In the spring of 2019, myself and two lab assistants will have the privilege of teaching PF1 to Kenyan physical therapists through the Kenya Medical Training College (KMTC) in Nairobi, Kenya. The program at KMTC started six years ago by Washington DC-based physical therapist Richard Jackson, and The Jackson Clinics Foundation (Teachandtreat.org), with a focus on orthopedic manual therapy. A neuro rehab program ensued two years later, and the aim for this women’s health program is to build a three level course series similar to the way it is taught in the United States. The goal of all of these programs is to transition them to Kenyan faculty within six years, which has recently occurred in the orthopedic component. Herman & Wallace Pelvic Rehab Institute has graciously agreed to donate curriculum content to the women’s health course component.
 Teaching assistant Terri Lannigan, PT, DPT, OCS, who has taught the lumbopelvic girdle course in the orthopedic program, and also practices women’s health physical therapy in the US, began laying the groundwork for this program with her students and in the Nairobi community last December. “Not only is there a tremendous need, but there is a lot of excitement from a group of students currently taking courses in the program, that women’s health education is coming to KMTC!”
Teaching assistant Terri Lannigan, PT, DPT, OCS, who has taught the lumbopelvic girdle course in the orthopedic program, and also practices women’s health physical therapy in the US, began laying the groundwork for this program with her students and in the Nairobi community last December. “Not only is there a tremendous need, but there is a lot of excitement from a group of students currently taking courses in the program, that women’s health education is coming to KMTC!”
Over the past month, I have been editing the Pelvic Floor 1 course to tailor it to our Kenyan physical therapist audience. The overwhelming majority of Kenyan PT’s do not have access to biofeedback or electric stim, so those sections will be omitted. As there are no documentation or coding requirements in the Kenyan health system, those sections of curriculum will also be edited out. Many of Terri’s PT students complained of significant underemployment, so we will keep the marketing component in our lectures, in hopes to promote expansion of women’s health PT to a larger segment of the Kenyan population.
Meanwhile, teaching assistant Kathy Golic, PT of Overlake Hospital Medical Center’s Pelvic Health Program in Bellevue, WA has headed up the data collection for a lecture on managing fistula and obstetric trauma. Kathy has accumulated data from many sources and conferred with several PTs currently involved in both clinical education as well as direct patient care in multiple African nations, to help us to create relevant, meaningful and culturally appropriate curriculum for this section of the PF1 course.
Pelvic Floor Level 1 will be offered between March 25 – April 6, 2019 at Kenya Medical Training College. We will post photos and additional information of our class and our experiences. We are grateful to Herman and Wallace and The Jackson Clinics Foundation for allowing us to be involved in this exciting endeavor.
Going to the Combined Sections Meeting of the American Physical Therapy Association (CSM2019)? Look for Herman & Wallace instructor Carolyn McManus, MPT, MA at the educational session titled “Pain Talks: Conversations with Pain Science Leaders on the Future of the Field”. Carolyn will be a panelist along with Kathleen Sluka, PT, PhD, Steve George, PT, PhD, Carol Courtney, PT, PhD and Adriaan Louw, PT, PhD. The panel will be moderated by Derrick Sueki, DPT, PhD and Mark Shepherd, DPT, OCS.
 These influential leaders will share how they personally became interested in the field of pain and discuss innovative pain treatment, as well as leading edge pain research and its translation into clinical practice. Initiatives to standardize entry-level curriculum, develop pathways to pain specialization and create post-professional opportunities such as pain-specific residencies and fellowships will be explored. The session will conclude with the leaders discussing their views on the future of pain and the role of physical therapy in its management. The audience will be able to submit questions via text or email to the moderator for individual or panel discussion.
These influential leaders will share how they personally became interested in the field of pain and discuss innovative pain treatment, as well as leading edge pain research and its translation into clinical practice. Initiatives to standardize entry-level curriculum, develop pathways to pain specialization and create post-professional opportunities such as pain-specific residencies and fellowships will be explored. The session will conclude with the leaders discussing their views on the future of pain and the role of physical therapy in its management. The audience will be able to submit questions via text or email to the moderator for individual or panel discussion.
