At Herman & Wallace, we know that pelvic rehabilitation is a dynamic and ever-evolving field. While foundational courses like Pelvic Function Level 1 and Dry Needling and Pelvic Health often get the spotlight, there are several highly valuable courses that tend to fly under the radar. These courses offer practitioners the opportunity to deepen their knowledge, broaden their skills, and better serve patients with complex needs.
Here are five underrated courses that can have a powerful impact on your practice:
1. Nutrition Perspectives for the Pelvic Rehab Therapist
 Pelvic health doesn’t exist in isolation from the rest of the body, and nutrition plays a critical role in tissue healing, inflammation, digestion, and pelvic pain syndromes. This course introduces pelvic rehab practitioners to the fundamentals of nutrition as it relates to pelvic health.
Pelvic health doesn’t exist in isolation from the rest of the body, and nutrition plays a critical role in tissue healing, inflammation, digestion, and pelvic pain syndromes. This course introduces pelvic rehab practitioners to the fundamentals of nutrition as it relates to pelvic health.
Participants learn how to recognize when dietary factors may be contributing to issues such as constipation, bladder irritation, vulvar pain, or chronic inflammation. While not a course that trains clinicians to act as dietitians, it empowers them to screen for red flags, collaborate with nutrition professionals, and make basic, evidence-informed recommendations that can significantly impact patient outcomes.
2025 Course Date Options: October 11-12, December 6-7.
2. Oncology and the Pelvic Floor Series
 (OPF1: Foundations, OPF2A: Male Pelvic & Colorectal Cancers, and OPF2B: Female Pelvic & Bladder Cancers)
(OPF1: Foundations, OPF2A: Male Pelvic & Colorectal Cancers, and OPF2B: Female Pelvic & Bladder Cancers)
Pelvic health isn’t just for perinatal or orthopedic populations. People undergoing treatment for pelvic and abdominal cancers face unique and complex challenges, including incontinence, pelvic pain, sexual dysfunction, and scar tissue restrictions.
The Oncology and the Pelvic Floor series offers a comprehensive framework for working with patients at every stage of the cancer journey, and provides the knowledge and sensitivity needed to support this underserved population, integrating trauma-informed care, manual therapy, exercise, and interdisciplinary collaboration.
2025 Course Date Options: Level 1 September 13-14, Level 2A December 6-7, Level 2B November 1-2.
3. Pharmacologic Considerations for the Pelvic Health Provider
 Medications have a profound impact on the pelvic floor—often in ways that are overlooked. Whether it’s constipation from opioids, hormonal changes from contraceptives, or bladder irritation from certain antibiotics, understanding pharmacology is crucial.
Medications have a profound impact on the pelvic floor—often in ways that are overlooked. Whether it’s constipation from opioids, hormonal changes from contraceptives, or bladder irritation from certain antibiotics, understanding pharmacology is crucial.
This course demystifies medications commonly encountered in pelvic health practice. It helps clinicians understand how drugs can influence bowel, bladder, sexual function, pain processing, and healing. Armed with this knowledge, practitioners can engage in more informed discussions with patients and other members of the healthcare team, helping to troubleshoot barriers to progress.
2025 Course Date Option: September 13.
4. Yoga for Pelvic Pain
 Yoga is more than stretching—it’s a mind-body practice with proven benefits for nervous system regulation, pain management, and muscular balance. Yoga for Pelvic Pain teaches practitioners how to integrate evidence-based yoga principles into rehabilitation for patients with chronic pelvic pain.
Yoga is more than stretching—it’s a mind-body practice with proven benefits for nervous system regulation, pain management, and muscular balance. Yoga for Pelvic Pain teaches practitioners how to integrate evidence-based yoga principles into rehabilitation for patients with chronic pelvic pain.
This course goes beyond asana (physical postures) to incorporate breathwork, mindfulness, and gentle movement tailored to the needs of people with complex pain syndromes. Participants leave with practical tools they can immediately incorporate into one-on-one sessions or group classes, supporting both physical function and emotional well-being.
2025 Course Date Option: September 13-14.
5. Rehabilitative Ultrasound Imaging: Pelvic Health & Orthopedic Topics
 Rehabilitative Ultrasound Imaging (RUSI) provides real-time feedback for both clinicians and patients. It’s an invaluable tool for assessing muscle activation, motor control, and coordination - particularly for the deep core and pelvic floor muscles.
Rehabilitative Ultrasound Imaging (RUSI) provides real-time feedback for both clinicians and patients. It’s an invaluable tool for assessing muscle activation, motor control, and coordination - particularly for the deep core and pelvic floor muscles.
This course covers both pelvic health applications (like visualizing pelvic floor contractions) and broader orthopedic topics (like assessing the transverse abdominis or multifidus). Practitioners gain hands-on experience in using ultrasound to refine exercise prescription, improve patient engagement, and objectively document progress. Despite its transformative potential, RUSI remains underutilized in many pelvic rehab settings.
2025 Course Date Options for September 5-7: Self-hosted, Indianapolis IN, Seattle WA.
Don’t Overlook These Gems
Expanding your clinical toolbox with specialized knowledge can transform your patient care. Whether it’s understanding how nutrition, medications, cancer treatments, or mind-body practices influence the pelvic floor—or learning to harness the power of ultrasound imaging—these courses provide essential insights that go beyond the basics.
Ready to elevate your practice? Explore these courses and others at Herman & Wallace and continue your journey as a lifelong learner in pelvic rehabilitation.
As a small business owner, I’m grateful to have weathered the COVID-19 storm. When reflecting on the 5 year anniversary of the shutdown, I remember how we adapted day after day — masking up, running air filtration systems, and feeling grateful that we could continue to do our work safely. Yet, despite prioritizing sleep, nourishing my body with fresh food, staying active, and hydrating well, I sometimes still feel myself carrying a lingering undercurrent of stress and tension in my physical body.
We have spent years holding our breath—both literally and figuratively. The weight of collective uncertainty, change, and grief may have left some imprints on our bodies. I was reminded of this when a sudden flare of lumbopelvic pain forced me to pay closer attention to my own breath patterns. It became clear that I needed to soften, to release layer by layer of held tension, and to deepen my own breathwork and meditation practice.
As healthcare providers, our work extends beyond addressing physical concerns. We are honored to hold space for our patients' grief—whether it stems from physical trauma, medical challenges, gaslighting, or life's hardships.
They trust us, not just for guidance on optimizing their pelvic health, but as guides on their healing journeys. And yet, we too are human. We experience burnout, fatigue, and emotional strain.
We often teach our patients that breath is a bridge—connecting the nervous system, digestion, spine, pelvic floor, and our emotional state. It is one of the most powerful tools we have to remind the body that it is safe. And yet, even with this knowledge, we may find ourselves unconsciously holding our breath because we are humans living in this unpredictable and sometimes challenging world. When we resist feeling something, we don’t breathe. When we are afraid, we hold tension in our ribs. Even in moments when we think we are relaxed, we can sometimes still be bracing our jaw, back, or pelvic floor.
Let’s take a moment to pause.
Notice your body. Try not to make any adjustments to “fix” your posture.
