At Herman & Wallace, we know that pelvic rehabilitation is a dynamic and ever-evolving field. While foundational courses like Pelvic Function Level 1 and Dry Needling and Pelvic Health often get the spotlight, there are several highly valuable courses that tend to fly under the radar. These courses offer practitioners the opportunity to deepen their knowledge, broaden their skills, and better serve patients with complex needs.
Here are five underrated courses that can have a powerful impact on your practice:
1. Nutrition Perspectives for the Pelvic Rehab Therapist
 Pelvic health doesn’t exist in isolation from the rest of the body, and nutrition plays a critical role in tissue healing, inflammation, digestion, and pelvic pain syndromes. This course introduces pelvic rehab practitioners to the fundamentals of nutrition as it relates to pelvic health.
Pelvic health doesn’t exist in isolation from the rest of the body, and nutrition plays a critical role in tissue healing, inflammation, digestion, and pelvic pain syndromes. This course introduces pelvic rehab practitioners to the fundamentals of nutrition as it relates to pelvic health.
Participants learn how to recognize when dietary factors may be contributing to issues such as constipation, bladder irritation, vulvar pain, or chronic inflammation. While not a course that trains clinicians to act as dietitians, it empowers them to screen for red flags, collaborate with nutrition professionals, and make basic, evidence-informed recommendations that can significantly impact patient outcomes.
2025 Course Date Options: October 11-12, December 6-7.
2. Oncology and the Pelvic Floor Series
 (OPF1: Foundations, OPF2A: Male Pelvic & Colorectal Cancers, and OPF2B: Female Pelvic & Bladder Cancers)
(OPF1: Foundations, OPF2A: Male Pelvic & Colorectal Cancers, and OPF2B: Female Pelvic & Bladder Cancers)
Pelvic health isn’t just for perinatal or orthopedic populations. People undergoing treatment for pelvic and abdominal cancers face unique and complex challenges, including incontinence, pelvic pain, sexual dysfunction, and scar tissue restrictions.
The Oncology and the Pelvic Floor series offers a comprehensive framework for working with patients at every stage of the cancer journey, and provides the knowledge and sensitivity needed to support this underserved population, integrating trauma-informed care, manual therapy, exercise, and interdisciplinary collaboration.
2025 Course Date Options: Level 1 September 13-14, Level 2A December 6-7, Level 2B November 1-2.
3. Pharmacologic Considerations for the Pelvic Health Provider
 Medications have a profound impact on the pelvic floor—often in ways that are overlooked. Whether it’s constipation from opioids, hormonal changes from contraceptives, or bladder irritation from certain antibiotics, understanding pharmacology is crucial.
Medications have a profound impact on the pelvic floor—often in ways that are overlooked. Whether it’s constipation from opioids, hormonal changes from contraceptives, or bladder irritation from certain antibiotics, understanding pharmacology is crucial.
This course demystifies medications commonly encountered in pelvic health practice. It helps clinicians understand how drugs can influence bowel, bladder, sexual function, pain processing, and healing. Armed with this knowledge, practitioners can engage in more informed discussions with patients and other members of the healthcare team, helping to troubleshoot barriers to progress.
2025 Course Date Option: September 13.
4. Yoga for Pelvic Pain
 Yoga is more than stretching—it’s a mind-body practice with proven benefits for nervous system regulation, pain management, and muscular balance. Yoga for Pelvic Pain teaches practitioners how to integrate evidence-based yoga principles into rehabilitation for patients with chronic pelvic pain.
Yoga is more than stretching—it’s a mind-body practice with proven benefits for nervous system regulation, pain management, and muscular balance. Yoga for Pelvic Pain teaches practitioners how to integrate evidence-based yoga principles into rehabilitation for patients with chronic pelvic pain.
This course goes beyond asana (physical postures) to incorporate breathwork, mindfulness, and gentle movement tailored to the needs of people with complex pain syndromes. Participants leave with practical tools they can immediately incorporate into one-on-one sessions or group classes, supporting both physical function and emotional well-being.
2025 Course Date Option: September 13-14.
5. Rehabilitative Ultrasound Imaging: Pelvic Health & Orthopedic Topics
 Rehabilitative Ultrasound Imaging (RUSI) provides real-time feedback for both clinicians and patients. It’s an invaluable tool for assessing muscle activation, motor control, and coordination - particularly for the deep core and pelvic floor muscles.
Rehabilitative Ultrasound Imaging (RUSI) provides real-time feedback for both clinicians and patients. It’s an invaluable tool for assessing muscle activation, motor control, and coordination - particularly for the deep core and pelvic floor muscles.
This course covers both pelvic health applications (like visualizing pelvic floor contractions) and broader orthopedic topics (like assessing the transverse abdominis or multifidus). Practitioners gain hands-on experience in using ultrasound to refine exercise prescription, improve patient engagement, and objectively document progress. Despite its transformative potential, RUSI remains underutilized in many pelvic rehab settings.
2025 Course Date Options for September 5-7: Self-hosted, Indianapolis IN, Seattle WA.
Don’t Overlook These Gems
Expanding your clinical toolbox with specialized knowledge can transform your patient care. Whether it’s understanding how nutrition, medications, cancer treatments, or mind-body practices influence the pelvic floor—or learning to harness the power of ultrasound imaging—these courses provide essential insights that go beyond the basics.
Ready to elevate your practice? Explore these courses and others at Herman & Wallace and continue your journey as a lifelong learner in pelvic rehabilitation.

Breast cancer is the second most common cancer in women, following skin cancers. In the United States, 1 in 8 women will develop breast cancer in their lifetime.
The treatments used in breast cancer also affect the pelvic floor.
Survivors report issues with pelvic floor dysfunction including incontinence, pelvic pain, sexual dysfunction, and constipation. Up to 58% of survivors report issues with bladder urgency and incontinence. (1) Around 52% of women report sexual dysfunction six months following post-breast cancer treatment, and 19-26% continue to have sexual dysfunction five to ten years after their diagnosis. (2) When compared to individuals without breast cancer, those with breast cancer presented with significantly weaker pelvic floor muscles when measured by maximal squeeze pressure and digital examination.
Additionally, the ability to relax the pelvic floor was poorer in participants with breast cancer compared to controls. (3) These are problems that pelvic rehabilitation practitioners can assist survivors with. However, not all survivors are being referred to therapy. Barriers to individuals accessing treatment for pelvic floor dysfunction include a lack of awareness about pelvic floor dysfunction following breast cancer treatments and health care professionals “not focusing on the management of pelvic floor symptoms during cancer treatment.” (4<)
We as rehabilitation clinicians should strive to correct this!
We can educate providers and patients regarding the potential to develop pelvic floor dysfunction with breast cancer treatment and how therapy can help.
Learn more about cancer treatment and pelvic-related complications in the Oncology of the Pelvic Floor Series. In the first course, you will learn about general oncology treatment, (certified lymphatic therapists can skip this course). The second course (Oncology of the Pelvic Floor Level 2A) in the series focuses on penile, testicular, and prostate cancer, along with colorectal cancers. The third course (Oncology of the Pelvic Floor Level 2B) in the series focuses on gynecological cancers and bladder cancer. In the series, you will learn about the medical treatment of cancer, how this affects the body, and how rehabilitation clinicians can help patients. Hands-on techniques are learned that can help patients return to activities they love. The first course in the series, Oncology of the Pelvic Floor Level 1, is being offered November 2-3. Join us to learn more about helping individuals with cancer!
Resources:
- Donovan KA, Boyington AR, Ismail-Khan R, Wyman JF. (2012) Urinary Symptoms in Breast Cancer: A Systematic Review. Cancer. 118(3): 582–593.
- Seav SM, Dominick SA, Stepahyuk B, Gorman JR, Chingos DT, Ehren JL, Krychman ML, Su HL. (2015). Management of sexual dysfunction in breast cancer survivors: a systematic review. Women's Midlife Health 1:9.
