills to preserve our wellbeing and strengthen our resilience against burnout.
Especially since the pandemic, more and more health care workers are reporting very high levels of burnout. Nari Clemons and I went through a period of burnout earlier in our careers. The tools and techniques we learned to heal ourselves and develop new patterns of delivering care are powerful. We know you might also be struggling and we want to help. So we developed a course to equip you. We would love to learn with you at Boundaries, Self-Care, and Meditation. A two-part, online journey toward experiencing a practice you enjoy and a life you love.
Boundaries, Self-Care, and Meditation is a two-part series intended to be completed in order. Participants should register for Part 1 and Part 2 at the same time, or complete Part 1 and wait to complete Part 2 at a later date. This course was developed by Nari Clemons, PT, PRPC, and Jennafer Vande Vegte, PT, PRPC and was "born out of our own personal and professional struggles and our journey to having a life and a practice that we love and can sustain." The intention of this class is deep, personal, and professional transformation through evidence-based information and practices. Both Part One and Part Two have a significant amount of pre-work to digest and practice before meeting via Zoom. Nari shares that "This sets the stage for you to find your path to experiencing more joy, energy, and balance."
Boundaries, Self-Care, and Meditation - Part 1 - Remote Course
In Part One, participants begin their process of study, meditation, and self-reflection in the weeks prior to the start of the class. Pre-work includes focusing on the neuroscience of pain, trauma, PTSD, and meditation. Participants will learn about the powerful influence both negative and positive experiences have on our nervous system’s structure and function. Personal meditation practice and instruction will create changes in the participant's own nervous system. Participants will also learn how to prescribe meditation for various patient personalities and needs, as well as analyze yourself through inventories on coping, self-care, empathy, burnout, values as well as track how you spend your time. Commitment to pre-work will facilitate rich discussion as we put what you have learned into practice around building a shared responsibility model of patient care, language to support difficult patients, and both visualizing and planning steps to create new, healthier patterns in your life and in your practice.
Boundaries, Self-Care, and Meditation - Part 2 - Remote Course
Part Two continues the focus on personal and professional growth for the participant, with a deeper dive into meditation and self-care practices. Yoga is introduced as a means of mindful movement and energy balance. Participants will learn to identify unhealthy relational patterns in patients and others, and skills on how to use language and boundaries to create shifts that keep the clinician grounded and prevent excessive energic and emotional disruptions. There is a lecture on using essential oils for self-care and possibly patient care. Learning new strategies to preserve energy, wellness, and passion while practicing appropriate self-care and boundaries will lead to helpful relationships with complex patients. This course also includes a discussion of energetic relationships with others as well as the concept of a "Higher Power". Course discussion will also include refining life purpose, mission, and joy potential, unique to the individual participant. The goal is that the participating clinician will walk away from this experience equipped with strategies to address both oneself and one's patients with a mind, body, and spirit approach.

Amanda Moe, DPT, PRPC specifically treats women, men, and children with disorders of the pelvis and pelvic girdle. Amanda earned her Pelvic Rehabilitation Practitioner Certification (PRPC) in 2015 to distinguish herself as a highly qualified and specialized practitioner in the field of pelvic health and worked at Texas Children's Hospital in Houston, TX. There Amanda assisted with the development and expansion of the pediatric pelvic physical therapy program treating children with a variety of diagnoses such as bowel and bladder dysfunction, constipation, encopresis, coccydynia, abdominal/groin pain, as well as other disorders related to the pelvic girdle. Amanda enjoys assistant teaching with the Herman & Wallace Pelvic Rehabilitation Institute in her free time as well as working out, practicing yoga, and spending time with her family.
Before the Book
I started off my career in Pelvic Physical Therapy treating adult women and men as do many physical therapists entering the pelvic niche. My local children’s hospital discussed a need for pelvic physical therapy in children which, with the help of Herman and Wallace’s Adult/Pediatric courses as well as mentoring from my local Gastroenterology department, I devoted the next few years of my career to.
I aided in program development and expansion of Pediatric Pelvic Physical Therapy services at Texas Children’s Hospital in Houston, Texas. After moving out of state, I then collaborated and expanded Pediatric Pelvic Physical Therapy services in Pittsburgh, Pennsylvania—working closely with both the Urology and Gastroenterology Department at UPMC’s Children’s Hospital of Pittsburgh. While treating children with pelvic dysfunctions is similar to treating those in adults, there is much to be considered when providing education to children, parents, and even referring providers about pelvic floor dysfunction and Pediatric Pelvic Physical Therapy.
The NEED for this Book
When educating children, parents, or even referring practitioners about pelvic floor dysfunction and physical therapy, I grew frustrated with the lack of “simplified” or “child-friendly” models, illustrations, or depictions available. Specifically, I saw a need for:
- the depiction of pelvic girdle muscles and organs in a “child-friendly” format for BOTH boys and girls
- pictures of what a child’s pelvic muscle “role” or “activity” is during peeing or pooping
- what common muscle dysfunctions in children “look like” in easy-to-understand pictures
Additionally, I longed for a book or resource that described common conditions and symptoms treated in Pediatric Pelvic Physical Therapy (or Occupational Therapy) as well as what the Pediatric Pelvic PT/OT evaluation and treatment may look like. In 2021, I decided to do something about this which lead to me writing my first book: Pelvic PT for ME: Storybook Explanation of Pelvic Physical Therapy for Children.