We are thrilled to have Carolyn on our faculty and excited that she has been offered this honor to contribute insights from her over 30-year career experience in the field of pain with her colleagues at CSM2019. Carolyn will offer her popular courses, Mindfulness for Rehabilitation Professionals at University Hospitals in Cleveland, OH on April 6 and 7, and Mindfulness-Based Pain Treatment in Portland, OR May 18 and 19, and Houston TX, October 26 and 27. We recommend these unique opportunities to train with a nationally recognized leader who pioneered the successful applications of mindfulness to the field of physical therapy. Hope to see you there!
"Over the next 30 years, growth in demand for services to care for female pelvic floor disorders will increase at twice the rate of growth of the same population. Demand for care for pelvic floor disorders comes from a wide age range of women… These findings have broad implications for those responsible for administering programs to care for women, allocating research funds in women’s health and geriatrics, and training physicians to meet this rapidly escalating demand"
- Karl M. Luber, MD, Sally Boero, MD, Jennifer Y. Choe, MD. The demographics of pelvic floor disorders: Current observations and future projections. Presented at the Sixty-seventh Annual Meeting of the Pacific Coast Obstetrical and Gynecological Society, Kamuela, Hawaii, November 14-19, 2000.
Patients with pelvic floor dysfunction have suffered for many years without knowing the names of their ailments. Chronic pain, constipation, incontinence, sexual dysfunction, and other pelvic conditions have a long history of being under-reported, misdiagnosed, and untreated. Shelby Hadden recounts in her animated documentary "Tightly Wound" being told by her doctor to treat vaginismus with a glass of wine before intimacy. She is not the only woman to be given such advice. It is going to take many voices to break through the years of misinformation and stigma that has impeded patients' ability to get treatment.
Thankfully the healthcare landscape has begun to shift. We seem to be on the cusp of a renaissance in pelvic care as patients become more aware of their treatment options. It is the mission of Herman & Wallace to help patients access a higher quality of care, through our courses and through our practitioner directory at https://pelvicrehab.com/. Patient education resources and practitioner directories are a big step in bringing about this awakening, and we believe that the more information the public has access to, the better. Ours is just one of several websites where patients can find learn about their conditions and find qualified clinicians to evaluate them and craft treatment regimens.
We hope that patients find pelvicrehab.com useful, and also encourage them to check out some other great resources. The Section on Women's Health operates a PT Locator available at https://ptl.womenshealthapta.org, and Pelvic Guru has been doing incredible work (see their robust patient portal at https://pelvicguru.com/for-patients/). Patients can also find helpful information via the International Pelvic Pain Society (IPPS) website at https://pelvicpain.org.
As an Institute, we've had the privilege of working with so many impassioned therapists, and we are excited to see so many of them out there in the world spreading awareness and knowledge so that patients get the care they need. We know there are many others working in the field and we hope you will tag and share your patient resources in the comments on this post.
Exciting news! Carolyn McManus, Herman & Wallace instructor of Mindfulness-Based Pain Treatment, will be a presenter in programming at the International Association for the Study of Pain (IASP) World Congress on Pain in to be held in Boston, September 11 - 16. This conference brings together experts from around the globe practicing in multiple disciplines to share new developments in pain research, treatment and education. Participants from over 130 countries are expected to attend. The last time it was held in the U.S. was 2002, so it presents an especially exciting opportunity for those interested in pain to have this international program taking place in the U.S. Carolyn will present a workshop on mindfulness in a Satellite Symposia, Pain, Mind and Movement: Applying Science to the Clinic.
 Carolyn has been a leader in bringing mindfulness into healthcare throughout her over-30 year career. She recognized early on in her practice how stress amplified patients’ symptoms and, as she had seen the benefits of mindfulness in her own life, it was a natural progression to integrate mindful principles and practices into her patient care. An instructor for Herman and Wallace since 2014, she has developed two popular courses, Mindfulness-Based Pain Treatment and Mindfulness for Rehabilitation Professionals, enabling her to share her clinical and research experiences with her colleagues.