- Colombage UN, Soh SE, Lin KY, Frawley HC. (2023). Pelvic floor muscle function in women with and without breast cancer: a cross-sectional study. Continence. 5; 100580.
- Colombage UN, Lin KY, Soh SE, Brennen R, Frawley HC. (2022). Experiences of pelvic floor dysfunction and treatment in women with breast cancer: a qualitative study. Supportive Care in Cancer. 30; 8139-8149.
AUTHOR BIO:
Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC
 Allison Ariail has been a physical therapist since 1999. She graduated with a BS in physical therapy from the University of Florida and earned a Doctor of Physical Therapy from Boston University in 2007. Also in 2007, Dr. Ariail qualified as a Certified Lymphatic Therapist. She became board-certified by the Lymphology Association of North America in 2011 and board-certified in Biofeedback Pelvic Muscle Dysfunction by the Biofeedback Certification International Alliance in 2012. In 2014, Allison earned her board certification as a Pelvic Rehabilitation Practitioner. Allison specializes in the treatment of the pelvic ring and back using manual therapy and ultrasound imaging for instruction in a stabilization program. She also specializes in women’s and men’s health including conditions of chronic pelvic pain, bowel and bladder disorders, and coccyx pain. Lastly, Allison has a passion for helping oncology patients, particularly gynecological, urological, and head and neck cancer patients.
Allison Ariail has been a physical therapist since 1999. She graduated with a BS in physical therapy from the University of Florida and earned a Doctor of Physical Therapy from Boston University in 2007. Also in 2007, Dr. Ariail qualified as a Certified Lymphatic Therapist. She became board-certified by the Lymphology Association of North America in 2011 and board-certified in Biofeedback Pelvic Muscle Dysfunction by the Biofeedback Certification International Alliance in 2012. In 2014, Allison earned her board certification as a Pelvic Rehabilitation Practitioner. Allison specializes in the treatment of the pelvic ring and back using manual therapy and ultrasound imaging for instruction in a stabilization program. She also specializes in women’s and men’s health including conditions of chronic pelvic pain, bowel and bladder disorders, and coccyx pain. Lastly, Allison has a passion for helping oncology patients, particularly gynecological, urological, and head and neck cancer patients.
In 2009, Allison collaborated with the Primal Pictures team for the release of the Pelvic Floor Disorders program. Allison's publications include: “The Use of Transabdominal Ultrasound Imaging in Retraining the Pelvic-Floor Muscles of a Woman Postpartum.” Physical Therapy. Vol. 88, No. 10, October 2008, pp 1208-1217. (PMID: 18772276), “Beyond the Abstract” for Urotoday.com in October 2008, “Posters to Go” from APTA combined section meeting poster presentation in February 2009 and 2013. In 2016, Allison co-authored a chapter in “Healing in Urology: Clinical Guidebook to Herbal and Alternative Therapies.”
Allison works in the Denver metro area in her practice, Inspire Physical Therapy and Wellness, where she works in a more holistic setting than traditional therapy clinics. In addition to instructing Herman and Wallace on pelvic floor-related topics, Allison lectures nationally on lymphedema, cancer-related changes to the pelvic floor, and the sacroiliac joint. Allison serves as a consultant to medical companies, and physicians.

September is Ovarian Cancer Awareness Month. Ovarian cancer is the seventh most common type of malignant neoplasm in women and the eighth cause of mortality for women (Gaona-Luviano et al, 2020). In women who have died from gynecological cancers, ovarian cancer is the leading cause of death (Arora et al., 2021). This type of cancer can originate from any of the ovary's three main components, including the epithelium, stroma, and germinal cells. Per Gaona-Luviano et al., 2020, “epidemiology of this cancer shows differences between races and countries due to several factors including genetic and economic.” Detection of ovarian cancer is problematic because there is no standardized screening process and most cases of ovarian cancer are found in the advanced stages (Gaona-Luviano et al, 2020).
How is ovarian cancer diagnosed?
Sadly, the existing screening tests have a low predictive value. A gynecological evaluation, transvaginal ultrasound, and tumor marker testing (cancer antigen-125/CA-125 assay) can help with early detection strategies but this has not shown a significant effect on the morbidity or mortality of this cancer (Arora et al., 2021).
How is ovarian cancer treated medically?
Research shows that the standard line of care treatment includes surgery and platinum-based chemotherapy. Additional options including anti-angiogenic bevacizumab and Poly(ADP-ribose) polymerase (PARP) inhibitors have also been used more recently. (Arora et al., 2021)
What are the outcomes of an ovarian cancer diagnosis?
There is a high rate of recurrence after the initial detection treatment. Many of the cases re-occurred and these secondary cases were less curable with increased incidence of treatment failures (Arora et al., 2021).
What are ovarian cancer risk factors?
Some risk factors include advanced age, early menarche, late menopause, family history, nulliparity, obesity, perineal talc use, smoking, endometriosis, and hormone replacement therapy (Arora et al., 2021). Some protective factors include oral contraceptives, bilateral tubal ligation or salpingectomy, breastfeeding, and multiparity (Arora et al., 2021).
Some research shows there may be some health disparities in the diagnoses between Non-Hispanic Black women compared to Non-Hispanic White women. In a study by Washington et al. in 2023 53,367 women were included in the analysis with the profile being 82% Non-Hispanic White, 8.7% Non-Hispanic Black, 5.7% Hispanic, and 2.7% Non-Hispanic Asian/Pacific Islander. They found that the Non-Hispanic Black race was associated with a higher risk of death than Non-Hispanic White race and Non-Hispanic Black women versus Non-Hispanic White women had an increased risk of mortality among those with low and mid socioeconomic status groups.
In response to this potential inequity, the National Cancer Institute has launched 3 studies to look at these patterns to “better understand the causes of racial and ethnic disparities among women with ovarian cancer.” These studies will examine whether the treatments with these patient populations were consistent with standard clinical guidelines and ensure all patients received quality care. Additional studies will look at a “cells-to-society approach” to assess the biology behind these trends. In both cases, the researchers will assess a range of potential factors that can affect disparities, from the molecular makeup of tumors to environmental factors, and comorbidities (NCI, 2024).
What can pelvic health providers do to help?
As pelvic health providers, we can educate ourselves on how best to screen and refer our patients to ensure early diagnosis and medical treatment if we hear anything suspicious. It is difficult to self-advocate in this current medical climate and having a skilled provider guiding the questions to ask and the support to seek is invaluable. If a patient is already into their treatment journey, we can provide the needed rehabilitation support including things like coordination and strengthening of the core and pelvic floor, stretching and positioning to lengthen tight areas, scar mobilization, patient education, and symptom management with the patient for any symptoms that may pop up throughout their course of care.
If you’re unsure that you have these skills in your skill set, please check out the Oncology of the Pelvic Floor Series to gain more knowledge and experience in these areas to better help patients with these diagnoses. Certified Lymphatic Therapists may skip this course and move on to the level Oncology of the Pelvic Floor Level 2A and Level 2B courses.
- Oncology of the Pelvic Floor Level 1, next scheduled for November 2-3, 2024, is the first course in the series and focuses on topics that prepare practitioners to be part of the interdisciplinary oncology team. Topics will include the basics of cancer: terminology, staging, medical treatment, and the sequelae of these medical treatments. These topics include the lymphatic system as well as issues that are commonly seen in a patient who has been diagnosed with cancer such as cardiotoxicity, peripheral neuropathy, and radiation fibrosis.