- Where is your ribcage in relation to your pelvic floor?
- Does the breath feel deep or shallow, smooth, or restricted?
- Where do you sense movement—your chest, ribs, belly?
- What temperature is the air as it enters your nose?
What does it feel like to exhale?
- Does your breath release with ease or feel held back?
- Can you soften just a little more with each out-breath?
- Notice if there is a natural pause before your next inhale—what does that moment of stillness feel like?
If you're sitting, allow yourself to slouch for a moment.
- How does your breath feel in this position?
- Is it shallow or restricted?
- Now, gently imagine your head and spine being drawn upward, as if a magnet is lifting you toward the ceiling. Take another breath. Does it feel different? Notice any shifts in ease of expansion or softening more fully after the exhale.
Now, let’s zoom into the intercostal spaces.
- Imagine this space expanding with each inhale and softening with each exhale.
- Can you soften any more in your ribcage?
- Picture your shoulders softening, warm water is dripping down the upper trap and down the arms.
- Let your jaw unclench, your tongue relax, the space between your eyebrows melt.
Take another long, conscious breath.
- What do you notice?
- Does your body feel a little softer, a little more open, or is there still a place holding tension, waiting for a little more attention?
As practitioners, we give so much to others all day long and sometimes forget to remember to check in with ourselves. Staying connected to our own breath and body serves us just as much as it serves our patients. When we remain grounded and at ease, we can reduce fatigue, physical discomfort, and emotional exhaustion.
So, let’s remind ourselves—throughout the day—to take long easy breaths, soften our jaws, and allow our bodies to move with greater ease. It is not only a gift to ourselves to prevent burn out, but also helps us facilitate co-regulation with our patients’ nervous systems.
If you enjoyed this article, then join Dustienne in her upcoming remote course Yoga for Pelvic Health, on May 3-4, 2025. This two-day remote course offers participants an evidence-based perspective on the value of yoga for patients with chronic pelvic pain and focuses on two of the eight limbs of Patanjali’s eight-fold path: pranayama (breathing) and asana (postures) and how they can be applied for patients who have hip, back and pelvic pain. The course will describe the role of yoga within the medical model, discuss contraindicated postures, and explain how to incorporate yoga home programs as therapeutic exercise and neuromuscular re-education both between visits and after discharge.
AUTHOR BIO
Dustienne Miller PT, MS, WCS, CYT

Dustienne Miller PT, MS, WCS, CYT (she/her) is the creator of the two-day course Yoga for Pelvic Pain and an instructor for Pelvic Function Level 1. Born out of an interest in creating yoga home programs for her patients, she developed a pelvic health yoga video series called Your Pace Yoga in 2012. She is a contributing author in two books about the integration of pelvic health and yoga, Yoga Mama: The Practitioner’s Guide to Prenatal Yoga (Shambhala Publications, 2016) and Healing in Urology (World Scientific). Prior conference and workshop engagements include APTA's CSM, International Pelvic Pain Society, Woman on Fire, Wound Ostomy and Continence Society, and the American Academy of Physical Medicine and Rehabilitation Annual Assembly.
Her clinical practice, Flourish Physical Therapy, is located in Boston's Back Bay. She is a board-certified women's health clinical specialist recognized by the American Board of Physical Therapy Specialties. Dustienne weaves yoga, mindfulness, and breathwork into her clinical practice, having received her yoga teacher certification through the Kripalu Center for Yoga and Health in 2005.
Dustienne's love of movement carried over into her physical therapy and yoga practice, stemming from her previous career as a professional dancer. She danced professionally in New York City for several years, most notably with the national tour of Fosse. She bridged her dance and physical therapy backgrounds working for Physioarts, who contracted her to work backstage at various Broadway shows and for the Radio City Christmas Spectacular. She is currently an assistant professor of jazz dance at Boston Conservatory at Berklee.
Dustienne passionately believes in the integration of physical therapy and yoga within a holistic model of care. Her course aims to provide therapists and patients with an additional resource centered on supporting the nervous system and enhancing patient self-efficacy.
Before we talk about yoga, let’s do a quick overview of interstitial cystitis/bladder pain syndrome.
In 2022, the American Urological Association updated the clinical guidelines on the treatment of interstitial cystitis/bladder pain syndrome. Prior to this revision, pelvic physical (and occupational) therapy was considered first-line treatment with evidence strength grade A. After this revision, the AUA recommends looking at the phenotype of the patient to determine which treatment categories would best serve the individual patient.
Three phenotypes have been identified: a bladder-centric phenotype, a pelvic floor phenotype, and a phenotype that experiences widespread symptoms with chronic overlapping pain conditions.
Treatment categories include behavioral/non-pharmacologic, oral medicines, bladder instillations, procedures, and major surgery.
There are three guideline statements that are within our scope of practice as rehab professionals.
Guideline Statement 10: “Self-care practices and behavioral modifications that can improve symptoms should be discussed and implemented as feasible. Clinical Principle”
This is the space that pelvic PTs and OTs live in every day. The recommended treatments within our scope of practice include:
- evaluating the concentration and/or volume of urine
- limiting bladder irritants
- an elimination diet to determine which foods or fluids are triggering
- thermal modalities (eg, suprapubic or perineal heat or cold)
- strategies to manage IC/BPS flare-ups (eg, meditation, imagery)
- pelvic floor muscle relaxation
- bladder retraining
- avoiding pain-provoking exercise
- managing constipation
Guideline Statement 12: “Appropriate manual physical therapy techniques (eg, maneuvers that resolve pelvic, abdominal, and/or hip muscular trigger points, lengthen muscle contractures, and release painful scars and other connective tissue restrictions), if appropriately trained clinicians are available, should be offered to patients who present with pelvic floor tenderness. Pelvic floor strengthening exercises (eg, Kegel exercises) should be avoided. Standard (Evidence Strength: Grade A)”
As therapists, we will often also evaluate the spine and perhaps further up and down the chain to look for potential contributing factors. While this was not mentioned in the guideline paper, it is often how we holistically treat each individual who walks into our office.
But wait! There’s more! We can also help coach our patients on one more clinical principle….
Guideline Statement 11: “Patients should be encouraged to implement stress management practices to improve coping techniques and manage stress-induced symptom exacerbations. Clinical Principle”
Remember back in guideline 10 when it listed “strategies to manage IC/BPS flare-ups (eg, meditation, imagery) and pelvic floor muscle relaxation”? Clinically we use breathwork, pain neuroscience, and gentle stretching. Some practitioners use yoga as an adjunct modality in the clinic and for home programs.
Khandwala et al looked at 8 patients during 3 months of integrated yoga therapy. There was a statistically significant improvement in two areas of the SF-36 (social function and pain). There was a non-statistically significant trend towards improved voiding volumes.
Dao et al looked at 97 patients assigned to the control group (usual care) or intervention group (usual care plus yoga and meditation). The intervention group showed faster improvement during the clinical trial. Additionally, there were decreases in anxiety, depression, pain interference, and pain scores.
I (Dustienne) created the two flows for the Dao study, and I’m absolutely thrilled to see echoed in the research what we see clinically - downregulation of the nervous system, breathwork, visualization, and mindful movement support our patients and offer additional strategies for resilience.