Book Features
Do you have parents, patients, referring physicians, or other medical providers wondering exactly what Pelvic Physical Therapy for children is like—look no further! In Pelvic PT for ME: Storybook Explanation of Pelvic Physical Therapy for Children, I explain the basics all in a rhyming, child-friendly format. This book introduces the collaborative nature in resolving children’s potty or pelvic troubles and describes how Pediatric Pelvic PT/OT often works closely with gastroenterologists, urologists, pediatricians, or other providers to remedy a child’s complaints. Pelvic PT for ME has many unique features pertaining to Pediatric Pelvic Physical Therapy, some of which are highlighted below:
- Common Conditions Treated
- I discuss typical conditions that are treated in Pelvic PT such as pee leaks, poo problems (constipation, poo leaks/smears), nighttime bedwetting, pelvic pain, and many others.
- Child-Friendly Anatomy Illustrations
- Age-appropriate anatomical illustrations of muscles and organs in the pelvic girdle are utilized throughout the book to aid in explaining bowel, bladder, and pelvic functioning.
- Pelvic Floor Muscles during Peeing or Pooping
- Pelvic floor muscle anatomy, functioning, and dysfunction—as they relate to potty troubles—are discussed through the use of child-friendly images to enhance not only child but also parent and referring provider understanding.
- Common Evaluation Techniques and Treatment Interventions
- The Pediatric Pelvic Physical Therapy evaluation, as well as typical treatment interventions, are discussed and illustrated to make both children and parents excited to seek treatment!
- Inclusion of Occupational Therapy
- While the field of Pediatric Pelvic Physical Therapy in of itself is new, I briefly discuss the inclusion of Occupational Therapists also providing Pediatric Pelvic Therapy services.
Where to Purchase
My primary goal behind the creation of this book was to develop an affordable resource for every Pelvic PT/OT who treats children. Secondarily, my goal was to increase knowledge and understanding of our services to parents, children, and potential referral sources or colleagues. Pelvic PT for ME encourages parents and children to refuse the notion that potty troubles “go away with age” and empowers children to be active participants in their Pelvic PT (or OT) experience. Enjoy this comprehensive yet simple storybook explanation of Pediatric Pelvic Physical Therapy, available on Amazon for $15.
Contact
Contact me or check out my website for more information: www.pelvicphysicaltherapyandmore.com
IG/Facebook: amandampelvicpt

Bre Stuhlmuller is an LA-based doctor of physical therapy (DPT) who practices at Origin, a leading provider of virtual and in-person physical therapy for women and individuals with vaginal anatomy. Dr. Stuhlmuller is especially interested in helping women through their pregnancy/postpartum journey and strives to help her patients understand the purpose behind the therapy they are receiving so they can begin to relate to their bodies differently and take an active role in their rehabilitation process.
When Covid ramped up in 2020 and Origin began to focus more fully on virtual care, many PTs were excited about this new way to reach patients. Although the prospect of working from home piqued my interest, I was still skeptical. I dabbled in virtual care at the beginning of my time at Origin, with the occasional appointment here and there. Even still, the concept of it was hard for me to fully grasp and I couldn’t say that I loved it. It felt unknown and even intimidating. I love to connect with my patients — establishing a good rapport is one of my strong suits — and I was worried that what I did in person wouldn’t translate the same way through a screen.
Looking back, I realize my attitude was very much informed by what I’d learned in training. I had a mentor during one of my rotations who emphasized the importance of human touch, how it was integral to the healing process. What would assessment and healing look like if I couldn’t use my hands?
To be fully transparent, manual therapy had also become a fallback for me while caring for my patients. If a patient was struggling to understand a concept, I could use my hands to show them. If I found myself at a loss of what to do next, I could provide manual therapy — it was always welcomed, felt productive, and gave me time to plan. With virtual, I knew I would have to rethink how I approached my assessment and treatment strategy, and I had no idea what that might be.
New Fuel for Creativity & Connection
When it was clear I didn’t really have a choice, I gave virtual PT a try for more than just those occasional appointments. At first, as I was building up my caseload, it lived up to my not-so-positive expectations. It just wasn’t the same and I felt completely out of my element. It wasn’t until I began filling my caseload entirely with virtual visits that it began to surprise me.
As I engaged more consistently with patients on Zoom, my creativity kicked in. Without my hands to fill in the gaps, I really had to think about the cues that I was giving and how I was explaining things. Suddenly, my mind was lighting up with new ideas and ways of getting my point across. Where should the patient be focusing their attention? What should they be noticing or feeling?
I began helping patients tune into their bodies, instead of solely looking to me to give them information. Often, when I first ask “What do you feel when you do X?” a patient’s first response is vague and unsure. Then I’ll try again, talking through the concepts and movement in more detail. I’ll describe the outcome I am after and provide analogies and examples. If that doesn’t work, I’ll have them try a different position, or experiment with a new analogy that relates to their life and specific situation.
What happens next has been so encouraging — I see them have a pretty powerful ah-ha moment. (And because they’re not wearing a mask, it’s great to be able to see the understanding on their face!) They’re connecting with and learning from their body directly, which gives them so much empowerment. They tap into their own abilities instead of only relying on mine, which is exactly what we hope to give to our patients. On my side, I continue to gain clarity and hone my communication skills. I’m excited to share that despite doing all of this through a screen, my connection with patients feels as strong as ever.
That’s not to say that patients aren’t missing manual therapy! If you’re a PT who sees patients in person, you know how much they like (and often expect) it. I think they can tend to rely on it too much — and a decent number of people really want to come in and just get something like a massage. That can be a struggle. We are not massage therapists. And unfortunately, some patients think they need it in order to get better. I think that will be an ongoing struggle when it comes to getting patients to try virtual physical therapy. But, in my experience, once they do try virtual, they are quickly won over.