- Oncology of the Pelvic Floor Level 2A, (not yet scheduled for 2025), builds on information presented in Oncology of the Pelvic Floor Level 1 and focuses on male pelvic cancers (prostate cancer, penile cancer, and testicular cancer), colorectal cancer, and anal cancer including risk factors, diagnosis, and prognosis. Topics discussed include sequelae of the medical treatment of cancer and how this can impact a patient’s body and quality of life, rehabilitation, and nutritional aspects focusing on these specific cancers, as well as home program options that patients can implement as an adjunct to therapy. Participants MUST register with a partner, or plan to have a volunteer available to work on during course labs.
- Oncology of the Pelvic Floor Level 2B, next scheduled for December 7-8, 2024, builds on information presented in Oncology of the Pelvic Floor Level 1 and focuses on gynecological and bladder cancers including risk factors, diagnosis, and prognosis. Topics discussed include sequelae of the medical treatment of cancer and how this can impact a patient’s body and quality of life, rehabilitation, and nutritional aspects focusing on these specific cancers, as well as home program options that patients can implement as an adjunct to therapy. Participants MUST register with a partner, or plan to have a volunteer available to work on during course labs.
References:
- Arora, T., Mullangi, S., & Lekkala, M. R. (2021). Ovarian cancer.
- Gaona-Luviano, P., Medina-Gaona, L. A., & Magaña-Pérez, K. (2020). Epidemiology of ovarian cancer. Chinese Clinical Oncology, 9(4), 47-47.
- NCI. Ovarian cancer studies aim to reduce racial disparities. Ovarian Cancer Studies Aim to Reduce Racial Disparities - NCI. (2024, June). https://www.cancer.gov/news-events/cancer-currents-blog/2020/ovarian-cancer-racial-disparities-studies#:~:text=Credit:%20iStock,impeded%20research%20in%20this%20area.
- Washington, C. J., Karanth, S. D., Wheeler, M., Aduse-Poku, L., Braithwaite, D., & Akinyemiju, T. F. (2024). Racial and socioeconomic disparities in survival among women with advanced-stage ovarian cancer who received systemic therapy. Cancer Causes & Control, 35(3), 487-496.
AUTHOR BIO:
Mora Pluchino, PT, DPT, PRPC

Mora Pluchino, PT, DPT, PRPC (she/her) is a graduate of Stockton University with a BS in Biology (2007) and a Doctorate of Physical Therapy (2009). She has experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. She began treating Pelvic Health patients in 2016 and now has experience treating women, men, and children with a variety of Pelvic Health dysfunction. There is not much she has not treated since beginning this journey and she is always happy to further her education to better help her patients meet their goals.
She strives to help all of her patients return to a quality of life and activity that they are happy with for the best bladder, bowel, and sexual functioning they are capable of at the present time. In 2020, She opened her own practice called Practically Perfect Physical Therapy Consulting to help meet the needs of more clients. She has been a guest lecturer for Rutgers University Blackwood Campus and Stockton University for their Pediatric and Pelvic Floor modules since 2016. She has also been a TA with Herman & Wallace since 2020 and has over 150 hours of lab instruction experience. Mora has also authored and instructs several courses for the Institute.

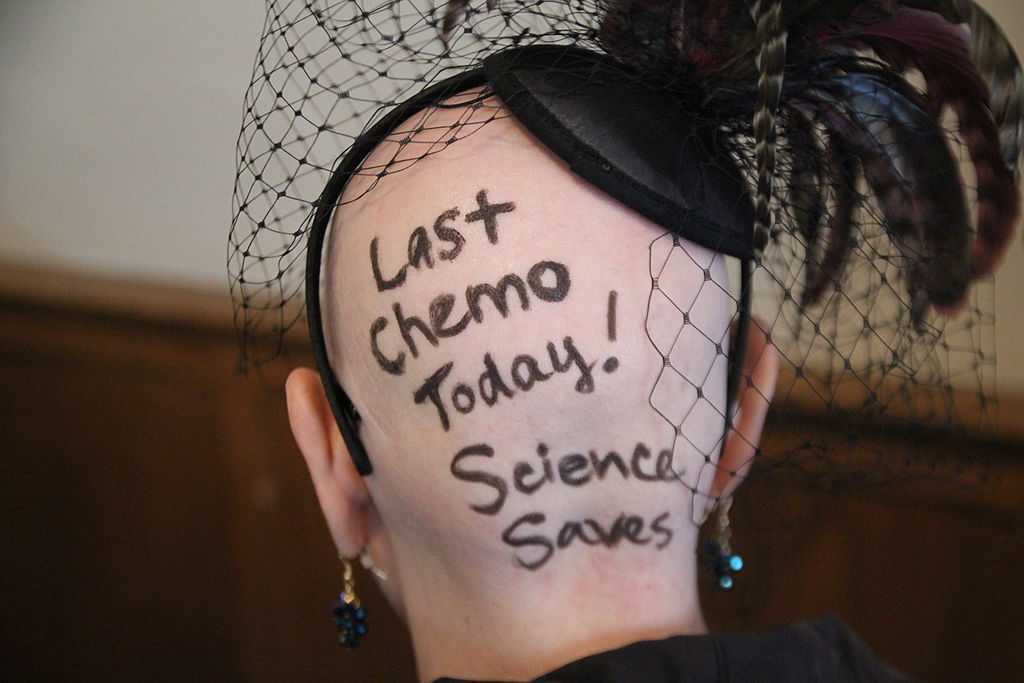
When I was diagnosed with Thyroid Cancer, I’ll be honest, one of my first thoughts was “Thank goodness this won’t directly affect my pelvic floor.” I think as someone who has experienced pelvic floor problems in the past and worked in the pelvic health field for many years, this is probably a somewhat normal reaction, but it wasn’t the standard from my parents and other loved ones. They wanted answers and information and because Thyroid cancer didn’t fall into my niche knowledge of pelvic health, I had to do some research.
Let’s start by saying that thyroid Cancer is the most pervasive endocrine cancer in the world (Bray, 2018). It is the sixth most common cancer in females in the United States (Siegel, 2019). Thyroid cancer incidence and outcomes depend on where the patient lives with Ethiopia and the Philippines having the highest death rates (Deng, 2020). There has been a rise in the diagnosis of thyroid cancer which studies attribute to access to health care, ultrasound, training of those doing the ultrasound, use of fine needle aspiration biopsy, and changes in monitoring and management guidelines (Megwalu & Moon, 2022). The five-year survival rate for people diagnosed with Thyroid Cancer is around 98.5% (Boucai et al. 2024). There are a few types of Thyroid Cancer and Papillary Thyroid Cancer accounts for 84% of all cases (Boucai et al. 2024). There are also follicular, medullary, and anaplastic forms making up the remaining cases (Boucai et al. 2024).
When I tell people I have Thyroid Cancer one of their first questions is “What were your symptoms, how did you know?!” The short answer is, I didn’t know. My cancer journey started when I found out I had a 3 cm nodule that had grown a “significant” amount since my last ultrasound. My endocrinologist said the growth was enough to warrant a fine needle aspiration biopsy. In reading about this diagnosis, it seems many cases of Thyroid Cancers are asymptomatic and detected during a routine physical examination or found incidentally with diagnostic imaging (Boucai et al. 2024).