For free access to the two videos used in the study, visit: https://www.yourpaceyoga.com/interstitial-cystitis-yoga
Dustienne Miller developed her course Yoga For Pelvic Pain in 2012. She enjoys seeing the research grow and supports how she and her colleagues have been practicing in pelvic health over the years. Remote course offerings for 2025 are: February 22-23, May 3-4, and September 13-14.
References:
- Clemens, J. Q., Erickson, D. R., Varela, N. P., & Lai, H. H. (2022). Diagnosis and Treatment of Interstitial Cystitis/Bladder Pain Syndrome. Journal of Urology, 208(1), 34–42. https://doi.org/10.1097/JU.0000000000002756 (Original work published July 1, 2022)
- Dau, A., Meriwether, K.V., Petersen, T., Jansen, S. & Komesu, Y. Mindfulness and Yoga for Pain with Interstitial Cystitis Evaluation: An RCT
- FitzGerald, M. P., Anderson, R. U., Potts, J., Payne, C. K., Peters, K. M., Clemens, J. Q., ... & Nyberg, L. M. (2009). Urological Pelvic Pain Collaborative Research Network Randomized multicenter feasibility trial of myofascial physical therapy for the treatment of urological chronic pelvic pain syndromes. J. urol, 182(2), 570-580.
- Khandwala, S., & Cruff, J. (2020). The Role of Yoga in the Management of Bladder Pain Syndrome: A Single-Arm Pilot Study. Advances in mind-body medicine, 34(4), 4–9.
- Rovner, E., Propert, K. J., Brensinger, C., Wein, A. J., Foy, M., Kirkemo, A., ... & Interstitial Cystitis Data Base Study Group. (2000). Treatments used in women with interstitial cystitis: the interstitial cystitis database (ICDB) study experience. Urology, 56(6), 940-945.
Author Bio:
Dustienne Miller PT, MS, WCS, CYT

Dustienne Miller is the creator of the two-day course Yoga for Pelvic Pain and an instructor for Pelvic Function Level 1. Born out of an interest in creating yoga home programs for her patients, she developed a pelvic health yoga video series called Your Pace Yoga in 2012. She is a contributing author in two books about the integration of pelvic health and yoga, Yoga Mama: The Practitioner’s Guide to Prenatal Yoga (Shambhala Publications, 2016) and Healing in Urology (World Scientific). Prior conference and workshop engagements include APTA's CSM, International Pelvic Pain Society, Woman on Fire, Wound Ostomy and Continence Society, and the American Academy of Physical Medicine and Rehabilitation Annual Assembly.
Her clinical practice, Flourish Physical Therapy, is located in Boston's Back Bay. She is a board-certified women's health clinical specialist recognized by the American Board of Physical Therapy Specialties. Dustienne weaves yoga, mindfulness, and breathwork into her clinical practice, having received her yoga teacher certification through the Kripalu Center for Yoga and Health in 2005.
Dustienne's love of movement carried over into her physical therapy and yoga practice, stemming from her previous career as a professional dancer. She danced professionally in New York City for several years, most notably with the national tour of Fosse. She bridged her dance and physical therapy backgrounds working for Physioarts, who contracted her to work backstage at various Broadway shows and for Radio City Christmas Spectacular. She is an assistant professor of musical theater and jazz dance at the Boston Conservatory at Berklee.
Dustienne passionately believes in the integration of physical therapy and yoga within a holistic model of care. Her course aims to provide therapists and patients with an additional resource centered on supporting the nervous system and enhancing patient self-efficacy.
As musculoskeletal specialists, we are adept at identifying postural dysfunction. I often explain to patients how their ribcage might shift posteriorly relative to the plumb line and how gravity can amplify forces on specific structures. To help patients understand the difference between their habitual non-optimal posture and a more optimally aligned posture, many occupational and physical therapists use the IPA’s Vertical Compression Test (VCT). This test effectively demonstrates how improved alignment facilitates better weight transfer through the base of support. Sometimes this test reproduces back or pelvic pain which allows the patient to understand how their posture might be a contributing factor to them not feeling their best. In addition to the VCT, I incorporate Mountain Pose as an additional kinesthetic tool for postural retraining.
 Many moons ago, I was working with a lovely client on embodied postural awareness using Mountain Pose. I suggested she could close her eyes if she felt comfortable (some people will feel safer lowering their gaze instead of closing their eyes). Working from the ground up, she realized her weight was predominantly in her heels. When I guided her to shift her weight forward by hinging from the talocrural joint, she experienced an “aha moment,” saying, “It feels like my pelvic floor just sighed.” She hadn’t been aware that her habitual posture involved standing with her weight behind the plumb line, which contributed to overactivity of the posterior pelvic floor. Once she adjusted her base of support from the ground up, she felt a significant release in her habitual tension.
Many moons ago, I was working with a lovely client on embodied postural awareness using Mountain Pose. I suggested she could close her eyes if she felt comfortable (some people will feel safer lowering their gaze instead of closing their eyes). Working from the ground up, she realized her weight was predominantly in her heels. When I guided her to shift her weight forward by hinging from the talocrural joint, she experienced an “aha moment,” saying, “It feels like my pelvic floor just sighed.” She hadn’t been aware that her habitual posture involved standing with her weight behind the plumb line, which contributed to overactivity of the posterior pelvic floor. Once she adjusted her base of support from the ground up, she felt a significant release in her habitual tension.
At our follow-up visit, the client noted an increase in her postural awareness. She was surprised by how frequently she noticed her pelvic floor gripping in a state of overactivity. She also reported enhanced awareness during her standing yoga postures in class. Grounding down through the feet, cued as imagining the soles of the feet getting magnetically drawn into the floor, can be a useful verbal cue to assist with letting go of unnecessary gripping. The experience of achieving embodied optimal alignment has given her greater self-efficacy, and she’s successfully translated this improved postural awareness into her daily life. Self-awareness and empowerment are central goals in my physical therapy practice, and integrating yoga into this process makes my clinical work even more fulfilling.
To learn more, join Dustienne in her remote course Yoga for Pelvic Pain this September 14-15! This course discusses a variety of pelvic conditions including interstitial cystitis/painful bladder syndrome, vulvar pain, coccydynia, hip pain, and pudendal neuralgia. Dustienne also describes the role of yoga within the medical model, contraindicated postures, and how to incorporate yoga home programs as therapeutic exercise and neuromuscular re-education both between visits and after discharge in this course.
Author Bio:
Dustienne Miller PT, MS, WCS, CYT

Dustienne Miller is the creator of the two-day course Yoga for Pelvic Pain and an instructor for Pelvic Function Level 1. Born out of an interest in creating yoga home programs for her patients, she developed a pelvic health yoga video series called Your Pace Yoga in 2012. She is a contributing author in two books about the integration of pelvic health and yoga, Yoga Mama: The Practitioner’s Guide to Prenatal Yoga (Shambhala Publications, 2016) and Healing in Urology (World Scientific). Prior conference and workshop engagements include APTA's CSM, International Pelvic Pain Society, Woman on Fire, Wound Ostomy and Continence Society, and the American Academy of Physical Medicine and Rehabilitation Annual Assembly.