The Habit Building Power of Home
Another unexpected benefit of virtual physical therapy is the level of follow-through. For starters, patients cancel much less, which makes sense — it’s a lot easier to hop on a Zoom call at the last minute than it is to get in the car (and find parking). And if childcare isn’t available, they can keep an eye on their kids while we do our visit. We may not always get quite as much done, but at least we are able to do something, which I’m constantly reminding my patients is always better than nothing.
Along the same lines, in the few months since I’ve switched to solely treating virtually, I’ve been surprised to discover that patients seem more consistent with their exercises, not less. We’ll be collecting more data on this at Origin, but my guess is that being introduced to an exercise in the same environment where they’ll be doing it on their own makes a difference. When they do their exercises with me during a virtual visit, they’re creating a foundation of a habit. Later on, when it’s time to continue on their own, they can pick up right where they left off.
As much as I absolutely love our clinics at Origin — having all the equipment on hand, the music playing, and the other patients and PTs around — it is a very different experience for patients compared to being at home. At home, patients have to self-motivate and are limited to the equipment they happen to have or are willing to buy. Starting from scratch in their own space can often be a major barrier.
When we’re in a virtual visit, I can help a patient set up the space where they’ll do their exercises, and we can improvise. They may need to use a thick pillow instead of a pilates ball, or a rolled-up towel instead of a yoga block. This eliminates all those excuses along the lines of, 'I couldn't do my exercises because I didn’t have X.’ It not only helps me stretch and refine my skills as a PT, it helps patients gain more agency— it encourages patients to get into the mindset of “let’s see how I can make this work with the resources I have.”
Just as invaluable is being able to coach a patient through functional movements. I can watch a new mom lift their baby out of their crib or get up from their couch, then give tips and recommendations that are specific to their setup. Then I watch them immediately apply those tips and feel the difference. And boom, I know they’ve got it.
Tips for PTs Interested in Going Virtual
As a PT, having a separate, designated space to work is critical. At first, I was doing it in the corner of my bedroom, next to my bed, with limited lighting. Although I made it work, it was awkward to not have room to move and didn’t serve my patients the way I wanted. I have now made a space in our garage with bright lighting and a white backdrop behind me. You don’t necessarily need a whole setup, but you want to ensure that your patient can see your entire body when demonstrating movements or exercises. And of course, you need strong, reliable wifi!
One challenge that comes up is that virtual patients can be distracted at the start of or even throughout a visit. Because they’re at home and may have just stepped away from kids or work, they may need time to refocus. This is very different from being at the clinic, where the few minutes it takes to check-in and get settled helps them be more present. So I’ve learned to expect this, give them some grace, and will spend a few minutes bringing their attention back to their goals.
I also want to say that I do miss being in the same space with other Origin PTs. I miss the time in between patients when you can have those quick, but incredibly helpful conversations like “oh have you had a patient who presents like this,” or “let’s go into a room and I’ll show you how I do this.” It’s hard to recreate that kind of spontaneous interaction online. We have a shared Slack channel where PTs can chat throughout the day about our cases and although it helps to fill in that missing gap, it can also be nothing but crickets and still lacks that same feeling you get physically being in the office with your colleagues.
One major perk, however, is being able to spend more time between patients with my 2-year-old daughter. It makes being a working mama feel a little less of a sacrifice. But don’t get me wrong, it also comes with its challenges. I don’t have that same downtime driving to/from work to decompress and switch between mom mode and work mode. And it can be easy to get distracted between appointments and do chores or play with my daughter instead of cranking out my notes. At some point, I imagine I will want to split my time between the clinic and working from home. But for now, I am honestly more than content working virtually.
Origin is already working on new ways to integrate virtual and in-person therapy — thinking beyond either/or, toward a model where we can choose what works best from patient to patient and visit to visit. In the meantime, I’m excited to continue with virtual care and our patients are loving this option. My schedule has been more full in the past 4 months than it was before I went virtual, and I’m seeing more people get better under my care. It’s truly amazing to see them making so much progress, right at home.

As 2022 has gotten underway, it has already brought many of us to a place where we simply need to hear something lighthearted. The start of a new year also gives us a chance to examine priorities and make room for what matters most. “What matters most” can look different for each of us; for me, it’s my family – including two dogs – Stella and Sadie. Of course, the dogs fall in line behind my human nuclear and extended families, however, they are such a part of my daily life and contribute to my quality of life, it seems only natural to share this story with a wider audience -especially because this story revolves around one of my favorite topics – intentional nourishment!
Let me begin by telling you about our 5-year-old Golden Retriever named Stella. She came to us as one of only three puppies in a litter; a pleasantly plump pup, she was well developed, well-fed, and well-loved. According to everyone who has had the opportunity to meet her, she is the happiest dog they’ve ever met. When we brought her home at eight weeks, she topped the scale at 21 lbs.
Stella's fur was shiny, her disposition sunny; she emanated maturity and wisdom. She slept through the night with such efficiency, we hardly remember having to let her out at night as a puppy. She was content; the perfect combination of calm and energetic. She was a breeze to housetrain, has an impeccable record of only two accidents in the house, and nary an indoor fecal incontinence episode. Stella brought us so much joy that we decided on a whim to add a second puppy to the milieu.
The second puppy is our ~16-week-old Golden Retriever puppy named Sadie. This past October – by coincidence – my family learned about some surprise Goldens needing homes – 17 to be exact – and we wondered if we might be interested in one. Two weeks later, sweet Sadie came home with us.