Carolyn has been a leader in bringing mindfulness into healthcare throughout her over-30 year career. She recognized early on in her practice how stress amplified patients’ symptoms and, as she had seen the benefits of mindfulness in her own life, it was a natural progression to integrate mindful principles and practices into her patient care. An instructor for Herman and Wallace since 2014, she has developed two popular courses, Mindfulness-Based Pain Treatment and Mindfulness for Rehabilitation Professionals, enabling her to share her clinical and research experiences with her colleagues.
For many patients, pain is not linearly related to tissue damage and interventions based on structural impairment alone are inadequate to provide full symptom relief. Mindfulness training can offer a key ingredient necessary for a patient to make additional progress in treatment. By learning therapeutic strategies to build body awareness and calm an over-active sympathetic nervous system, patients can mitigate or prevent stress-induced symptom escalation. They can learn to move with trust and confidence rather than fear and hesitation.
A growing body of research in mindfulness-based therapies demonstrates multiples benefits for patients suffering with pain conditions. Research suggests that mindfulness training can be helpful to women preparing for childbirth and patients suffering from fibromyalgia, pelvic pain, IBS and low back pain. In addition, for patients with anxiety, mindfulness training may contribute to reductions in anxiety and in adrenocorticopropic hormone and proinflammatory cytokine release in response to stress. Authors of this study conclude that these large reductions in stress biomarkers provide evidence that mindfulness training may enhance resilience to stress in patients with anxiety disorders.
In addition to her presentation at the IASP World Congress Satellite Symposia, Carolyn will be sharing a more in-depth examination and practice of mindfulness in her upcoming course Mindfulness-Based Pain Treatment, August 4 and 5 at Virginia Hospital Center, Arlington VA, and again November 3 and 4 at Pacific Medical Center in Seattle, WA. Please join an internationally-recognized expert for 2 days of innovative training in mindfulness that will both improve your patient outcomes and enhance your own well-being!
Duncan LG, Cohn MA, Chao MT, et al. Benefits of preparing for childbirth with mindfulness training: A randomized controlled trial. BMC Pregnancy Childbirth 2017 May 12;17(1):140.
Fox SD, Flynn E, Allen RH. Mindfulness meditation for women with chronic pelvic pain: a pilot study. J Reprod Med.2011;56(3-4):158-62.
Garland EL, Gaylord SA, Paisson O. Therapeutic mechanisms of a mindfulness-based treatment for IBS: effects on visceral sensitivity, catastrophizing and affective processing of pain sensations. J Behav Med. 2012;35(6):591-602.
Cherkin DC, Sherman KJ, Balderson BH, et al. Effect of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: a randomized Clinical Trial. JAMA. 2016;315(12):1240-9.
Hoge EA, Bui E, Palitz SA, et al. The effect of mindfulness meditation training on biological acute stress responses in generalized anxiety disorder. Psychiatry Res. 2018;262:328-332.

In patients who failed to respond to biofeedback therapy alone for anismus, authors in this study reported a beneficial, although temporary, effect of using botulinum toxin type A injection (BTX-A injection) to the puborectalis and external sphincter muscles. Anismus is more commonly referred to as dyssynergic defecation, or an inability to properly lengthen the pelvic floor muscles during emptying of the bowels. 31 patients who had been treated with and failed "simple biofeedback training" were then treated with BTX-A injection followed by biofeedback training. 18 males and 13 females with a mean age of 50 and a mean duration of constipation of 5.6 years were diagnosed with defecation dysfunction, or anismus. Diagnosis of animus was made using anorectal manometry, balloon expulsion test, surface electromyography (EMG) of the pelvic floor, and defecography.
Pelvic floor muscle training included biofeedback therapy consisting of intra-anal surface EMG and electrotherapy (although the way the methods are described make determining if both EMG and electrotherapy were completed with internal sensors difficult). Treatment occurred 1-2 times/day for 30 minutes per session (15 minutes of electrotherapy and 15 minutes of biofeedback). Frequency of the electrotherapy was 10 Mz, 10 seconds of "considerable sensation without…pain" and 10 seconds of rest. During biofeedback sessions, pelvic muscle strengthening and relaxation was also instructed. Therapy occurred for up to one month, and patients were instructed to continue with therapeutic exercises at home. The researchers followed up one month after the injection and therapy, and 6-12 months after intervention by telephone.