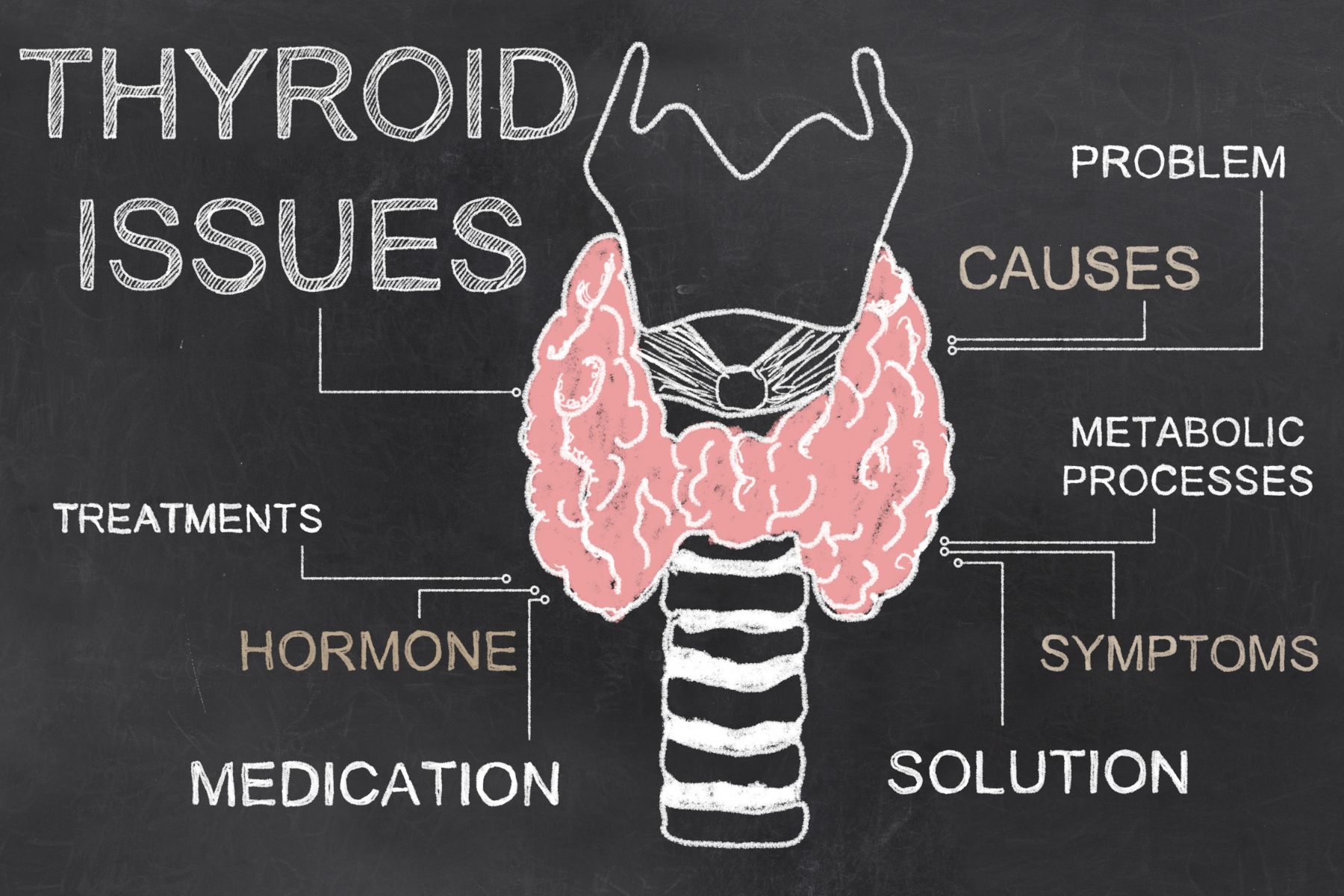 Some other symptoms, mostly related to a growing tumor could include lumps in the throat, a hoarse voice lasting three or more weeks, trouble swallowing or breathing, neck pain/pressure, and swollen cervical lymph nodes. If we had a patient with such complaints, referring them to their primary provider for further diagnostics would be very appropriate. Medullary thyroid cancer does have the ability to increase bowel movements and cause diarrhea and therefore should be on a pelvic health provider’s radar for differential diagnosis. The good news is that the solution to most cases of Thyroid Cancer is surgical removal of the thyroid with the option to perform radioactive iodine ablation treatment. There are other targeted therapies available if the cancer does not respond to radioactive iodine including antiangiogenic multikinase inhibitors and medications for specific genetic mutations (Boucai et al. 2024).
Some other symptoms, mostly related to a growing tumor could include lumps in the throat, a hoarse voice lasting three or more weeks, trouble swallowing or breathing, neck pain/pressure, and swollen cervical lymph nodes. If we had a patient with such complaints, referring them to their primary provider for further diagnostics would be very appropriate. Medullary thyroid cancer does have the ability to increase bowel movements and cause diarrhea and therefore should be on a pelvic health provider’s radar for differential diagnosis. The good news is that the solution to most cases of Thyroid Cancer is surgical removal of the thyroid with the option to perform radioactive iodine ablation treatment. There are other targeted therapies available if the cancer does not respond to radioactive iodine including antiangiogenic multikinase inhibitors and medications for specific genetic mutations (Boucai et al. 2024).
Let’s get to the good part, the therapeutic indications! How can we best support our patients going through Thyroid Cancer or after they have completed treatment?
There are a few things to consider and based on the setting you work on, you may or may not be the one to provide these services.
First, if the patient has a partial or total thyroidectomy, they will have a surgical incision which means a scar to work on and connective tissue restriction. We can help them to mobilize and soften this scar to maintain their cervical range of motion and help the scar to heal better, be less painful, and be more visually appealing. If the therapist has the training, education, and/or application of lymphatic drainage is also very valuable in this healing time.
The patient will have activity restrictions for 1 - 4 weeks depending on the severity of the procedure, including needing rest, eating soft foods, avoiding extremes of ROM of the neck and upper extremities, and regaining vocal control. Working with a patient prior to surgery to review ways to conserve energy and prepare themselves and their home for surgery can be invaluable, especially if the patient doesn’t have a huge support system available post-operatively. Food shopping, meal prepping, and convenience stations set up in the home can make post-operative recovery much smoother.
From personal experience, the throat irritation from the intubation was the most annoying and longest-lasting symptom. My surgeon used electrical stimulation with my intubation to my vocal cords to avoid damage to them. The mucous and hoarseness this created lasted a full 7 days. I still had voice limitations for about a month after and had to work to regain my full voice. Everyone handles pain differently though, and others may feel more pain. My provider, a very seasoned ENT, said they typically found post-thyroid patients had less discomfort than their patients with tonsillectomy or adenoid removal. This can give your patient a benchmark of what to expect if they’ve had one of those surgeries. We can give recommendations to our clients to help with pain management such as using rest, ice, gentle movement, breathing exercises, and meditation to help manage the discomfort, while also taking their pain medication regularly.
As a pelvic floor therapist, as soon as I hear pain medication is involved, I want to make sure that we are keeping the bowels happy. If we have a patient expecting this type of surgery and treatment, we can help guide them to fiber-filled foods and fluid intake to avoid constipation (as long as they don’t have restrictions). If constipation is not something they typically experience, this may be their first introduction to things like osmotic laxatives and a squatty potty and we can be the person who presents them with this education if they need it.
There will be a few things going on hormonally after the surgery. Because the thyroid has been removed, the patient will be hypothyroid unless they take synthetic thyroid hormone or have a partial thyroidectomy where the remaining half has continued to function and adjust. Hypothyroidism can cause many symptoms, but related to our patients in pelvic health, we might see constipation, fatigue, skin changes, menstrual cycle changes, musculoskeletal complaints, and intolerance to temperature changes. If we see our patient experiencing any of these, we can refer them back to their provider to have their levels checked. We can also tailor our plan of care to adjust for some of these things.
 Another more life-threatening complication that can happen is disruption of the parathyroid glands. These produce the calcium needed to regulate muscles and nerves. With calcium levels too low, a person can experience some uncomfortable and possibly dangerous symptoms such as feeling foggy and confused, muscle tremors, heart arrhythmias, and even seizures if the levels get too low. These little guys sit right under the thyroid and can be traumatized or accidentally removed with the thyroid. After surgery, patients will likely be taking a calcium supplement and have instructions to take it if they feel this way, but they may need a reminder from their very caring and observant therapist.