Her clinical practice, Flourish Physical Therapy, is located in Boston's Back Bay. She is a board-certified women's health clinical specialist recognized by the American Board of Physical Therapy Specialties. Dustienne weaves yoga, mindfulness, and breathwork into her clinical practice, having received her yoga teacher certification through the Kripalu Center for Yoga and Health in 2005.
Dustienne's love of movement carried over into her physical therapy and yoga practice, stemming from her previous career as a professional dancer. She danced professionally in New York City for several years, most notably with the national tour of Fosse. She bridged her dance and physical therapy backgrounds working for Physioarts, who contracted her to work backstage at various Broadway shows and for Radio City Christmas Spectacular. She is an assistant professor of musical theater and jazz dance at the Boston Conservatory at Berklee.
Dustienne passionately believes in the integration of physical therapy and yoga within a holistic model of care. Her course aims to provide therapists and patients with an additional resource centered on supporting the nervous system and enhancing patient self-efficacy.
The popularity of yoga continues to rise with over 36 million yogis living in the United States of America and over 300 million practitioners worldwide. Yoga has several therapeutic effects that make it a beneficial addition to home exercise programs for practitioners and personal practice.
Dustienne Miller discussed some of the benefits of yoga in her March blog (March 8, 2022 - A yoga practice can change your neuroanatomy!). These benefits extend beyond the musculoskeletal system and include improved mood and depression, changes in pain perception, improved mindfulness and associated improved pain tolerance, and the ability to observe situations with emotional detachment.
The physical benefits are well documented in several research studies and include improved flexibility, strength, and stability as well as enhanced respiratory and cardiovascular function. Supporting documentation also shows that yoga can help alleviate the symptoms of chronic pain. Dustienne Miller shared that in a study by Villemure et al, they determined “that the insula-related interoceptive awareness strategies of the yoga practitioners being used during the experiment correlated with the greater intra-insular connectivity...concluding that the insular cortex can act as a pain mediator for yoga practitioners.”
Restorative yoga shares the many benefits seen in other styles of yoga and can also be a great addition to home programs for pelvic rehab practitioners. Kate Bailey shared in her interview with The Pelvic Rehab Report (August 31, 2021 – Faculty Interview: Kate Bailey) that restorative yoga “focuses on the lesser-known aspects of the yoga platform: breath, restorative practice, and a bit of meditation. I have clients all the time who struggle with meditation because their nervous systems aren’t ready for it. So we look at breathing and restorative yoga both as independent alternatives, but also as a way to get closer to meditation.. giving the clinicians another skill for their own rest practice can be useful when feeling tired, overwhelmed, or burned out. “
But what does this mean? Let’s look at some of these aspects a bit closer:
Improving mood and sleep: This includes depression, anxiety, and even stress or other mood disorders. Consistent yoga practice can lead to significant increases in serotonin levels coupled with decreases in the levels of monoamine oxidase, an enzyme that breaks down neurotransmitters and cortisol(1). Yoga can inhibit the areas in the brain responsible for fear, aggressiveness, and rage (posterior or sympathetic area of the hypothalamus) – while simultaneously stimulating the rewarding pleasure centers in the median forebrain and other areas leading to a state of bliss and pleasure. This inhibition results in lower anxiety, heart rate, respiratory rate, blood pressure, and cardiac output (2).
Think about it. Deep breathing calms the nervous system. This promotes relaxation. The more relaxed you are then the better the chance of having a good night’s sleep. Consistent yoga practice can also assist sleep quality by increasing melatonin and reducing hyperarousal (3). Pratyahara, or a turning inward of the senses, allows downtime for the nervous system and can be encouraged by yoga poses such as savasana (corpse pose) and pranayama (breathing exercises/control.
Reduced Chronic Pain: Asana and meditation have been shown to reduce chronic pain including reduced pain from arthritis, back pain, and other chronic conditions while also improving balance and increasing proprioception(1). Yoga sessions can take our joints through a full range of motion. This squeezes and soaks areas of cartilage not often used and provides fresh nutrients, oxygen, and blook to the joints. Otherwise neglected areas of cartilage in the joints would wear out, exposing bone, which can lead to arthritis and chronic pain. At the same time, yoga is gentle on the body and consistent practice can strengthen the connective tissues that surround the bones and joints.
Effects on Cancer Patients: Yoga cannot cure cancer, but it can reduce stress and improve physical, emotional, and spiritual wellness. There is supporting research that the growth of cancerous tumors can be exacerbated by stress(4). This same study found that consistent yoga practice could decrease post-chemotherapy-induced frequency and intensity of nausea and the intensity of anticipatory nausea and vomiting. In 2018 Lin et al provided new research showing that restorative yoga can decrease depression in cancer survivors; improve symptoms of anxiety, depression, and pain symptoms in cancer patients; and help patients manage the toxicity of cancer treatments (5). In addition, yoga has a fundamental emphasis placed on mindfulness and acceptance of your body and its limitations.
Kate Bailey likes to joke about lying on the floor, but really, it is not a joke at all. Lying on the floor for 15 minutes is savasana. She shares that “Savasana is a wakeful resting and a practice of relaxation response. It seems easy: you always have access to a floor. You don’t need anything fancy. Aside from the neuroregulatory benefits of rest, savasana also gives the postural muscles a break. It allows the hip flexors to re-lengthen and the cervicothoracic junction to realign.”
Let’s take a moment to close with a savasana (did you know that a 5-minute savasana is recommended for every 30 minutes of yoga?). This pose can calm the central nervous system, aid the digestive and immune systems, reduce headaches, fatigue, and anxiety while lowering blood pressure and calming the mind, and reducing stress.
Take a moment and lay on the floor with your arms and legs open wide and relaxed (starfish style), supported by a bolster, or you may want to place your hands gently over your chest or your stomach. Now gently still your body. Release your breath and be present. Be completely aware of the moment. Let your mind and body go for a few moments.
Namaste.
References:
- McCall T. New York: Bantam Dell a division of Random House Inc; 2007. Yoga as Medicine.
- Woodyard C. Exploring the therapeutic effects of yoga and its ability to increase quality of life. International journal of yoga, 4(2), 49–54. 2011. doi: 10.4103/0973-6131.85485
- Wang W-L, Chen K-H, Pan Y-C, Yang S-N, Chan Y-Y. The effect of yoga on sleep quality and insomnia in women with sleep problems: A systematic review and meta-analysis. BMC Psychiatry. 2020;20(1):195. doi:10.1186/s12888-020-02566-4
- Carson, J. W., Carson, K. M., Porter, L. S., Keefe, F. J., Shaw, H., & Miller, J. M. (2007). Yoga for women with metastatic breast cancer: results from a pilot study. Journal of pain and symptom management, 33(3), 331–341.
