


This specialty of pelvic health has given each of us so many things: purpose, community, and a means to empower and equip so many people to better understand and care for their pelvic health challenges and reach their goals.
But for the rest of the developing world, it’s not like that. Imagine a place where the field of pelvic health simply doesn’t exist. Where women have no choice but to live the rest of their lives with leaking, and community condemnation from birth-induced fistula. Where men suffer in silence with impotence and pelvic pain. Where people with all types of pelvic health conditions must go about their lives hiding and suffering in their private shame.
And then imagine that YOU had the power and influence to change this! To extend your influence, expertise and support all the way across the world to East Africa - to the Amref International University in Nairobi Kenya (AMIU), where even now two cohorts of the FIRST Masters Level Pelvic Health Therapists are busy preparing to revolutionize the understanding and delivery of pelvic rehab in East Africa: Kenya, Uganda, and Ethiopia!
“Is anyone else feeling super burnt out from complex patients right now? I’ve been in pelvic health for 20 years and used to see a lot of easy urinary incontinence patients who all got better fairly quickly. Now all I have is pudendal neuralgia, pelvic pain, and bowel dysfunction. I can’t remember the last SUI patient I had!!”
This week I was tagged in a social media post, that started with the above inquiry…and quickly filled up with thirty-six replies from therapists all over the US, with comments like:
- “The burnout is real.”
- “Mental health issues of today are complicating our patients’ presentations.”
- “Some days I wish for a straightforward TKA.”
- “It’s mentally exhausting.”
- “The simple solutions are rare.”
- “There is so much going on in our world, toxin exposure, stress, work expectations, loneliness, less access to nature and healthy food, less access to being outside…our health is suffering.”
- “The better our skills, the more complex our patients become.”
The last is a favorite. You, dear therapist, INVEST and WORK HARD to EQUIP yourself to serve a population of patients that is ever-increasing in complexity.
Special thanks to faculty member Jennafer Vande Vegte, MSPT, BCB-PMD, PRPC for writing this article. Jen began her career as a physical therapist at Spectrum Health in Grand Rapids, MI she has focused her professional attention on treating women, men, and children with pelvic health disorders since 2002. She has been faculty for Herman & Wallace since 2009 and loves to inspire other rehab professionals treating pelvic floor dysfunction. She is an author of the chapter, “Manual Therapy for the Pelvic Floor” which was published in the book, “Healing in Urology.”
To the physical therapists,


Jennafer Vande Vegte, MSPT, BCB-PMD, PRPC began her career as a physical therapist at Spectrum Health in Grand Rapids, MI. Since 2002 Jen has focused her professional attention on treating women, men, and children with pelvic health disorders. She has been faculty for Herman and Wallace Pelvic Rehabilitation Institute since 2009 and loves to inspire other rehab professionals treating pelvic floor dysfunction. She is an author of the chapter, “Manual Therapy for the Pelvic Floor” which was published in the book, “Healing in Urology.” Jen was a contributing writer for the Pelvic Floor Capstone curriculum and also co-authored the continuing education course, “Boundaries, Self-Care and Meditation” with Nari Clemons.
Do you ever feel like you put more care into treating your patients than do for themselves?
Part 1: Burnout
Let’s get real for a minute.
You are a highly educated professional. If you are reading this blog, I can assume you are invested in your career and your continued education. You are probably pretty skillful, and you help a lot of people.
Faculty members Jenni Gabelsberg DPT, WCS, MSc, MTC and Jennafer Vande Vegte, PT, BCB-PMD, PRPC along with senior Teaching Assistant Quozette Valera PT, DPT will travel to Africa to teach pelvic health in Nairobi City, Kenya through a partnership between Herman & Wallace and The Jackson Foundation. These instructors will be teaching two modules of comprehensive pelvic health training with the goal of creating a self-sustaining, continuous education program taught and offered locally. In addition to training a cohort of physiotherapists in assessing and treating the pelvic floor, these American faculty members will be mentoring local Kenyan therapists to teach these courses in an ongoing manner. We at the Institute are proud and thrilled to be a part of spreading this knowledge and skillset in this currently-underserved region.
The courses offered will comprise H&W's Pelvic Floor Series, with the addition of content relevant to Kenya, including obstetric fistula and female genital mutilation. According to the Worldwide Fistula Fund, there are ~ 2 million women and girls suffering from fistulas. Estimates range from 30 to 100 thousand new cases developing each year; 3-5 cases/1000 pregnancies in low-income countries. A woman may suffer for 1-9 years before seeking treatment. For women who develop fistula in their first pregnancy, 70% end up with no living children.
Have you ever had a dream hidden so deep in your heart you never even spoke it aloud?