Another more life-threatening complication that can happen is disruption of the parathyroid glands. These produce the calcium needed to regulate muscles and nerves. With calcium levels too low, a person can experience some uncomfortable and possibly dangerous symptoms such as feeling foggy and confused, muscle tremors, heart arrhythmias, and even seizures if the levels get too low. These little guys sit right under the thyroid and can be traumatized or accidentally removed with the thyroid. After surgery, patients will likely be taking a calcium supplement and have instructions to take it if they feel this way, but they may need a reminder from their very caring and observant therapist.
When we think about how else Thyroid Cancer could affect our patients, I think it is important to consider the emotional aspect. Even though it’s a very common, easy-to-treat cancer with a high “cure rate,” it is still cancer. From personal experience, providers are so used to treating more sick people, that they have an almost blase attitude towards the treatment. I’ve spoken to others with endocrine cancer and heard similar stories. We have the “friendly” cancer, why stress or make haste about anything? There is a lack of haste or urgency, which can feel disconcerting when you just want to be cancer-free ASAP.
The incision, if surgery is needed, is directly to the anterior aspect of the neck. It's hard to hide the scar unless you wear a turtleneck. Most surgeons try to make the incision in a fold of the neck, but this may not be possible if lymph nodes also need to be dissected. Scars also take about a year to remodel and “silver.” We can further help our patients feel more confident with their scars by reminding them to avoid sunlight and utilize silicone patches to soften and protect the area to allow the scar to mature into a minimally noticeable line. There is still a reminder every time the patient looks in the mirror and this may affect all aspects of their life including their confidence in areas like sexual intimacy.
The last area to consider would be if a person needs the radioactive iodine treatment. Although this treatment is not “aggressive” like chemo or traditional targeted radiation, it can be a stressor to a patient. Radioactive iodine ablation has an extensive prep, multi-procedure application, and post-treatment quarantine phase that can be very disruptive to a person’s life. Pelvic health providers won’t be actively managing this phase, but being a friendly ear to bounce iodine-free recipe ideas off of and commiserate with the inability to ingest dairy for 3+ weeks can help make your patient feel supported and heard.
I have been fortunate enough to take Herman & Wallace’s Oncology series and so I felt prepared to treat and manage patients with these types of cancer. It was my own Thyroid Cancer journey that gave me hands-on experience with what it is like to be a cancer patient. It's been interesting to have to advocate in a medical system that doesn’t always listen to patients. I’ve also had to re-find who I am after having a pretty significant medical episode. These experiences always help give me perspective to be a better provider to my patients and bring more personalized care to them. I encourage you to take these classes, as cancer really affects so many lives. My most comforting providers during this time have been those who have taken the time to answer my questions, hold space for my worries, and have humor with me during this bizarre time.
The HW Oncology Series includes:
- Oncology of the Pelvic Floor Level 1 - Introduction (*Certified Lymphatic Therapists may skip this course)
- The next scheduled course is on November 2-3
- Oncology of the Pelvic Floor Level 2A - Male Pelvic and Colorectal Cancers
- The next scheduled course is on September 7-8
- Oncology of the Pelvic Floor Level 2B - Urogynecological Cancers
- The next scheduled course is on December 7-8
References:
- Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R. L., Torre, L. A., & Jemal, A. (2018). Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians, 68(6), 394-424.
- Boucai, L., Zafereo, M., & Cabanillas, M. E. (2024). Thyroid cancer: a review. Jama, 331(5), 425-435.
- Deng, Y., Li, H., Wang, M., Li, N., Tian, T., Wu, Y., ... & Dai, Z. (2020). Global burden of thyroid cancer from 1990 to 2017. JAMA network Open, 3(6), e208759-e208759.
- Megwalu, U. C., & Moon, P. K. (2022). Thyroid cancer incidence and mortality trends in the United States: 2000–2018. Thyroid, 32(5), 560-570.
- Siegel RL, Miller KD, Jemal A 2019 Cancer statistics, 2019. CA Cancer J Clin 66:7–30.
AUTHOR BIO:
Mora Pluchino, PT, DPT, PRPC

I am a graduate of Stockton University with my BS in Biology (2007) and Doctorate of Physical Therapy (2009). I have experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. I began treating Pelvic Health patients in 2016 and now have experience treating women, men, and children with a variety of Pelvic Health dysfunction. There is not much I have not treated since beginning this journey and I am always happy to further my education to better help my patients meet their goals.
I strive to help all of my patients return to a quality of life and activity that they are happy with for the best bladder, bowel, and sexual functioning they are capable of at the present time. In 2020, I opened my own practice called Practically Perfect Physical Therapy Consulting to help meet the needs of more clients. I have been a guest lecturer for Rutgers University Blackwood Campus and Stockton University for their Pediatric and Pelvic Floor modules since 2016. I have also been a TA with Herman & Wallace since 2020 and have over 150 hours of lab instruction experience.

Senior faculty member Allison Ariail, PT, DPT, CLT-LANA, BCB-PMD, PRPC sat down with the Pelvic Rehab Report to talk about the role pelvic therapists play on the oncology team that will work with the patient throughout treatment and into survivorship and the impact pelvic health has on quality of life for people with cancer.
Alison is part of the HW faculty team that wrote and instructs the Oncology course series, the next course is Oncology and the Pelvic Floor Level 1 on January 27-28, 2024.
Did you know that there are over 15 million cancer survivors in the United States? As advancements in care and early diagnosis improve, this is expected to increase to over 20 million survivors in the next 10 years. The continuum of care for patients with cancer ideally begins at diagnosis and the rehabilitation professional is an integral part of the oncology team that will work with the patient throughout treatment and into survivorship.
Pelvic cancers can include bladder cancer, cervical cancer, colorectal cancer, ovarian cancer, prostate cancer, and uterine cancer, among others. These patients can experience changes in how their body functions during or after cancer and its treatment. Changes caused by the treatment of cancer can lead to pain, discomfort, and problems with bowel, bladder, and sexual function
Why did you become a pelvic therapist?
I was attracted to pelvic therapy because I enjoy helping people who aren’t getting the help they need from other sources. When I first started working in pelvic floor therapy, there were not as many therapists working in the field. I absolutely loved it! I really enjoyed seeing the improvements patients made and the excitement that they had when they could come in and share with me that they saw improvements. They would share with me news about bowel, bladder, or sexual function that they would not even share with their partner. To see the happiness that people had with improvements in this intimate part of their lives really brought me joy. I enjoy helping people have hope in their lives and working with these patients is very rewarding to me.
What role does a rehab practitioner play on the oncology team?
Rehab professionals are key members of the oncology team. While the other members of the oncology team are focused on curing the cancer and helping the patient live longer, rehabilitation professionals focus on getting the patient to be able to do things in their lives that they enjoy. We are trained in working with the body and identifying dysfunction within the body that is limiting the patient and keeping them from functioning to their full potential. We have skills to address the musculoskeletal, visceral, nervous, and integumentary systems that can help improve the way a patient’s body is working and therefore improve function. Sometimes we address the little things with patients that then make the biggest impact in them living their lives. One patient of mine said that “her doctors saved her life, but her therapist helped her put her life back together so she could live it.” This quote really demonstrates the role a rehabilitation professional can have on an oncology patient.
What are some of the most important things you (and pelvic therapists) do for people with cancer in your role?
One of the most important things we therapists can do for our oncology patients is to listen. We spend a lot of time with our patients and develop a rapport with our patients. They then often share things with us they may not other providers. We have the skills to treat and help our patients with very personal symptoms in intimate areas. Pelvic floor therapists can help oncology patients return to a life that is more similar to their life before their cancer diagnosis. This is important. Their lives have been changed forever with their cancer diagnosis. If we can listen to the patient, and improve some of the symptoms they are experiencing; it can make a bigger difference than we think in helping them return to living their lives.
What are some common concerns oncology patients have, and how do you help address them?