- Lin P-J, Peppone LJ, Janelsins MC, et al. Yoga for the management of cancer treatment-related toxicities. Curr Oncol Rep. 2018;20:5. doi:10.1007/s11912-018-0657-2
 Restorative Yoga for Physical Therapists with instructor Kate Bailey
Restorative Yoga for Physical Therapists with instructor Kate Bailey
This course will provide the basis for experiencing and integrating restorative yoga into physical therapy practice. Restorative yoga is an accessible practice that can teach patients (and practitioners) how to rest systematically, for short periods of time, on a regular basis to encourage the parasympathetic nervous system to balance with the sympathetic nervous system for improved neuroregulation. Topics include the difference between meditation and restorative yoga, and how they can support each other in order to support the ability to drop into relaxation. Restorative postures, each taking 20-30 minutes are offered prior to the live meeting so that participants can experience what a patient might experience when restorative yoga is a component of their home program. Then in the live course participant experiences, questions, and strategies on how to reduce barriers to relaxation so that patients can integrate this practice into their lifestyle will be discussed. There will also be live labs for breathing techniques and specific meditations that may be helpful to patients working with an unregulated nervous system.
 Yoga for Pelvic Pain with instructor Dustienne Miller
Yoga for Pelvic Pain with instructor Dustienne Miller
This course offers an evidence-based perspective on the value of yoga for patients with chronic pelvic pain by focusing on two of the eight limbs of Patanjali’s eightfold path: pranayama (breathing) and asana (postures) - and how they can be applied for patients who have hip, back and pelvic pain. A variety of pelvic conditions will be discussed including interstitial cystitis/painful bladder syndrome, vulvar pain, coccydynia, hip pain, and pudendal neuralgia. Lecture topics include the role of yoga within the medical model, contraindicated postures, and how to incorporate yoga home programs as therapeutic exercise and neuromuscular re-education both between visits and after discharge.
Hi Kate, can you tell us about the course you have designed Restorative Yoga for Physical Therapists?
My name is Kate Bailey and I am a pelvic floor physical therapist. I’ve been a pelvic floor PT going on4-5 years now. Before that, I’ve been a pilates instructor for 20 years and taught yoga for over a decade. This course is a culmination of all of my experiences both with the yoga, pilates, and the pelvic floor population from kiddos through adulthood. It allows us to use the techniques from the yoga and pilates philosophies to support people in their healing process from pelvic pain and also just in their bodies.
What can participants expect to learn when they come to the course?
I wrote this course when the pandemic started. My whole intention was to make the didactic information self-paced and watch the videos as often as you want kind of course. This way, when we have dedicated time together it’s a lot more about discussion and me guiding people through the labs, and in turn, they can guide their colleagues or patients. It is designed so I’m not spending a lot of time lecturing to a screen and our time dedicated to each other is more about a conversation. I want people to learn about the information in their own time, marinate in it a little bit, and then come with questions.
How do you feel that restorative yoga fits in with the care we provide to our patients with pelvic health conditions?
The restorative yoga component to me is really special because it’s one of the only times we prioritize rest, and not doing, and sitting with ourselves. Not necessarily trying to get strong, or trying to get more flexible. It’s really about allowing our bodies to be. Sometimes that is being in a little bit of discomfort. Sometimes that is just being with the exhaustion that I think we all have a little bit of. Just learning how to be with ourselves for 8, to 12, to 15 minutes and see that as a really productive part of our treatment plan.
How does trauma-informed care influence your course?
One of the things that I highlight in the course is how much trauma occurs in and around the home. So when we’re asking patients to do a home program one of the discussion points we have in the course is “what if the home is inherently triggering or unsafe?” How can we use concepts of graded exposure to get someone from needing a lot of sensory things, like lights on, windows locked, facing the window, eyes open to slowly getting people toward a little bit more safety. If that is not a possibility, finding another location and strategizing how we can prioritize our own safety and our own ability to relax rather than saying I must relax.
The other component of trauma in the course is the unveiling of how prevalent trauma is. In pelvic health, we talk a lot about sexual trauma because we are dealing a lot with the pelvic floor region and the genitals. One of the things I think we sometimes might be able to speak to more is the little subversive types of trauma. Whether it is emotional trauma, whether it is neglect, whether it is transgenerational trauma or intersectionality trauma…
There’s this other component in yoga that is coming out now that is the trauma that has been handed down through the yoga lineages. What I think is not understood is that a lot of people who practice yoga in a deep way have significant trauma from yoga. The question then is how do we reclaim a practice that is so lovely, done with care and kindness and non harming, for people who have maybe experienced it in a very harmful way – and introduce it as a non-harming, caring, compassionate method for people who haven’t experienced it. The whole idea is about how do you be in rest in your body and in empowerment.
Can you give an example of how a pelvic PT or OT would fit restorative yoga into their practice?
As PTs and Ots we are starting to bring mindfulness in, a lot, to our programming in terms of some of the work from Jon Kabat Zen on how great meditation is for so many things. There is still a question of “How do I put this in my plan of care?” The great thing about this class is that we can speak directly to this. Let's say that you are in a hospital-based scenario, you can give restorative yoga to someone n a hospital bed very easily. They’re not going anywhere and what a great thing to give them: a breathing practice, a concentration practice, and a rest practice.
For someone in private practice, such as orthopedics, this is the type of practice where maybe you’re not giving pelvic floor strengthening if someone has a large degree of overactivity in their pelvic floor. But they still need something to do at home, or they need something to do at the office. Maybe restorative yoga is a little bit too far out there for the patient. Maybe they don’t have a space they can lie down on the floor. That’s when we can say, ok how can we then transfer a pelvic floor restorative yoga posture to a desk situation? Can you cross your legs on your chair and lean forward, and modify it that way.
Then there is this component of the class that is all about breathing. I think we know in pelvic health how wonderful and how great breath-work can be and so some of these techniques can be used as ‘secret exercises’ in your everyday life in addition to being a dedicated practice. We talk about all of that in class.
Watch the full interview with Kate Bailey at the Herman & Wallace YouTube Channel:
Join Kate to learn more about including restorative yoga into your practice with Restorative Yoga for Physical Therapists this year. Courses are scheduled for:
Dustienne Miller, CYT, PT, MS, WCS instructed the H&W remote course Yoga for Pelvic Pain. Dustienne passionately believes in the integration of physical therapy and yoga in a holistic model of care, helping individuals navigate through pelvic pain and incontinence to live a healthy and pain-free life. You can find Dustienne Miller on Instagram at @yourpaceyoga
Research demonstrates multiple benefits of a yoga practice that extend beyond the musculoskeletal system. These benefits include improved mood and depression, changes in pain perception, improved mindfulness and associated improved pain tolerance, and the ability to observe situations with emotional detachment.
Do the brains of yoga practitioners vs non-practitioners look different?
A study by Villemure et al looked at the role the insular cortex plays in mediating pain in the brains of yoga practitioners. They included various styles of yoga to capture the essence of yoga across multiple styles - Vinyasa, Ashtanga, Kripalu, Sivananda, and Iyengar.
Rewind back to neuroanatomy class - remember the insular cortex? The insular cortex is responsible for sensory processing, decision-making, and motor control by communicating between the cortical and subcortical aspects of the brain. The outside inputs include auditory, somatosensory, olfactory, gustatory, and visual. The internal inputs are interoceptive (Gogolla).