Weighing in at only 13 lbs 6 oz at eight weeks, she was miniature compared to Stella at the same age. It didn’t take us long to figure out that not only was she smaller, but her digestive tract and elimination systems were not like Stella’s either. Sadie pooped often - what seemed like every hour – including sometimes in the house. Her bottom was sore and irritated, and she seemed frustrated and uncomfortable. My husband and I looked at each other more than once thinking the same thought: WHAT did we get ourselves into?!?
Sadie tested negative for parasites, and the vet said she was just working on adjusting to her new home and to give it time. He also suggested we might be feeding her too much. So, we fed her less - but that didn’t help. We tried adding pumpkin, that didn’t help either. Then we upped her food amount again, tried timing her foods differently, tried feeding her more often, then less often. None of these approaches helped. The messes continued.
We began to feel exasperated. I was reluctant to try adding new foods for fear of upsetting her GI tract further.
This puppy was pooping nonstop – much of it type 6 & 7 applying the Bristol Scale to dogs (1). She barely came in at 16 lbs. week 10 and alarmingly, she still weighed 16 lbs. at week 12. The vet confirmed our concerns – she was too thin and needed to put on weight.
Now I started to worry. With all the bowel troubles she had, how could she thrive? We weren’t getting any continuous hours of sleep at night which meant she wasn’t either. It was an exhausting few weeks.
Given what we had tried – with no success – we had no choice but to begin what we called “Operation Nourishment” for this little puppy. We put worries aside about adding new foods and applied what we understand about functional nutrition to help our sweet Sadie.
“Operation Nourishment” consisted of following several basic digestive principles:
- Make her food more digestible
- Feed her nutrient-dense options (dog appropriate, of course)
- Practice puppy-version mindfulness at mealtime
- Help support her puppy microbiome
#1: Make her food more digestible: Without changing the kibble she was eating, we soaked it with a bit of water before ingestion to soften it. This helped make her food easier to break down in her digestive tract and also helped S L O W D O W N her tendency to inhale food. Prior, she was definitely not chewing her food thoroughly which can result in undigested food reaching the colon and causing irritation. The softened food facilitated just the slightest bit of chewing and tripled the time it took her to finish a meal, giving her GI tract less of a shock.
#2: Feed her nutrient-dense options: We began adding an organic egg (3,4) softly cooked in a tiny bit of coconut oil (2) to her breakfast. The egg adds a whole food-based protein-containing cholesterol, vitamins, and minerals -all important for building her gut lining and nervous system. Coming from such a large litter in a somewhat stressful/chaotic environment, her gut and nervous system may not have been at their healthiest and needed extra support (4).
#3: Practice mindfulness at mealtime: The egg at breakfast has quickly become the highlight of her day.
The anticipation while watching us cook it calms her. She intently follows as the pan comes out of the cupboard and onto the stove. She watches more intently as we slowly cook the egg. Then she must wait even longer while it sits in her bowl to cool up on the countertop.
I presume this has taught her mindfulness and presence before eating – essential for thorough digestion!
#4: Help support her puppy microbiome: We gradually began to add a dollop of kefir (5) to her breakfast and dinner – knowing that even dogs have a microbiome and that cultured foods can help normalize gut flora which can help normalize stool consistency. A healthy gut helps us extract nutrients from the food we eat. It can also, fascinatingly, modulate our stress responses.
“Operation Nourishment” began to take effect almost immediately. She jumped from 16 to 24 lbs. in 3 weeks! We were so proud! She finally began to have a soft, healthy belly - and the vet was thrilled, “whatever you’re doing, keep it up!”. She began to sleep through the night – and WE were thrilled. She also began to sprout her golden retriever fur patterns and take on more shine. Brilliantly, her stools became formed – a perfect 4 on the Bristol Stool Scale (1) and had significantly less urgency which led to the elimination of accidents. We were shocked at how quickly her body adapted to a diet higher in nutrient density and digestibility– one that was safe and appropriate for puppies.
Upping her nutrient density and digestibility helped unlock her potential so she could become the best sweet version of herself. Once more deeply nourished, she happily settled into her calm, gentle nature. She and Stella have become quite the pair. And we – her humans - are finally, gratefully sleeping again (most nights), which makes us adore her even more.
How might A Tale of Two Goldens provide us with insight relevant to pelvic rehabilitation?
We acknowledge that no two people come into this world in exactly the same circumstance and that we each arrive with a certain level of built-in resiliency. Some of us come into this world with our tails wagging, ready to greet everything that comes our way. Many of us and those we serve– let’s face it –are figuratively more like Sadie. We have the potential waiting inside of us to become the best version of ourselves.
Sometimes reaching that potential takes just a little tweaking, a little coaxing, a little know-how. Maybe that tweaking, coaxing, and know-how could include principles of “Operation Nourishment” for ourselves and those we serve in the form of nourishment-focused guidance. With a little patience, time, and intentional action, we may be surprised to see how a few small changes have an enormous impact on what matters most to each of us and those we serve.
Nourishment knowledge – now more than ever – is vital.
Join us in 2022 for Nutrition Perspectives for the Pelvic Rehab Therapist to learn more about these principles and beyond. Upcoming 2022 remote offerings include Feb 26-27, April 29-30, July 23-24, August 27-28, Sept 23-24, Oct 22-23, and Nov 11-12. We welcome you to join us.
References:
- https://www.bladderandbowel.org/wp-content/uploads/2017/05/BBC002_Bristol-Stool-Chart-Jan-2016.pdf Accessed January 11, 2022.