One of the biggest issues oncology patients experience is restricted movement within the body. Surgery, and radiation both cause changes to the body that lead to scarring, fibrosis, and adhesions. This leads to a tightness that limits the normal movement of a body part, or decreased glide of the tissues. We address this a lot in the oncology series. We learn how to work with this restricted movement and help improve it. If the rehabilitation clinician can improve the ability of the body to move (whether it is a joint, a muscle, or the glide within the tissues), then this can ease pain, improve the function of that body part, and improve overall mobility and function for the patient.
What is the number one thing that practitioners should be aware of when it comes to pelvic therapy and cancer?
Radiated tissue is never the same as before it was radiated. Even if it has been years. Radiation changes the tissues. It can lead to inflammation, fibrosis, scarring, adhesions, texture change, and elasticity changes, among other effects. The effects of radiation can continue for years, and the tissues should be treated differently even if it has been many years since the patient underwent radiation. The therapist should learn to “listen” with their hand to see what state the tissues are in, and how to treat these tissues in a gentle and non-aggressive manner.
How can people with cancer better communicate with their pelvic therapists, and how can the practitioner facilitate these conversations?
I would encourage any cancer survivor to tell their therapist what is keeping them from doing what they love. When someone is diagnosed with cancer and goes through treatment, they often become limited in some of their activities. Unfortunately, many people don’t return to the activities that brought them joy. I would encourage patients to tell their therapist things that they wish they could do but cannot. Even if it is something little like making the bed, cooking a meal, or walking to the bathroom without leaking. Or if it is something bigger, like jumping on the trampoline with their kids, or returning to their exercise routine.
The therapist needs to know what it is that the patient would like to do but cannot do at this time. That way we can analyze the situation and figure out what can be done to help the patient reach their goal. I encourage therapists to ask their patients “What do you wish you could do but can’t now?”, or “What activities bring you joy?” If they are not able to do these activities after cancer treatment, work with the patient to see if you can help them return to that activity. It may be in baby steps, but that still can bring the patient joy!
What are some of the most rewarding parts of your job?
What I enjoy most about my job and working with oncology patients is the hope that I get to experience alongside these patients. I have the privilege of being able to work with these fighters and help them to gain function. The happiness they have when they can return to a loved activity, have an orgasm again, or be able to go to a movie without having fecal urgency is so very rewarding. I work with patients and try to instill an optimism that they can return to a better state. However, they also give me hope in life. Seeing their perseverance, their will to live, and their fight is inspirational! Working with oncology patients provides a positive light in my life; knowing that I am helping people that really need it, and the inspiration I get from working with these patients is amazing!
Join Oncology and the Pelvic Floor Level 1 on January 27-28, 2024 to learn more about working with oncology patients as part of an interdisciplinary oncology team to improve patient outcomes and quality of life.
Allison Ariail, PT, DPT, CLT-LAANA, BCB-PMD is one of the creators of the Herman & Wallace Oncology of the Pelvic Floor Course Series. Allison Ariail is a physical therapist who started working in oncology in 2007 when she became certified as a lymphatic therapist. She worked with breast cancer, lymphedema patients, head and neck cancer patients, and the overall oncology team to work with the whole patient to help them get better. When writing these courses, Allison was part of a knowledgeable team that included Amy Sides and Nicole Dugan among others.
As pelvic rehab professionals, we know the importance of the microbiome of the digestive tract and how this can influence issues our bowel patients may experience. You also may know that the GI microbiome can influence immune function as well as mental health. Did you know that the urinary bladder has its own microbiome? Recent developments in next-generation sequencing and bioinformatic platforms have allowed for the detection of microbial DNA in the urinary tract.(1) This could be a game changer for those who suffer from chronic urinary tract infections. However, it could be even more important as a way to prevent bladder cancer. May is Bladder Cancer Awareness Month. In honor of this month, let’s further discuss how the urinary microbiome may influence the development of bladder cancer.
Dysbiosis of the urinary microbiome could be related to bladder cancer through chronic inflammation in the urothelial microenvironment. Chronic inflammation is a hallmark of genomic instability and the development of cancer. A study in 2021 compared the urinary microbiome of patients with muscle-invasive and non-muscle-invasive bladder cancer. They found the microbial profiles differed in patients with cancer compared to healthy individuals. They also found that there were different microbial profiles from the less invasive non-muscle invasive versus the more invasive types of bladder cancer.(2)
The urinary microbiome is a growing area of research and I would expect to see more information come out on this, what influences the urinary microbiome, as well as how modulating this can prevent and fight urothelial cell carcinoma. I would anticipate more treatment options including some new immunotherapy agents to emerge that can help to fight bladder cancer.
If you do not know much about bladder cancer and would like to learn more, Oncology of the Pelvic Floor Level 2B covers topics on bladder cancer and gynecological cancers. Join us to learn more about these diagnoses, medical treatments, and ways a pelvic rehab professional can help these patients recover.
Resources:
1. Neugent ML, Hulyalkar NV, Nguyen VH, Zimmern PE, and De Nisco NJ. Advances in understanding the human urinary microbiome and its potential role in urinary tract infection. mBio. 2020; 11(2): e00218-20.
2. Hussein AA, Elsayed AS, Durrani M, et al. Investigating the association between the urinary microbiome and bladder cancer: an exploratory study. Urol Oncol. 2021; 39(6): 370.e9-370e19.

*Certified Lymphatic Therapists may skip Oncology of the Pelvic Floor Level 1 and move on to the Level 2A and Level 2B courses.*
Oncology of the Pelvic Floor Level 1 - no partner needed for registration
Price: $550.00 Experience Level: Beginner Contact Hours: 17.5 hours
Description: The course will address issues that are commonly seen in a patient who has been diagnosed with cancer such as cardiotoxicity, peripheral neuropathy, and radiation fibrosis. Some holistic medicine topics, including yoga and mindfulness, will be discussed in order to fully prepare the participant to be able to competently work with cancer survivors.
The basics of the lymphatic system will be covered, as well as when to refer the patient to a lymphatic specialist for further treatment. Red flags and warning symptoms will be discussed so the participant feels comfortable with knowing when to refer the patient back to their medical provider for further assessment.
This introductory course is aimed to get the participant comfortable with working with oncology patients and as part of an interdisciplinary oncology team.
Course Dates: July 8-9 and December 2-3
Oncology of the Pelvic Floor Level 2B - partner needed for registration
Price: $600.00 Experience Level: Intermediate Contact Hours: 19.25 hours
This course was designed to build on the information that was presented in Oncology of the Pelvic Floor Level 1.
Description: Information will be provided focusing on gynecological and bladder cancers including risk factors, diagnosis, and prognosis. The participant will also understand the sequelae of the medical treatment of cancer and how this can impact a patient’s body and quality of life. Other topics include rehabilitation and nutritional aspects focusing on these specific cancers, as well as home program options that patients can implement as an adjunct to therapy.
Course Dates: December 9-10
Allison Ariail, PT, DPT, CLT-LAANA, BCB-PMD is one of the creators of the Herman & Wallace Oncology of the Pelvic Floor Course Series. Allison Ariail is a physical therapist who started working in oncology in 2007 when she became certified as a lymphatic therapist. She worked with breast cancer, lymphedema patients, head and neck cancer patients, and the overall oncology team to work with the whole patient to help them get better. When writing these courses, Allison was part of a knowledgeable team that included Amy Sides and Nicole Dugan among others.
March is Colorectal Cancer Awareness Month. Did you know that the incidence rate of colorectal cancers is increasing? According to the International Agency for Research on Cancer, 1.9 million new cases of colorectal cancer were identified worldwide in 2020. This number is expected to grow even more. It is predicted that by 2040 the number of new cases of colorectal cancer will rise to 3.2 million new cases a year, and 1.6 million annual deaths worldwide. Additionally, did you know due to the fact that the incidence rate is increasing and it is being diagnosed in younger individuals, the age for screening for colorectal cancer has lowered to 45? At age 45 individuals should begin regular screening for colorectal cancer either via stool-based testing or visual-based screening via a colonoscopy. If someone has risk factors they may need to begin screening at a younger age.