Villemure et al found several interesting objective differences. The practitioners had increased grey matter volume in several areas of the brain. This increase in grey matter specifically in the insula correlated with increased pain tolerance. The length of time practiced correlated with increased grey matter volume of the left insular cortex. Additionally, white matter in the left intrainsular region demonstrated more connectivity in the yoga group.
Other differences were seen in strategies utilized to manage pain. Most folks in the yoga group expected their practice would decrease reactivity to pain, which it did. The yoga group used parasympathetic nervous system accessing strategies and interoceptive awareness. These strategies were breathwork, noticing and being with the sensation, encouraging the mind and body to relax, and acceptance of the pain. The control group strategies were distraction techniques and ignoring the pain.
The authors determine that the insula-related interoceptive awareness strategies of the yoga practitioners being used during the experiment correlated with the greater intra-insular connectivity. Therefore, the authors conclude that the insular cortex can act as a pain mediator for yoga practitioners.
The more strategies our patients have for pain management, the better! Yoga is one of several non-invasive modalities our patients can add to their healing toolbox.
Yoga for Pelvic Pain was developed by Dustienne Miller to offer participants an evidence-based perspective on the value of yoga for patients with chronic pelvic pain. This course focuses on two of the eight limbs of Patanjali’s eightfold path: pranayama (breathing) and asana (postures) and how they can be applied for patients who have hip, back, and pelvic pain.
A variety of pelvic conditions are discussed including interstitial cystitis/painful bladder syndrome, vulvar pain, coccydynia, hip pain, and pudendal neuralgia. Other lectures discuss the role of yoga within the medical model, contraindicated postures, and how to incorporate yoga home programs as therapeutic exercise and neuromuscular re-education both between visits and after discharge.
References:
Gogolla N. The insular cortex. Current Biology. 2017; 27(12): R580-R586.
Villemure C, Ceko M, Cotton VA, Bushnell MC. Insular cortex mediates increased pain tolerance in yoga practitioners. Cereb Cortex. 2014 Oct;24(10):2732-40. doi: 10.1093/cercor/bht124. Epub 2013 May 21. PMID: 23696275; PMCID: PMC4153807.

This week The Pelvic Rehab Report sat down with Kate Bailey, PT, DPT, MS, E-RYT 500, YACEP, Y4C, CPI to discuss her career as a physical therapist and upcoming course, Restorative Yoga for Physical Therapists, scheduled for September 11-12, 2021. Kate’s course combines live discussions and labs with pre-recorded lectures and practices that will be the basis for experiencing and integrating restorative yoga into physical therapy practice. Kate brings over 15 years of teaching movement experience to her physical therapy practice with specialties in Pilates and yoga with a focus on alignment and embodiment.
Who are you? Describe your clinical practice.
My name is Kate Bailey. I own a private practice in Seattle that focuses on pelvic health for all genders and ages. I work under a trauma-informed model where patient self-advocacy and embodiment are a priority. My dog, Elly, assists in my practice by providing a cute face and some calming doggy energy. My patients often joke that they come to see her just as much as to see me, which I think is great. In addition to being a physical therapist, I’ve been teaching Pilates for nearly 20 years and yoga for over 10. They are both big parts of my practice philosophy and my own personal movement practice
What books or articles have impacted you as a clinician?
I have a diverse library of Buddhist philosophy, emotional intelligence, trauma psychology, human behavior, breathwork/yoga, and sociology and, of course, a bunch of physical therapy pelvic floor books. I also love a children’s book on emotional regulation or inclusion, even for adults. One of my favorite finds is the Spot series that gives kiddos different ways to use their hands to help deal with different emotions. I’ve used it for adults who need physical self-soothing options. There are so many, and I find that it's the amalgamation of information that really impacts my practice the most.
How did you get involved in the pelvic rehabilitation field?
I have a deep interest in the human experience and how culture and dissociation create mass-disembodiment and how hands-on work can be profound in how we experience our body. Pelvic rehab allowed me the opportunity to work more closely with people on areas that bring up the most shame, disembodiment, and trauma, and therefore have some pretty amazing possibilities to make an impact not only in their lives but how they act in culture. In many ways, I see my work in pelvic rehab as a point of personal activism in creating a more embodied, empowered, and powerful culture.
What has your educational journey as a pelvic rehab therapist looked like?
I knew I wanted to go into pelvic health from my second year in PT school. I’ve always been at bit…well, let’s call it driven. I did an internship with great therapists in Austin and then only considered full-time pelvic floor positions once licensed. I took as many courses as I could handle in my first couple years of practice, which worked well for me, but understandably is not the right path for all those entering this field for a number of reasons. I went through the foundational series, and then into visceral work as well as continued my yoga and Pilates studies. I continued my education in trauma and emotional intelligence which is both a personal and professional practice. I found that a blend of online coursework and in-person kept me satisfied with my educational appetite.
What made you want to create your course, Restorative Yoga for Physical Therapists?
I was a yoga teacher long before I became a PT. When I found my way into the specialty of pelvic floor physical therapy, this particular part of my yoga teaching became incredibly useful for patients who had high anxiety, high stress, and difficulty with relaxation and/or meditation. This course was a way for me to share some of my knowledge of restorative yoga with the community of health care providers, where it could not only be used as a means of helping patients, but also as a means to start valuing rest as a primary component of wellbeing.
What need does your course fill in the field of pelvic rehabilitation?
Learning about yoga as a full practice and understanding that it has many components is very useful in deciding which component would be a good match for a pelvic health patient. Is it strengthening from an active practice? Is it meditation or pranayama (breath manipulation)? Or is it supported rest? This particular course focuses on the lesser-known aspects of the yoga platform: breath, restorative practice, and a bit of meditation. I have clients all the time struggle with meditation because their nervous systems aren’t ready for it. So we look at breathing and restorative yoga both as independent alternatives, but also as a way to get closer to meditation. Learning how to help people rest, the different postures, how to prop, and how to dose is an important component of this class. As a bonus, giving the clinicians another skill for their own rest practice can be useful when feeling tired, overwhelmed, or burned out. All this under a trauma-informed, neuro-regulation-focused model is a lovely way to deepen one’s physical therapy practice.
What demographic, would benefit from your course?
People who are stressed out or who work with people who are stressed out. In particular, clinicians who work with people who have pelvic pain or overactivity in their pelvic floors.
What patient population do you find most rewarding in treating and why?
I love working with female-identifying patients that struggle with sexual health or those who are hypermobile and trying to figure out movement that feels good. I love working with all genders generally and do so regularly. There’s nothing quite like helping a male-identifying patient find embodiment and understanding of their pelvis in a new way. I think for me, working to dismantle female normative structures for those identifying as female, particularly in the realm of sexual health feels inspiring to me because it combines physical, emotional, spiritual health with going against the cultural standards of how those identifying as women fit into society, and being able to sit with the trauma of all types that so many people face.
What do you find is the most useful resource for your practice?