The subjects in this study suffered from difficult and incomplete evacuation, use of laxatives, and chronic straining during defecation. The repeated measures for diagnostic criteria that were completed after intervention found improvements in the subjects' resting anal canal pressures and with the balloon expulsion test and constipation scoring system. The authors also reported adverse effects of BTX-A injections including fecal incontinence. Conclusions of the article include that the botox injections were considered a temporary treatment for defecation dysfunction, whereas the botox injection combined with pelvic floor biofeedback training is "a more valid way to treat."
What is missing from this study? Manual therapy, muscle coordination retraining in combination with abdominal wall activation, and functional training related to positioning. While the authors suggest that injections should be used with biofeedback training, the potential negative effects of botox injections cannot be overlooked. Infection, pain, and bleeding are complications that have been highlighted in the literature, and in this study, fecal incontinence (although reported as mild) occurred. The research design appears to fail to recognize the chronic tension and holding pattern of the pelvic floor muscles, and unless the goal of repeated contractions is to elicit a contract/relax effect, the pelvic floor strengthening per se does not align with the ideal therapeutic goal, which should be to correct the dyssynergic pattern of defecation. Relaxing the pelvic floor muscles is not the same as a functional bearing down or lengthening of the pelvic floor involved in defecation. If you are interested in learning more about training defecation patterns and pelvic muscle rehabilitation for bowel dysfunction, check out Pelvic Floor Level 2A (PF2A) which discusses in detail fecal incontinence, constipation, and other colorectal conditions. The next opportunity to take this course is in Wisconsin in March. If you have already taken PF2A, you might find a course focused on Bowel Pathology, Function, Dysfunction & the Pelvic Floor, with the next course taking place in Kansas City in April.
Jason Hardage is a physical therapist who practices in Alameda, CA. He recently attended the Mindfulness-Based Pain Treatment course which is written and instructed by faculty member Carolyn McManus, PT, MS, MA. Dr. Hardage was kind enough to send in the following review in order to help spread the good word about this powerful course. Your next opportunity to learn how to apply mindfulness practices in your clinic will be in Boston, MA on March 4-5, 2017.
Carolyn McManus' 2-day course, Mindfulness-Based Pain Treatment, was truly outstanding. In my opinion, the integration of mindfulness into healthcare is a paradigm shift and in that sense Carolyn is a visionary who is ahead of her time, as she has been practicing in this arena for many years. Her expertise is clear (as is her joy in teaching).
 In this course, she introduces the basic terminology, concepts, and mindfulness practices in a way that is experiential, practical, and accessible, with many tools and techniques to integrate into clinical practice. She thoroughly reviews the evidence in a way that is skillful and compelling and provides the theory as to how mindfulness works, then provides case studies from her own clinical practice. She also provides a brief survey of other tools and approaches that are complementary, such as yoga, loving kindness meditation, and motivational interviewing, then shows how to put it all together, including suggestions for documentation and billing. She is generous in sharing resources, including patient education materials and four open-access guided relaxation and meditation sessions from her Web site, as well as resources for continued study. Furthermore, she presents ways for the healthcare practitioner to use mindfulness for self care, to help combat the burnout that can come with serving those with complex needs in a demanding healthcare environment.
In this course, she introduces the basic terminology, concepts, and mindfulness practices in a way that is experiential, practical, and accessible, with many tools and techniques to integrate into clinical practice. She thoroughly reviews the evidence in a way that is skillful and compelling and provides the theory as to how mindfulness works, then provides case studies from her own clinical practice. She also provides a brief survey of other tools and approaches that are complementary, such as yoga, loving kindness meditation, and motivational interviewing, then shows how to put it all together, including suggestions for documentation and billing. She is generous in sharing resources, including patient education materials and four open-access guided relaxation and meditation sessions from her Web site, as well as resources for continued study. Furthermore, she presents ways for the healthcare practitioner to use mindfulness for self care, to help combat the burnout that can come with serving those with complex needs in a demanding healthcare environment.