Colorectal cancer can often be preventable through modifiable risk factors. Changing some of these risk factors, alongside the detection and removal of precancerous lesions can lower someone's risks. However, if a diagnosis is made, treatment can help to prolong the life of the patient. The treatment can include various surgeries, chemotherapy, and radiation. All of these treatments can cause changes to a patient's body. A rehab professional that has knowledge about both the body and how the medical treatment of cancer causes changes, can make all the difference in the world for that patient returning to activities that they enjoy and love after treatment.
There are not many opportunities for rehab professionals to learn about these changes and how we can help these patients. However, Herman & Wallace has a series focused on helping oncology patients. In this series, techniques are learned that can help colorectal cancer patients recover from their diagnosis and the medical treatment they go through. The oncology series is online and offered several times a year. You can attend the upcoming oncology courses on: Oncology of the Pelvic Floor Level 1 scheduled for July 8-9 and December 2-3, Level 2A scheduled for May 20--21, and Level 2B scheduled for December 9-10.
Reference:
Morgan E, Arnold M, Gini A, et al. Global burden of colorectal cancer in 2020 and 2040: incidence and mortality estimates from GLOBOCAN. Colon. 2023; 72(2).
*Certified Lymphatic Therapists may skip Oncology of the Pelvic Floor Level 1 and move on to the Level 2A and Level 2B courses.*
Oncology of the Pelvic Floor Level 1 - no partner needed for registration
Price: $550.00 Experience Level: Beginner Contact Hours: 17.5 hours
The basics of the lymphatic system will be covered, as well as when to refer the patient to a lymphatic specialist for further treatment. Red flags and warning symptoms will be discussed so the participant feels comfortable with knowing when to refer the patient back to their medical provider for further assessment.
This introductory course is aimed to get the participant comfortable with working with oncology patients and as part of an interdisciplinary oncology team.
Course Dates: July 8-9 and December 2-3
Oncology of the Pelvic Floor Level 2A - partner needed for registration
Price: $495.00 Experience Level: Intermediate Contact Hours: 17.25 hours
This course was designed to build on the information that was presented in Oncology of the Pelvic Floor Level 1.
Information will be provided focusing on male pelvic cancers, colorectal cancer, and anal cancer including risk factors, diagnosis, and prognosis. The participant will also understand the sequelae of the medical treatment of cancer and how this can impact a patient's body and quality of life. Other topics include rehabilitation and nutritional aspects focusing on these specific cancers, as well as home program options that patients can implement as an adjunct to therapy.
Course Dates: May 20--21
Oncology of the Pelvic Floor Level 2B - partner needed for registration
Price: $600.00 Experience Level: Intermediate Contact Hours: 19.25 hours
This course was designed to build on the information that was presented in Oncology of the Pelvic Floor Level 1.
Information will be provided focusing on gynecological and bladder cancers including risk factors, diagnosis, and prognosis. The participant will also understand the sequelae of the medical treatment of cancer and how this can impact a patient’s body and quality of life. Other topics include rehabilitation and nutritional aspects focusing on these specific cancers, as well as home program options that patients can implement as an adjunct to therapy.
Course Dates: December 9-10
In a 2018 article by Holly Tanner, she explains how managing a medical crisis such as a cancer diagnosis can be overwhelming for an individual. ‘Faced with choices about medical options, dealing with disruptions in work, home, and family life often leaves little energy left to consider sexual health and intimacy. Maintaining closeness, however, is often a goal within a partnership and can aid in sustaining a relationship through such a crisis.” Research shows that cancer treatment is disruptive to sexual health. Intimacy is a larger concept that may be fostered even when sexual activity is impaired or interrupted.
Prostate cancer treatment can change relational roles, finances, work-life, independence, and other factors including hormone levels. (1) Exhaustion (on the part of the patient and the caregiver), role changes, changes in libido, and performance anxiety can create further challenges. (1, 3, 4) Recovery of intimacy is possible, and reframing of sexual health may need to take place. Most importantly, these issues need to be talked about, as a renegotiation of intimacy may need to take place after a diagnosis or treatment of prostate cancer. (2)
If a patient brings up sexual health, or the practitioner encourages the conversation, many research-based suggestions can be provided to encourage recovery of intimacy including:
• Redefining sex to include other sexual practices beyond penetration, such as massage or touching, cuddling, talking, use of vibrators, medication, aids such as pumps (5)
• Participation in couples therapy to understand their partner’s needs, address loss, be educated about sexual function (7)
• Participation in “sensate focus” activities (developed by Masters & Johnson in the 1970s as “touch opportunities”) with appropriate guidance (6)
Holly continues to share that “Within the context of this information, there is an opportunity to refer the patient to a provider who specializes in sexual health and function. While some rehabilitation professionals are taking additional training to be able to provide a level of sexual health education and counseling, most pelvic health providers do not have the breadth and depth of training required to provide counseling techniques related to sexual health - we can, however, get the conversation started, which in the end may be most important.”
Courses of Interest:
- A colorectal or male pelvic cancer diagnosis has multiple systems that are affected by cancer treatment. The rehabilitation professional that works with the pelvic oncology patient needs to competently navigate treatment techniques for all of these systems, as well as be confident in treating a patient in a personal area. This two-day course will address specific cancer types including prostate cancer, penile cancer, and testicular cancer. Additional cancer types covered include colorectal cancer and anal cancer.
Trauma Awareness for the Pelvic Therapist - Remote Course - Apr 9-10, 2022
- Bring their increased awareness of trauma to the successful, holistic treatment of patients with pelvic pain, sexual dysfunction, bowel dysfunction, and bladder dysfunction.
Sexual Medicine in Pelvic Rehab - Remote Course - Apr 9-10, 2022
- This course provides a thorough introduction to pelvic floor sexual function, dysfunction and treatment interventions for males and females of all sexual orientations, as well as an evidence-based perspective on the value of physical therapy interventions for patients with chronic pelvic pain related to sexual conditions, disorders, and multiple approaches for the treatment of sexual dysfunction including understanding medical diagnosis and management.
Male Pelvic Floor Function, Dysfunction, and Treatment - Satellite Lab Course - April 23-24 2022
- Discuss sexual anatomy and physiology, prostate issues, and look at the research describing models of intimacy and what worked for couples who did learn to renegotiate intimacy after prostate cancer. Participants will be able to describe the relationships between pelvic muscle function and men’s sexual health, including the evidence that demonstrates pelvic muscle rehabilitation's positive impact on erectile function.
1. Beck, A. M., Robinson, J. W., & Carlson, L. E. (2009, April). Sexual intimacy in heterosexual couples after prostate cancer treatment: What we know and what we still need to learn. In Urologic oncology: seminars and original investigations (Vol. 27, No. 2, pp. 137-143). Elsevier.
2. Gilbert, E., Ussher, J. M., & Perz, J. (2010). Renegotiating sexuality and intimacy in the context of cancer: the experiences of carers. Archives of Sexual Behavior, 39(4), 998-1009.
3. Hawkins, Y., Ussher, J., Gilbert, E., Perz, J., Sandoval, M., & Sundquist, K. (2009). Changes in sexuality and intimacy after the diagnosis and treatment of cancer: the experience of partners in a sexual relationship with a person with cancer. Cancer Nursing, 32(4), 271-280.
4. Higano, C. S. (2012). Sexuality and intimacy after definitive treatment and subsequent androgen deprivation therapy for prostate cancer. Journal of Clinical Oncology, 30(30), 3720-3725.
5. Ussher, J. M., Perz, J., Gilbert, E., Wong, W. T., & Hobbs, K. (2013). Renegotiating sex and intimacy after cancer: resisting the coital imperative. Cancer Nursing, 36(6), 454-462.