A pelvic floor model is great. The most important part of my practice is a conversation about consent, not only for internal work but for everything I offer during visits and also for patients to understand that they can give or retract consent with any medical provider for just about any service. Emergency procedures are a smidge different, but I hope my patients walk away with the understanding that the medical community is here to serve their embodied experience. My newest favorite resource is a series of metal prints that depict the emotional intelligence grid used in the RULER syllabus. I have a magnet that patients can use to identify how they are feeling and help develop their language for emotional and then somatic or interoceptive knowledge.
What has been your favorite Herman & Wallace Course and why?
There was nothing quite like PF1. I don’t think I’ll ever forget it. The instructors were Stacey Futterman Tauriello and Susannah Haarmann. I was still in grad school prepping for my internship and ended up being the model for labs which falls squarely in line with my upbringing as a dancer who wanted to understand everything from the inside out. It was a challenging weekend on pretty much every level. I went through phases of dissociation and total connection. It made me realize that my decision to enter health care after having a career in movement was the right one.
What lesson have you learned from a course, instructor, colleague, or mentor that has stayed with you?
Meet the patient where they are at first and validate that they live in an incredibly intelligent body. I think sometimes it’s so exciting to see the potential that patients have because, as clinicians, we’ve seen the progress of others. In yoga, there is a practice of the beginner’s mind. It asks the student to sit with an empty cup of knowledge and experience each practice with the curiosity of someone just being introduced to yoga. I have knowledge that may be helpful to patients. Patients have so much knowledge of their own body from their life experiences, some of which are conscious and so much of which is subconscious. The fun part is seeing how my experience and their experience match (or don’t sometimes) to then assess how to craft the care plan.
If you could get a message out to other clinicians about pelvic rehab what would it be?
That it's so much more than pelvic rehab. We get to talk to people about things that aren’t talked about and normalize the human experience. Pelvic rehab gives safety to patients to experience their bodies in all the sensations that come from having a nervous system: from sadness to joy to relief to fear. It's all in there and when we learn about those sensations from pelvic rehab, my hope is that it can flood into other areas of life.
What is in store for you in the future as a clinician?
Refining, learning, and seeing what else comes. Hoping to publish a book of cartoon organs shortly. But most importantly to create a safe space for patients to feel cared for and supported in my corner of Seattle.
Kate Bailey (She/Her)
Pelvic Floor Physical Therapy
Yoga & Pilates
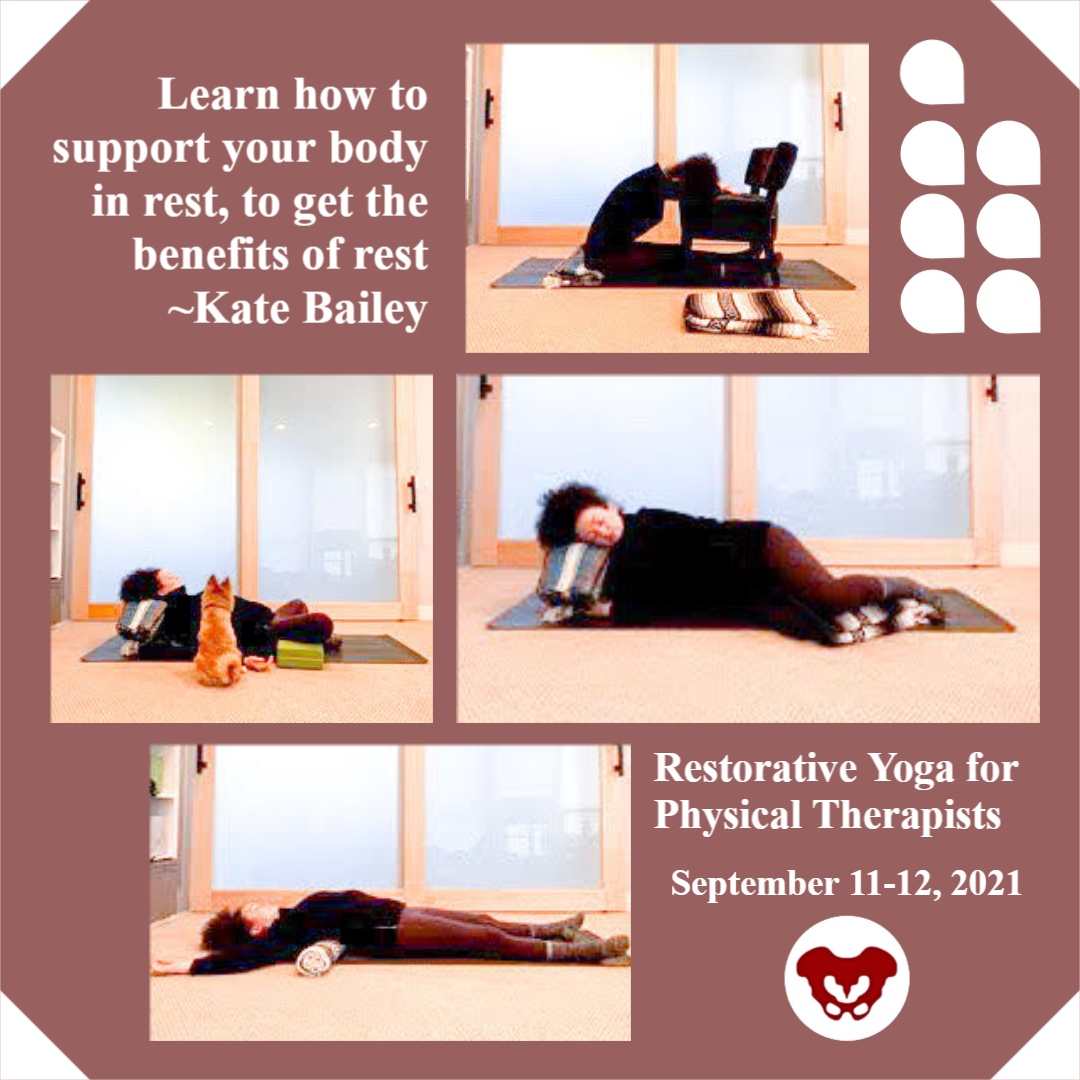
Kate Bailey, PT, DPT, MS, E-RYT 500, YACEP, Y4C, CPI curated and instructs the remote course on Restorative Yoga for Physical Therapists, which is scheduled for September 11-12, 2021. Kate brings over 15 years of teaching movement experience to her physical therapy practice with specialties in Pilates and yoga with a focus on alignment and embodiment. Kate’s pilates background was unusual as it followed a multi-lineage price apprenticeship model that included the study of complementary movement methodologies such as the Franklin Method, Feldenkrais, and Gyrotonics®. Building on her Pilates teaching experience, Kate began an in-depth study of yoga, training with renown teachers of the vinyasa and Iyengar traditions. She held a private practice teaching movement prior to transitioning into physical therapy and relocating to Seattle.
Without a doubt, these past couple of years have been tough with this global pandemic of a virus that caused major shifts in how we work, play, learn and socialize. Wherever you live on this planet, it is nearly impossible not to have been affected by the stress and trauma that the Covid-19 virus has created. Just like with any other stressor, the first step of management is recognition. Check, done.