- Alves DVS, Sousa MSB, Tavares MGB, Batista-de-Oliveira Hornsby M, Amancio-Dos-Santos A . Coconut oil supplementation during development reduces brain excitability in adult rats nourished and overnourished in lactation. Food Funct. 2021 Apr 7;12(7):3096-3103. doi: 10.1039/d1fo00086a. Epub 2021 Mar 15. PMID: 33720258.
- Avirineni BS, Singh A, Zapata RC, Phillips CD, Chelikani PK. Dietary whey and egg proteins interact with inulin fiber to modulate energy balance and gut microbiota in obese rats. J Nutr Biochem. 2022 Jan;99:108860. doi: 10.1016/j.jnutbio.2021.108860. Epub 2021 Sep 11. PMID: 34520853.
- Choi, M., Lee, J. H., Lee, Y. J., Paik, H. D., & Park, E. (2022). Egg Yolk Protein Water Extracts Modulate the Immune Response in BALB/c Mice with Immune Dysfunction Caused by Forced Swimming. Foods, 11(1). doi:10.3390/foods11010121
- Vieira CP, Rosario AILS, Lelis CA, Rekowsky BSS, Carvalho APA, Rosário DKA, Elias TA, Costa MP, Foguel D, Conte-Junior CA. Bioactive Compounds from Kefir and Their Potential Benefits on Health: A Systematic Review and Meta-Analysis. Oxid Med Cell Longev. 2021 Oct 27;2021:9081738. doi: 10.1155/2021/9081738. PMID: 34745425; PMCID: PMC8566050.

Elijah Sharrieff is the content writer for My Community Health Network. MYCHN is a full-service healthcare provider in Houston Texas, that provides accessible health care in multiple Houston Communities. Elijah specializes in blogs that educate patients on relevant topics such as: prenatal care, mental health, the importance of diet and exercise, and dental care. Elijah’s holistic approach to health care blogging stems from his background in education. Elijah taught preschool, middle school, and tutored college and high school students. Teaching allowed Elijah to realize the interconnected nature of health as it relates to the mind and body.
Cervical Health Awareness
Cancer is among the leading causes of death in America. Despite this, cancer is one of those things that you don't think will happen to you. We like to think we are healthy individuals, but cancer is unpredictable and complicated.
Around 300,000 women are diagnosed with cervical precancers in America. MYCHN has created a list of prevention tips to ensure a healthy cervix!
What Causes Cervical Cancer?
Cervical Cancer typically develops when healthy cervix cells grow and multiply continuously. In other words, they don't die like normal cells. Instead, these continually replicating cells form a mass, also known as tumors.
In many cases, HPV can lead to cervical cancer. However, an HPV diagnosis doesn't mean you will be diagnosed with cervical cancer.
What are Cervical Cancer Risk Factors?
Risk factors can increase your cancer risk. There are multiple risk factors for cervical cancer; some of them may surprise you.
- Sexual history: Your sexual history can put you more at risk for cervical cancer.
If you are sexually active at a young age (18 years old and under)
- Diet: If you do not consume a balanced diet, you could be at higher risk for cervical cancer
- Cervical Cancer in the family: If you have family members who have cervical cancer, your chances of developing cervical cancer are higher than if no one in your family has it. In some cases, this is because of rare inherited conditions that make it harder for some women to fight HPV.
- Smoking: It's a difficult habit to quit. However, smoking has been shown to harm the body. Women who smoke are twice as likely to develop cervical cancer.
Tobacco by-products have been found in the cervical mucus of women who smoke. Some studies have shown that the chemicals in cigarettes can damage the DNA of cervix cells. This occurrence can lead to the development of cervical cancer.
How can you Have a Healthy Cervix?
Prevention is going to be vital to lowering your risk of cervical cancer. What are some cervical cancer prevention methods?
- Pap Smear:
A pap smear is a screening that looks for abnormal changes that could lead to cancer. Luckily, cervical cancer doesn't develop overnight, so regular pap smears are useful in cervical cancer prevention.
- Following up with your health care provider:
Following up with your health care provider is crucial to cervical health. Health care providers provide access to pap smears and other preventative measures.
- Get the HPV Vaccine:
The HPV vaccine protects against sub strains of HPV that lead to cervical cancer.
- Limit your sexual partners:
Unfortunately, HPV is easily spread. It is relatively easy to become exposed to HPV. The virus spreads through skin-to-skin contact, so it can be spread without having sex. The American cancer society has stated that HPV can be spread through hand to genital contact.
With the aforementioned in mind, limiting the number of sexual partners could put you at a lower risk of HPV.
- Stop smoking:
Smoking is a tough habit to shake. However, the consequences of smoking are severe for the body's health in the long term. Many cigarettes and tobacco products have harmful cancer-causing chemicals. In addition, smoking weakens your immune system.
A weakened immune system makes it harder for your body to fight viruses like HPV. Just a gentle reminder, HPV can lead to cervical cancer.
Pap Smear Near Me
According to The World Health Organization, cervical cancer is the fourth most common cause of cancer in women. Pap Smears are an excellent cervical cancer prevention method. MYCHN offers pap smears and other women's health services. We have 11 locations in the metropolitan Houston area.
CHN Cares for patients with private insurance, Medicaid, Medicare, and uninsured! Visit https://mychn.org/services/womens-health/ for more.
Bottom Line
Cervical cancer is common cancer for women and, in many cases, can be deadly. Thankfully, there are prevention methods to prevent the disease. For example, regular Pap smears can be used to prevent Cervical cancer.
Eating a balanced diet and not smoking can also be excellent prevention methods.