This is certainly one of the best courses that I've taken in over 17 years as a physical therapist. While it's easy to see how the content of the course is applicable to people with chronic pain, in my opinion, this approach is broadly applicable across patient populations. It's exciting to know that we have a physical therapist who is an expert, long-time practitioner and teacher of mindfulness from whom to learn. I highly recommend this course! At the same time, it left me wanting more and I'd love to see Carolyn develop other ways to deliver content--such as a blog and online video content--that would allow her to connect with a wider audience and also to stay connected to those who have taken her course.**
Sincerely,
Jason Hardage, PT, DPT, DScPT, GCS, NCS
Alameda, CA
Editor's note: Since publication of this review, Carolyn has began to publish a blog on mindfulness! See more at The Mindfulness in Healthcare Blog
Herman & Wallace are pleased to announce a new course! Pudendal Neuralgia and Nerve Entrapment will be presented by Michelle Lyons in Freehold, NJ on June 17/18, 2017. We chatted with Michelle about this new course to hear her thoughts and get an overview of the contents
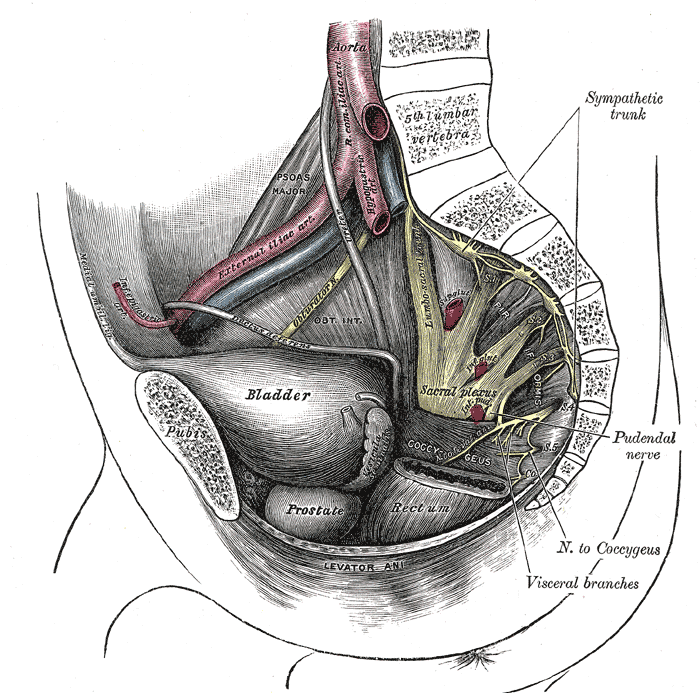 There are a number of courses which I teach for Herman & Wallace including Pelvic Floor Level 2A, my Male Oncology and Female Oncology and the The Athlete and the Pelvic Floor courses. They all have sections on pudendal dysfunction and it’s an area that participants always want more information on. There’s no other nerve that elicits the same interest, discussion and confusion! Nobody really talks about iliohypogastric or ulnar neuralgia with the same intensity as pudendal neuralgia, and no other nerve dysfunction provokes the same amount of controversy and mystery.
There are a number of courses which I teach for Herman & Wallace including Pelvic Floor Level 2A, my Male Oncology and Female Oncology and the The Athlete and the Pelvic Floor courses. They all have sections on pudendal dysfunction and it’s an area that participants always want more information on. There’s no other nerve that elicits the same interest, discussion and confusion! Nobody really talks about iliohypogastric or ulnar neuralgia with the same intensity as pudendal neuralgia, and no other nerve dysfunction provokes the same amount of controversy and mystery.