Step two involves making conscious choices about how we want to live. This is where we have some options, including self-care. “Self-care” is one of my least favorite phrases. Not because at its core, self-care is not important. But because it's another thing on an overflowing to-do list and can create even more of a sense of imbalance, lack of accomplishment, and self-defeat. Yet, learning how to manage stress is a skill we all need: individually and communally.
However, there is a step before stress management that we need to address first. Interoception, defined by Porges, Ph.D., is the process that describes both conscious feelings and unconscious monitoring of bodily processes by the nervous system. As a clinician, this is a key aspect of every single patient care plan. I am a big fan of embodied decision making, and yet our somatic intelligence (or interoceptive skills) is widely underdeveloped.
Just as emotional intelligence is getting some wonderful development, through the work of researchers and educators like Marc Brackett, Ph.D. of Yale Center for Emotional Intelligence, our wellbeing and access to wellness are dependent on our ability to understand the sensations and signals throughout our body and then make a choice. This is important since you can’t make an embodied choice (step 2) before you have the data (step 1 - interoception). An example would be to imagine if you never felt the sensation of hunger, or the ‘hangry’ feeling when it’s been too long since the last boost of nourishment…how would you determine that you are hungry?
So, what to do? Many of us (clinicians and patients alike) live in a world full of overstimulation, productivity requirements, and constant stress. To develop interoception, finding little periods of stillness can be really useful. In yoga, there is a dedicated practice called pratyahara. Translated from Sanskrit to English as ‘withdrawal of the senses.’ The senses, in this case, includes all the sense organs: sight, smell, sound, touch, taste, movement (vestibular), and spatial placement (proprioception). Traditionally this is an aspect of meditation.
In my experience as a yoga teacher and physical therapist, I find this practice more accessible in the restorative yoga practice. It can take some graded exposure, but at the heart of the restorative yoga practice is stillness, darkness, silence, and support from props so that the body doesn’t have to do anything. These are also the essential components described by Herbert Benson, MD in his work on the Relaxation Response. In his work, he showed the relaxation response to be effective in decreasing heart and respiration rate triggering the benefits of the vagal nerve; which we are learning has so much to do with our ability to neuroregulate and participate in individual and communal stress management.
Restorative yoga is a practice of wakefully resting. Immordino-Yang et al, studied the brain in functional MRI when individuals were wakefully resting. The study found that during wakeful rest (without a meditative component where the brain has a task of concentration) the brain goes into a mode of neural processing called default mode. In default mode, the brain supports memory recall, imagining the future, and developing socio-emotional intelligence. In relationship to stress management, this is so important because it re-centers us, and allows for connection for even more neuroregulation.
For my patients, I often joke about lying on the floor. Really, it is not a joke at all. Lying on the floor for 15 minutes is savasana. Savasana is a wakeful resting and a practice of relaxation response. It seems easy: you always have access to a floor. You don’t need anything fancy. Aside from the neuroregulatory benefits of rest, savasana also gives the postural muscles a break. It allows the hip flexors to re-lengthen and the cervicothoracic junction to realign.
It is pretty great, and really accessible for most people. For those who are not comfortable flat, that’s where the props used in restorative yoga come into play. As physical and occupational therapists, we are so well primed to help people learn how to support their bodies in rest to get the benefits of rest.
Burnout, the Secret to unlocking the stress cycle by Emily Nagoski, Ph.D. and Amelia Nagoski, DMA
Polyvagal Theory, Stephen W Porges, PhD
Immordino-Yang et al. - Perspectives on Psychological Science - 2012
The Relaxation Response by Herbert Benson, MD, and Miriam Z Klipper

Portions of this blog are from an interview with Dustienne Miller. Dustienne is the creator of the two-day course Yoga for Pelvic Pain. She passionately believes in the integration of physical therapy and yoga in a holistic model of care, helping individuals navigate through pelvic pain and incontinence to live a healthy and pain-free life.
Have you noticed when you are afraid or don’t want to feel something you hold your breath? Imagine what it's like to have daily pain that limits function and how that could impact rib cage, abdominal and pelvic floor expansion. Dustienne Miller discusses this in her remote course, Yoga for Pelvic Pain, upcoming on July 31 - August 1, 2021. Her course focuses on two of the eight limbs of Patanjali’s eightfold path: pranayama (breathing) and asana (postures) and how they can be applied for patients who have hip, back, and pelvic pain.
Dustienne explains "We teach our patients how breathing patterns inform our digestion, our spine, our emotional state, our pelvic floor, etc. It’s one of the most powerful tools we have to inform our system that we are safe. Despite this knowledge, we will often find ourselves holding our breath or breathing in non-optimal ways without even realizing it." Dustienne focuses her practice on introducing yoga to patients within the medical model. Yoga can be included in pelvic rehabilitation in so many ways, including incorporating yoga home programs as therapeutic exercise and neuromuscular re-education (both between visits and after discharge).
Pelvic conditions that can be positively impacted by yoga are interstitial cystitis/painful bladder syndrome, vulvar pain, coccydynia, hip pain, and pudendal neuralgia. Treatment for these conditions often involves an individualized approach that may include both pharmacologic therapies (prescription drugs, analgesics, and NSAIDs) and nonpharmacologic interventions such as exercise, muscle strength training, cognitive behavioral therapy, movement/body awareness practices, massage, acupuncture, and nutrition.
A systematic review of the 2017 clinical practice guidelines evaluated 14 randomized controlled trials and found that yoga was associated with lower pain scores (1). Similarly, in 2020 there was a review of 25 randomized controlled trials that examined the effects of yoga on back pain. Out of these trials, 20 studies reported positive outcomes in pain, psychological distress, and energy (2).
The great thing about yoga is that the asanas (postures) can be modified to accommodate your strength, experience, and health conditions. An example of this is the Downward Facing Dog pose. There are so many ways to made Downward Facing Dog work for your body. Use straps, the wall, or the plinth/countertop to provide support for your body as needed, which might look different each day.
Some folks think you need to be flexible to have a yoga practice. Dustienne stresses "What is necessary is to be flexible with understanding that every day might feel different. If you are in an active pain flare your practice will look different than on the days you are feeling better. That can be a challenging aspect of a mindful practice - embracing that every day is different. Have the courage not to judge yourself, but to celebrate that you are meeting your needs with kindness."
People have been doing yoga for thousands of years. It is a mind-body and exercise practice that combines breath control, meditation, and movements to stretch and strengthen muscles. Join Dustienne Miller in Yoga for Pelvic Pain on July 31 - August 1, 2021, to learn more about incorporating yoga into your clinical practice.
No prior experience with teaching yoga is required to attend the course. However, all participants must possess a working knowledge of pelvic pain conditions and foundational rehabilitation principles.
- Chou R, Deyo R, Friedly J, et al. Nonpharmacologic therapies for low back pain: a systematic review for an American College of Physicians clinical practice guideline. Ann Intern Med. 2017; 166(7):493-505.
- Park J, Krause-Parello CA, Barnes CM. A narrative review of movement-based mind-body interventions: effects of yoga, tai chi, and qigong for back pain patients. Holist Nurs Pract. 2020;34(1):3-23.