My Community Health Network. MYCHN is a full-service healthcare provider in Houston Texas, that provides accessible health care in multiple Houston Communities.
References:

Sarah Haran PT, DPT, OCS, CF - L2 earned a BS in exercise science from Gonzaga University and a DPT from the University of Washington. She has been practicing in Seattle for almost 15 years and opened her private practice, Arrow Physical Therapy in 2016. Her specialties include dance medicine, the CrossFit and weightlifting athlete, and conditions of the hip and pelvis such as femoroacetabular impingement and labral tears. In 2017, she began coaching other PTs who wanted to start their own practices and from there, she co-founded Full Draw Consulting with her partner Dr. Kate Blankshain. Together, they offer coaching, consulting, and several 8-week online business courses for Physical Therapy entrepreneurs. Sarah Haran instructs Weightlifting and Functional Fitness Athletes, next scheduled for February 26th, 2022.
As a physical therapist who works with CrossFit® athletes, I want to address a persistent problem we have in our professional community. Many PTs don’t know what to do with CrossFit® athletes.
When CrossFit® first came on the scene, a lot of PTs would encounter athletes who had injuries or dysfunctions related to their sport. Perhaps shoulder pain from kipping pull-ups or low back pain from deadlifts or kettlebell swings, maybe stress incontinence from box jumps.
Whatever it was, it seemed like we were seeing Crossfitter after Crossfitter in our practices. Was it that they were injuring themselves more than other athletes? Was it that their sport was bad and full of terrible ideas and awful coaching? I think what we were seeing was the quick growth of a popular sport (lots of people participating) and a community of people who not only were pushing themselves in the gym but who were interested in getting better and back into the gym quickly (ie. seeking rehab quickly). And then we were seeing rehab professionals who didn’t know how to help and were overwhelmed by the complexity of the sport.
And while there are some folks in healthcare who would like to see CrossFit® lose popularity, the reality is that it is here to stay and you will likely be faced with treating these athletes in some capacity. But what do we do with them? How do we keep our patients healthy when they want to continue to participate in CrossFit®??
The 3 primary duties of the physical therapist:
- Work to understand the sport
- Educate ourselves about where in the body these injuries commonly occur and how they happen
- Design rehab programs:
- ○ which address training volume just as we would in any other sport
- ○ that are functional to these athletes
- ○ that supplement CrossFit® workouts with accessory work to:
-
- ■ drill positions
- ■ strengthen weaknesses
- ■ mobilize tightness
- ■ improve endurance for these positions/movements

The messaging we need to communicate to our CrossFit® patients:
- Form and technique need to come first… then volume, weight, difficulty, and intensity.
- Mobility is not just flexibility; we also need to emphasize stability through a range of motion.
- Scaling and modifying is critical to all athletes at some point in their career. Work with your PT and coach to make appropriate decisions.
- CrossFit® is here to stay. Let’s keep our athletes in this sport for the long haul.
Treating CrossFit® athletes has been a primary passion of mine for many years and it is very exciting to be able to offer a course with Herman & Wallace that introduces the sport to other PTs. You do not have to be a CrossFit® athlete or specialist to want to help these patients and we want all the fabulous PTs out there to be able to impact the CrossFit® community effectively.
Weightlifting and Functional Fitness Athletes will review the history and style of Crossfit exercise and Weightlifting, as well as examine the role that therapists must play for these athletes. Common orthopedic issues presented to the clinic will be examined.
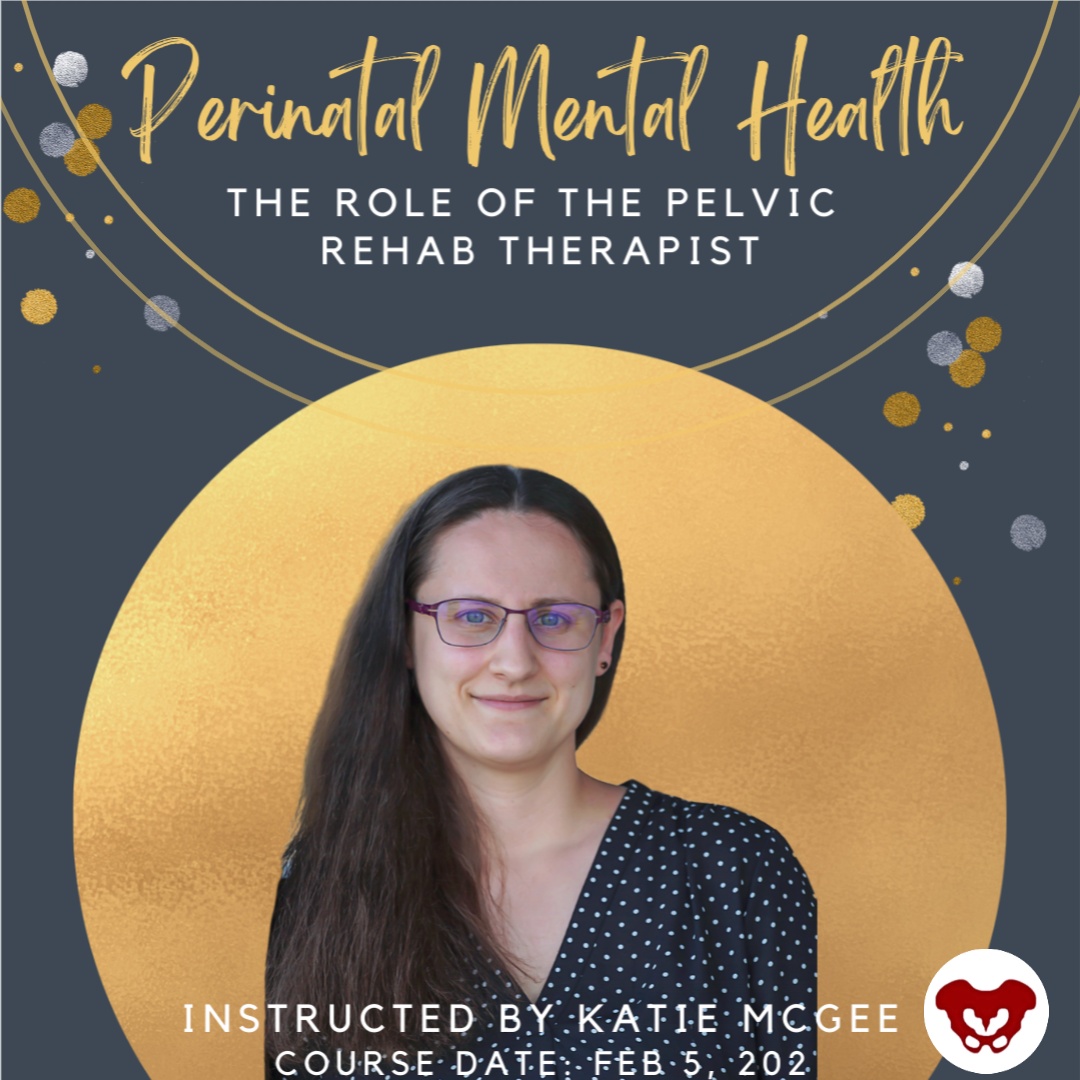