When I was approached about developing this course for the Institute, I jumped at the opportunity. For those who don’t know me, I really like to bring an integrative approach to my work, both clinically and educationally. I have experience and training in nutrition, coaching, yoga, Pilates and mindfulness as a therapeutic intervention and I think these fit really well alongside traditional pelvic rehab approaches. Manual therapy and bespoke exercise prescription will always be the bedrock of my approach, but sometimes our patients, especially those with chronic pain, need some extra support. I’m also a bit of an anatomy nerd, so the chance to delve deep into pelvic neuroanatomy and neurodynamics was too much to resist!
I think this is a Golden Age in pelvic health – there are so many great learning opportunities and resources available to us to help serve our patients better. Another area that I find fascinating to explore is the huge leap we have made in understanding neuroscience and the role of pain education when it comes to chronic pelvic pain. I’m a big fan of the work done by Moseley and Butler in Australia, and I love how authors like Hilton, Vandyken and Louw have transferred that to the world of pelvic pain in their book "Why Pelvic Pain Hurts". The language that we use is very important when discussing how the brain responds to chronic pain and the changes that occur with central sensitization. We never want our patients to feel as if we think their pain is ‘all in their heads’ but at the same time, we need to be able to incorporate strategies such as motor imagery and graded exposure and to demonstrate to our patients that"…it is important to acknowledge that chronic pain need not involve any structural pathology" (Aronoff 2016).
Those are some of the discussions we’ll be having in Freehold, NJ next June – I hope you’ll come and join the conversation!
"What Do We Know About the Pathophysiology of Chronic Pain? Implications for Treatment Considerations" Aronoff, GM Med Clin North Am. 2016 Jan;100(1):31-42
"Why Pelvic Pain Hurts: Neuroscience Education for Patients with Pelvic Pain" Hilton, Vandyken, Louw, International Spine and Pain Institute (May 28, 2014)
When I bring up the topic of pelvic floor dysfunction in athletes, stress urinary incontinence (SUI) is usually the first aspect of pelvic health that springs to mind – and rightly so, as professional sport is one of the risk factors for stress urinary incontinence Poswiata et al 2014. The majority of studies show that the average prevalence of urinary incontinence across all sports is 50%, with SUI being the most common lower urinary tract symptom. Athletes are constantly subject to repeated sudden & considerable rises in intra-abdominal pressure: e.g. heel striking, jumping, landing, dismounting and racquet loading.
What’s less often discussed is the topic of gastrointestinal dysfunction in athletes. Anal incontinence in athletes is not well documented, although a study from Vitton et al in 2011 found a higher prevalence than in age matched controls (conversely a study by Bo & Braekken in 2007 found no incidence). More recently, Nygaard reported earlier this year (2016) that young women participating in high-intensity activity are more likely to report anal incontinence than less active women.
A presentation by Colleen Fitzgerald, MD at the American Urogynecologic Society meeting in 2014 highlighted the multifaceted nature of pelvic floor dysfunction in female athletes, specifically in this case, triathletes. The study found that one in three female triathletes suffers from a pelvic floor disorder such as urinary incontinence, bowel incontinence and pelvic organ prolapse. One in four had one component of the "female athlete triad", a condition characterized by decreased energy, menstrual irregularities and abnormal bone density from excessive exercise and inadequate nutrition. Researchers surveyed 311 women for this study with a median age range of 35 – 44. These women were involved with triathlete groups and most (82 percent) were training for a triathlon at the time of the survey. On average, survey participants ran 3.7 days a week, biked 2.9 days a week and swam 2.4 days a week.
Of those who reported pelvic floor disorder symptoms, 16% had urgency urinary incontinence, 37.4% had stress urinary incontinence, 28% had bowel incontinence and 5% had pelvic organ prolapse. Training mileage and intensity were not associated with pelvic floor disorder symptoms. 22% of those surveyed screened positive for disordered eating, 24% had menstrual irregularities and 29% demonstrated abnormal bone strength. With direct access becoming a reality for many of us, we must acknowledge the need for specific questioning when it comes to pelvic health issues, as well as the ability to recognise signs and symptoms of the female athlete triad in our patients.
Want to learn more about pelvic health for athletes? Join me in beautiful Arlington this November 5-6 at The Athlete and the Pelvic Floor!