I will never forget when my sister, my bestie, told me she wanted to end her life. We were on the phone late one night, tears flowing. Depression was always a companion, but I had never heard her in such a state of despair. We made a plan that she would call the suicide hotline, then call her therapist and her doctor in the morning for urgent care. She made it through the night. Later, I went to her therapist with her so I could better understand and support my sister. She did her due diligence, adjusting medication and staying open and honest in therapy. Suicidal ideations would sometimes flare when there were triggers, but she was able to work through them, and now they are in the past.
Contrast that story with another. Ryan was a sweet woman who developed pudendal neuralgia after a routine hysterectomy. Right away, she told me she had a counselor who she loved who helped her navigate life with DID (Dissociative Identity Disorder) and that I’d probably be interacting with various personalities during our sessions. She helped me understand how to best support her during her care. We worked well together, and although she struggled with both the pain and the unfairness of what happened to her, she was well supported. Then her sweet dog passed away. It was so hard for her. She kept going through pain and heartache and found another pooch to adopt. And then the next visit, she didn’t show. And the next, and the next. And then I found out she was gone. Suicide. This hit me hard. Were there signs that I missed? Was there anything I could have done?
As pelvic rehab providers, we sometimes see people who have intense physical pain often combined with significant emotional wounds. In a study of 713 women seeking support for pelvic pain, 46.8 reported having sexual or physical abuse history, and 31.3 were positive for PTSD (1).
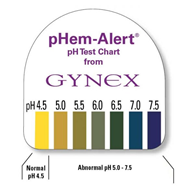
Many years ago a urology doctor shared the skill of testing vaginal pH as part of my pelvic floor exam. I’ve since used it to gather objective data around estrogen status, often finding elevated levels in post-partum, breastfeeding, and peri and post-menopausal women. When correlated with symptoms and visual skin changes this can be a helpful tool to both direct treatment and monitor treatment effectiveness.
To perform pH testing, place a pH strip into the distal vagina. Let it sit there for a few seconds to absorb vaginal moisture. Remove and record results. Any concerning changes in vaginal pH can be documented and reported back to your patient’s medical provider.







A Weekend of Transformation
Let me start this plog (picture/blog?) by saying it had been almost 2 years since Nari Clemons and I taught Boundaries, Self Care, and Meditation for the first time. Nari had some amazing ideas to change some of the course material to reflect more of our hearts’ intention for personal reflection and transformative change. We were excited and nervous to see how our second run of this material would be received. We were also profoundly aware of how the (at times painful) events in our lives that led up to the development of the course have molded and shaped us into much healthier versions of ourselves. We wanted to share a bit about what we have learned and how it has changed us.
We met up in beautiful San Diego on Thursday. Because this course was Saturday to Mononday we had an added bonus of extra time to spend together. We decided to spend our time practicing what we talk about in class.
1. Get out in nature:
Part 3: Carefully Choosing to Say Yes or No (or The Summer that Almost Wasn’t)
*Disclaimer: this essay is meant to be read in a voice of complete transparency and humility.
Two summers ago I was anxiously anticipating a break. I was wrapping up home school for my girls and had scheduled some down time from writing my contribution to “Boundaries, Meditation and Self-Care” when I got the call…
Rewind a bit. Two years prior I also got a call. Would I be interested in writing a chapter in a Urology textbook on alternative care for pelvic pain conditions…edited by and partnering with a big name in pelvic floor rehab? Oh yes indeed I would! I have always dreamed of seeing my name in print. Was I scared out of my mind? Heck yes! I was working 20 hours a week, part time home schooling my girls and teaching for Herman & Wallace. I had one day a week to myself for cleaning, errands, the occasional book reading or interacting with friends. I decided I could spend my next year of Fridays researching, writing and editing said chapter. Oh, I also started therapy for the anxiety increase that came with the project. My therapist suggested I hire help with house cleaning, which I did. She also suggested meditation, mindfulness and using essential oils. I opted not to enact these suggestions. It was a crazy year, but I learned a ton and was proud of my contribution to the publication.




