Katie McGee, PT, DPT, (they/them) is a pelvic health physical therapist based in Seattle. Katie received their Doctor of Physical Therapy from the University of Washington in 2014 and their board certification as a Women’s Health Clinic Specialist (WCS) in 2018. Their practice, B3 Physical Therapy, centers on transgender care and perinatal rehabilitation. Join H&W and Katie to learn about perinatal mental health in Perinatal Mental Health: The Role of Pelvic Rehab Therapist - Remote Course scheduled for February 5, 2022.
Due to the COVID-19 pandemic, rates of perinatal mental health conditions—such as anxiety and posttraumatic stress disorder—have risen sharply1. Around 70% of pregnant people are now reporting psychological distress1. With many families under increased stress and financial worry, the odds of developing postpartum depression have jumped from one in seven to one in five(1)!
Fortunately, pelvic rehabilitation therapists can make a difference in the mental health of their perinatal clients. In fact, many pelvic rehab therapists are reducing the risk of perinatal mental health issues without even knowing it! Simply supporting clients in keeping up with physical activity and reducing bodily pain are proven strategies for lowering the risk of perinatal mental health issues (2,3). Pelvic rehab providers can go even further in supporting their perinatal clients’ mental health with some simple actions:
1. Ask – Many birthing people feel shame around negative feelings and thoughts related to pregnancy and postpartum. Asking perinatal clients about their emotional challenges can help break through that shame. A good ice breaker for talking about perinatal mental health is letting your clients know that a mood disorder is the number one complication of pregnancy. Be sure to listen attentively and avoid interruption whenever someone discloses their mental health challenges.
2.Screen – Screening for mental health conditions can guide pelvic rehab therapists to know when it’s time to refer clients to specialized care, such as medication and/or therapy. Pelvic rehab therapists are qualified to use several screening tools in the perinatal period, including the Edinburgh Postnatal Depression Scale, the Patient Health Questionnaire-9, and the Generalized Anxiety Disorder-7. Best of all, these tests are free to use and easy to administer.
3. Gather resources – When a client discloses that they have thoughts of self-harm or are experiencing violence in their home, you want to be prepared with the next steps to help. Collecting resources ahead of time can go a long way in turning what would have been a fumbling offer to help into a confident action plan. Looking to grow your resource list? Check out these three links:
- Perinatal Mental Health Resources: https://www.postpartum.net/
- Intimate Partner Violence Resources: https://www.rainn.org/
- Substance Use Resources: https://www.samhsa.gov/
4. Connect – Racism leads to People of the Global Majority birthing in the United States to experience increased rates of preterm birth and low infant birth weights (4). Both these outcomes have been tied to worse postpartum mental health (5). Research shows that when People of the Global Majority are connected to culturally congruent birth doulas, rates of preterm birth and low infant birth weights fall (6). Other research similarly supports the concept that when people are paired with culturally congruent providers, health outcomes improve (7). Whenever possible, think about how you can offer your clients resources/referrals that match their identity and background to support their mental wellbeing.
5. Learn – Join Katie McGee, PT, DPT (they/them) for the Herman & Wallace course, Perinatal Mental Health: The Role of Pelvic Rehab Therapist - Remote Course scheduled for February 5, 2022. By participating in this remote learning class, you will:
- Develop a basic understanding of perinatal mood and anxiety disorders
- Bolster your listening skills for working with perinatal clients
- Gain additional tips for screening for perinatal mental health issues
- Learn how to help clients create perinatal wellness plans
- Expand your toolbox of coping skills to teach clients
Don’t miss this opportunity to truly change the lives of your perinatal clients!
References
- Yan H, Ding Y, Guo W. Mental Health of Pregnant and Postpartum Women During the Coronavirus Disease 2019 Pandemic: A Systematic Review and Meta-Analysis. Front Psychol. 2020;11:617001.