J Hum Kinet. 2014 Dec 9; 44: 91–96 Published online 2014 Dec 30. doi:10.2478/hukin-2014-0114 PMCID: PMC4327384. Prevalence of Stress Urinary Incontinence in Elite Female Endurance Athlete Anna Poświata, Teresa Socha and Józef Opara1
J Womens Health (Larchmt). 2011 May;20(5):757-63. doi: 10.1089/jwh.2010.2454. Epub 2011 Apr 18. Impact of high-level sport practice on anal incontinence in a healthy young female population. Vitton V, Baumstarck-Barrau K, Brardjanian S, Caballe I, Bouvier M, Grimaud JC.
Am J Obstet Gynecol. 2016 Feb;214(2):164-71. doi: 10.1016/j.ajog.2015.08.067. Epub 2015 Sep 6. Physical activity and the pelvic floor. Nygaard IE, Shaw JM.
Our understanding of treating pelvic pain keeps growing as a profession. We have so many manual therapies such as visceral manipulation, strain counter strain, and positional release adding dimension to our treatment strategies for shortened and painful tissues. Pharmacologic interventions such as botox, valium, and antidepressants are becoming more popular and researched in the literature. We are beginning to work more collaboratively with vulvar dermatologists, urogynecologists, OB’s, family practitioners, urologists, and pain specialists.
 Pelvic rehab providers are in a unique position of being able to offer more time with each patient and to see our patients for several visits. Frequently we are the ones being told stories about how a particular condition is really affecting our patient’s life and the emotional struggles around that. We are often the one who gets a clear picture of our patient’s emotional and mental disposition. A rehab provider may realize that a patient seems to exhibit mental patterns in their treatment. It can be anxiety from how the condition is changing their life, difficulty relaxing into a treatment, poor or shallow breathing patterns, frequently telling themselves they will never get better, or being able to perceive their body only as a source of pain or suffering, losing the subtlety of the other sensations within the body. Yet, aside from contacting a physician, who may offer a medication with side effects, or referring to a counselor or psychologist, our options and training may be limited. Patients may be resistant to seeing a mental health counselor, and we have to be careful to stay in our scope.
Pelvic rehab providers are in a unique position of being able to offer more time with each patient and to see our patients for several visits. Frequently we are the ones being told stories about how a particular condition is really affecting our patient’s life and the emotional struggles around that. We are often the one who gets a clear picture of our patient’s emotional and mental disposition. A rehab provider may realize that a patient seems to exhibit mental patterns in their treatment. It can be anxiety from how the condition is changing their life, difficulty relaxing into a treatment, poor or shallow breathing patterns, frequently telling themselves they will never get better, or being able to perceive their body only as a source of pain or suffering, losing the subtlety of the other sensations within the body. Yet, aside from contacting a physician, who may offer a medication with side effects, or referring to a counselor or psychologist, our options and training may be limited. Patients may be resistant to seeing a mental health counselor, and we have to be careful to stay in our scope.
Research is showing us that meditation as an intervention can be very helpful in addressing these chronic pain issues.
In a study in the Journal of Reproductive Medicine, 22 women with chronic pelvic pain were enrolled in an 8 week mindfulness meditation course. Twelve out of 22 enrolled subjects completed the program and had significant improvement in daily maximum pain scores, physical function, mental health, and social function. The mindfulness scores improved significantly in all measures (p < 0.01).
The questions have arisen, if meditation alters opiod pathways, how can it be administered safely with prescription medications. However in a 2016 study in the journal of neuroscience, it was concluded that meditation-based pain relief does not require endogenous opioids.” Therefore, the treatment of chronic pain may be more effective with meditation due to a lack of cross-tolerance with opiate-based medications.” “The risks of chronic therapy are significant and may outweigh any potential benefits”, according the the journal of American Family Medicine. Meditation training can be a tool to help our patients manage their pain without risk of long term opiod use.
In the two day course, Meditation for Patients and Providers, participants will learn several different meditation and mindfulness techniques they can use for patients with different dispositions, and to tailor the most appropriate approach to specific patients. The aim of the course is to be able to work meditation into a treatment and a home program that is best suited for your patient. The course also covers self care, preventing provider burn out and ways to be more mentally quiet as a provider seeking to give optimal care with appropriate boundaries.