6. Weiner, L., Avery-Clark, C. (2017). Sensate Focus in Sex Therapy: The Illustrated Manual. Routledge, New York.
7. Wittmann, D., Carolan, M., Given, B., Skolarus, T. A., An, L., Palapattu, G., & Montie, J. E. (2014). Exploring the role of the partner in couples’ sexual recovery after surgery for prostate cancer. Supportive Care in Cancer, 22(9), 2509-2515.
A recent article in the Washington Post Health & Science section explored the wonders of dietary fibre in an article called ‘Fiber has surprising anti-aging benefits, but most people don’t eat enough of it’ The article discussed how ‘…Fiber gets well-deserved credit for keeping the digestive system in good working order — but it does plenty more. In fact, it’s a major player in so many of your body’s systems that getting enough can actually help keep you youthful. Older people who ate fiber-rich diets were 80 percent more likely to live longer and stay healthier than those who didn’t, according to a recent study in the Journals of Gerontology’
But what is fiber and why does it matter?
Before we jump in there, let me answer the perennial questions that arise when we, as pelvic rehab clinicians, talk about fiber…’Is it in our scope of practice to talk about food?!’ I think it is fundamental that if we are placing ourselves as experts in bladder and bowel dysfunction, that we also remember that we can’t focus on problems at one end of ‘the tube’ without thinking about what happens at the other end. Furthermore, let me quote the APTA RC 12-15: The Role of the Physical Therapist in Diet and Nutrition. (June 2015): “as diet and nutrition are key components of primary, secondary, and tertiary prevention of many conditions managed by physical therapists, it is the role of the physical therapist to evaluate for and provide information on diet and nutritional issues to patient, clients, and the community within the scope of physical therapist practice. This includes appropriate referrals to nutrition and dietary medical professionals when the required advice and education lie outside the education level of the physical therapist’’
Fiber plays a huge role in so many of the health issues that we as clinicians face daily – constipation is regarded as a scourge of a modern sedentary society, perhaps over-reliant on processed convenience food – this is borne out when we gaze upon the rows of constipation remedies and laxatives in our pharmacies and supermarkets.
Let's take a look at the effects of fiber on breast cancer recovery – what does the research say?
There is growing interest and evidence to suggest that making different food choices can help control symptoms of breast cancer treatment and improve recovery markers – avoiding food with added sugar, hydrating well and focusing primarily on plant based food. Fiber is of course beneficial for bowel health, but may also have added benefits for heart health, managing insulin resistance, preventing excess weight gain and actually helping the body to excrete excess estrogen, which is often a driver for hormonally sensitive cancers. Fiber may be Insoluble (whole grains, vegetables) or Soluble (oats, rice, beans, fruit) but both are essential and variety is best.
In their paper ‘Diets and Hormonal levels in Post menopausal women with or without Breast Cancer’ Aubertin – Leheudre et al (2011) stated that ‘…Women eating a vegetarian diet may have lower breast cancer because of improved elimination of excess estrogen’, but even prior to that, in ‘Estrogen excretion patterns and plasma levels in vegetarian and omnivorous women.’ Golden et al (1982) concluded that ‘…that vegetarian women have an increased fecal output, which leads to increased fecal excretion of estrogen and a decreased plasma concentration of estrogen.’
Fiber may also be beneficial in the management of colorectal cancer, which is on the rise in younger women and men. A recent report by the World Cancer Research Fund International/American Institute for Cancer Research found that eating 90 grams of fiber-rich whole grains daily could lower colorectal cancer risk by 17 percent…and the side effects? A happier healthy digestive system, improved cardiovascular health and a lower risk of Type 2 Diabetes.
Your mother was right – eat your vegetables!
For more information on colorectal function and dysfunction, take Pelvic Floor Level 2A or for a deeper dive on the role of nutrition and pelvic health, why not take Megan Pribyl’s excellent course, Nutrition Perspectives for the Pelvic Rehab Therapist? Physical Therapy Treatment for the Breast Oncology Patient is also an excellent opportunity to learn about chemotherapy, radiation and pharmaceutical side effects of breast cancer treatment, as well as expected outcomes in order for the therapist to determine appropriate therapeutic parameters.
https://www.washingtonpost.com/national/health-science/fiber-has-surprising-anti-aging-benefits-but-most-people-dont-eat-enough-of-it/2018/04/27/c5ffd8c0-4706-11e8-827e-190efaf1f1ee_story.html?fbclid=IwAR0b-9VFUOCyUOgwe2BqV7-ahqwGzWs9rNpd1mscT75KNOGqnHm4ooFAu74&utm_term=.4d2784974ddc
Estrogen excretion patterns and plasma levels in vegetarian and omnivorous women. Goldin BR, Adlercreutz H, Gorbach SL, Warram JH, Dwyer JT, Swenson L, Woods MN. N Engl J Med. 1982 Dec 16;307(25):1542-7.
Diets and hormonal levels in postmenopausal women with or without breast cancer. Aubertin-Leheudre M1, Hämäläinen E, Adlercreutz H. Nutr Cancer. 2011;63(4):514-24. doi: 10.1080/01635581.2011.538487.
When a woman is given a cancer diagnosis, her entire world is turned upside down and inside out. There are so many things to think about; medical treatments, financial concerns, family concerns, and emotional upheaval. Sex may be the last thing that a woman may think about when she is actively going through treatment. However, at what rate are survivors having issues after treatment is complete?
 A recent study published in the journal Cancer looked at just this. A 2-year longitudinal study was performed that tracked young adults (18-39 years old) through and after their cancer diagnosis. The most common cancers seen in the samples were leukemia, breast cancer, soft-tissue sarcoma, and non-Hodgkin lymphoma. The patients completed the Medical Outcomes Study Sexual Functioning Scale at 4 months, 6 months, and 24 months after diagnosis. At 2 years after diagnosis over 50% of the patients surveyed reported some degree of sexual dysfunction. Women that were in a committed relationship had an increased likelihood for experiencing sexual dysfunction; while men had increased rate of reporting sexual issues regardless of their relationship status.
A recent study published in the journal Cancer looked at just this. A 2-year longitudinal study was performed that tracked young adults (18-39 years old) through and after their cancer diagnosis. The most common cancers seen in the samples were leukemia, breast cancer, soft-tissue sarcoma, and non-Hodgkin lymphoma. The patients completed the Medical Outcomes Study Sexual Functioning Scale at 4 months, 6 months, and 24 months after diagnosis. At 2 years after diagnosis over 50% of the patients surveyed reported some degree of sexual dysfunction. Women that were in a committed relationship had an increased likelihood for experiencing sexual dysfunction; while men had increased rate of reporting sexual issues regardless of their relationship status.
Women that undergo cancer treatment have several reasons that could be influencing their sexual function. Fatigue is a complaint that is often expressed by cancer patients. Their body image is often altered due to surgeries that have been performed. Chemotherapy and hormonal therapy often push women into menopause which then leads to vaginal dryness. Additionally, radiation and surgical treatment can lead to scar tissue, fibrosis, and stenosis of the vagina and pelvic floor muscles.
This is where physical therapy can help! In the Pelvic Floor Series Capstone course we teach advanced techniques that help treat pelvic floor issues by working on both the muscles, and the fascia. We also cover techniques that decrease the tenderness in the muscles that then allow you to stretch the muscle with less discomfort.
All of the techniques taught in Capstone are gentle but effective. The cancer survivor is the perfect population to use these gentle techniques on! Think of how rewarding our job will be when we help relieve the pain that may be associated with intercourse, and therefore improve intimacy of a cancer survivor with her partner!
Come join us for Capstone and learn techniques that will take your treatment skills to the next level!
Acquati, Zebrack, Faul, et al. Sexual functioning among young adult cancer patients: A 2-year longitudinal study. Cancer. 2018; 124(2): 398-405.