- Mathur VA, Nyman T, Nanavaty N, George N, Brooker RJ. Trajectories of pain during pregnancy predict symptoms of postpartum depression. Pain Rep. 2021;6(2):e933.
- Marconcin P, Peralta M, Gouveia ÉR, et al. Effects of Exercise during Pregnancy on Postpartum Depression: A Systematic Review of Meta-Analyses. Biology (Basel). 2021;10(12):1331.
- Andrasfay T, Goldman N. Intergenerational Change in Birthweight: Effects of Foreign-born Status and Race/Ethnicity. Epidemiology. 2020;31(5):649-58.
- Anderson C, Cacola P. Implications of Preterm Birth for Maternal Mental Health and Infant Development. MCN Am J Matern Child Nurs. 2017;42(2):108-14.
- Thomas MP, Ammann G, Brazier E, Noyes P, Maybank A. Doula Services Within a Healthy Start Program: Increasing Access for an Underserved Population. Matern Child Health J. 2017;21(Suppl 1):59-64.
- Towning EJ, Purohit A. Black babies cared for by black doctors less likely to die in the US: revolutionize medical education to tackle the problem in the UK. BMJ. 2020;370:m3783.

I will never forget when my sister, my bestie, told me she wanted to end her life. We were on the phone late one night, tears flowing. Depression was always a companion, but I had never heard her in such a state of despair. We made a plan that she would call the suicide hotline, then call her therapist and her doctor in the morning for urgent care. She made it through the night. Later, I went to her therapist with her so I could better understand and support my sister. She did her due diligence, adjusting medication and staying open and honest in therapy. Suicidal ideations would sometimes flare when there were triggers, but she was able to work through them, and now they are in the past.
Contrast that story with another. Ryan was a sweet woman who developed pudendal neuralgia after a routine hysterectomy. Right away, she told me she had a counselor who she loved who helped her navigate life with DID (Dissociative Identity Disorder) and that I’d probably be interacting with various personalities during our sessions. She helped me understand how to best support her during her care. We worked well together, and although she struggled with both the pain and the unfairness of what happened to her, she was well supported. Then her sweet dog passed away. It was so hard for her. She kept going through pain and heartache and found another pooch to adopt. And then the next visit, she didn’t show. And the next, and the next. And then I found out she was gone. Suicide. This hit me hard. Were there signs that I missed? Was there anything I could have done?
As pelvic rehab providers, we sometimes see people who have intense physical pain often combined with significant emotional wounds. In a study of 713 women seeking support for pelvic pain, 46.8 reported having sexual or physical abuse history, and 31.3 were positive for PTSD (1).
Chronic pelvic pain impacts all aspects of people’s lives: physical, financial, relational, emotional, and mental. People can also become dependent on narcotics or recreational drugs which may lead to intentional or accidental overdose, per Philip Hall, a gynecologist in Australia (2).
In a study of 13,500 women with endometriosis, half reported experiencing suicidal thoughts (3).
So what’s our role as health care providers?
It’s important to note that not everyone who is considering suicide will admit it, and not everyone who thinks about suicide will follow through with it. However, all threats of suicide should be taken seriously. Let people know you care, they are not alone, and help is available.
Ask questions: It may feel scary, but it won’t push someone into harmful action. The Columbus Protocol, listed below, uses three questions to identify suicide risk. If someone answers yes to any question, they have a significantly higher risk of suicide and need support(4).
- Have you wished you were dead or wished you could go to sleep and not wake up?
- Have you had any thoughts about killing yourself?
- Have you thought about how you might do this?
Be observant of warning signs:
- people may talk about taking their own life, wishing they could end things, wishing they were never born
- you may observe extreme mood swings
- the person may start putting their affairs in order
- there may have been a recent trauma or crisis
- you may notice withdrawal or sudden calmness
- the person may participate in risky or reckless behavior
If someone admits to planning for suicide, as health care providers, we MUST take supportive action. If your facility does not have a protocol, consider these steps:
- Call 911 and perhaps a friend or family member to meet the person at the hospital
- Stay with the person until help arrives
- Remove any objects that may be used for harm
- Listen with kindness and understanding
- Stay Connected: studies show that follow up after an event decreases the risk of suicide death(5)
It’s helpful also to note the following protective behaviors, as reported by psychiatry.org(6):
- Connection with health care providers
- Strong connections between family, friends, community
- Skillfulness around problem-solving and conflict resolution

Knowing what to look for, what questions to ask, and how to get someone the help they need empowers health care providers to provide the best support for patients struggling with suicidal ideation and contemplation.
There are local and national resources for us as well.
The National Suicide Prevention Lifeline: 1-800-273-(TALK) (1-800-273-8255). The Lifeline provides 24/7, free and confidential support for people in distress, prevention and crisis resources for you or your loved ones, and best practices for professionals in the United States(7).
References:
- Meltzer-Brody, S., Leserman, J., Zolnoun, D., Steege, J., Green, E., & Teich, A. (2007). Trauma and posttraumatic stress disorder in women with chronic pelvic pain. Obstetrics & Gynecology, 109 (4), 902-908.
- https://standrewshospital.com.au/about-us/news/news-listing/2016/09/05/chronic-pelvic-pain-linked-to-suicides-in-young-women
- https://www.bbc.com/news/health-49897873
- https://cssrs.columbia.edu/the-columbia-scale-c-ssrs/about-the-scale/
- Motto, J. A., & Bostrom, A. G. (2001). A randomized controlled trial of postcrisis suicide prevention. Psychiatric Services52(6), 828-833.
- https://www.psychiatry.org/patients-families/suicide-prevention
- https://suicidepreventionlifeline.org/