Fox, S. D., Flynn, E., & Allen, R. H. (2010). Mindfulness meditation for women with chronic pelvic pain: a pilot study. The Journal of reproductive medicine, 56(3-4), 158-162.
LEMBKE, A., HUMPHREYS, K., & NEWMARK, J. (2016). Weighing the Risks and Benefits of Chronic Opioid Therapy. American Family Physician,93(12).
Zeidan, F., Adler-Neal, A. L., Wells, R. E., Stagnaro, E., May, L. M., Eisenach, J. C., ... & Coghill, R. C. (2016). Mindfulness-Meditation-Based Pain Relief Is Not Mediated by Endogenous Opioids. The Journal of Neuroscience, 36(11), 3391-3397.
More than a year ago, after working on updating the pelvic floor series courses PF1, 2A and 2B, the Institute turned our attention to the final course in our popular series, PF3. To determine what content our participants wanted to learn about in the last continuing education course of the series, we asked that exact question. From a large survey of therapists who had taken all or most of the courses in the pelvic core series, we collected detailed data from therapists about what was needed to round out their comprehensive training. The results of that survey guided hundreds (and hundreds!) of hours of work completed by a team of instructors. This month, in the beautiful city of Denver, the three instructors who created the Capstone course will share their wisdom, clinical experiences, as well as their thoughtfully-designed lectures and labs. You will have an opportunity to learn in depth about topics covered in the prior courses in the series.
Such topics include lifespan issues and health issues common to different ages, conditions of polycystic ovarian syndrome, endometriosis, infertility, pelvic organ prolapse and surgeries, pelvic fascial anatomy, pharmacology and nutrition. Lab components are detailed and comprehensive for working with specific common implications from conditions in pelvic dysfunction or surgery. This course focuses on the female pelvis, including diving into the complexities of female pelvic health issues. The instructors have all worked in the field for many years, are experienced in working with complex patient presentations, and all excel at manual therapies. I asked each of them to briefly share thoughts about the Capstone course that they each dedicated the last year in developing; following you can read their thoughts.
 "I'm excited for every therapist who will take this course, as it is made to help you approach your practice at a whole new level. We are eager to help your hands work dynamically with more intelligence and how to tackle complex restrictions in the pelvis and abdomen that go far beyond releasing muscles. Additionally, the practitioners will raise their capacity of recognizing and helping the patient manage complex conditions, such as endometriosis, PCOS, fibroids, and IBS."
"I'm excited for every therapist who will take this course, as it is made to help you approach your practice at a whole new level. We are eager to help your hands work dynamically with more intelligence and how to tackle complex restrictions in the pelvis and abdomen that go far beyond releasing muscles. Additionally, the practitioners will raise their capacity of recognizing and helping the patient manage complex conditions, such as endometriosis, PCOS, fibroids, and IBS."
 "One of the best things about the Capstone course is that it provides the participants tools to treat more complicated patients. Topics such as endocrinology, oncology, vulvar dermatology, and surgical procedures are addressed, which will complete the picture for some of those patients that are hard to treat due to the complexity of their case. This knowledge, along with more advanced manual treatment techniques, will add to the skill set of the participants to improve their treatment outcomes. I am excited for the participants to combine their current clinical skills along with some new knowledge and techniques to be able to treat the whole person when working with complex and challenging patients."
"One of the best things about the Capstone course is that it provides the participants tools to treat more complicated patients. Topics such as endocrinology, oncology, vulvar dermatology, and surgical procedures are addressed, which will complete the picture for some of those patients that are hard to treat due to the complexity of their case. This knowledge, along with more advanced manual treatment techniques, will add to the skill set of the participants to improve their treatment outcomes. I am excited for the participants to combine their current clinical skills along with some new knowledge and techniques to be able to treat the whole person when working with complex and challenging patients."
 "Designing and creating Capstone with Nari and Allison was an incredible experience. My own knowledge and clinical expertise grew profoundly while researching and writing this material. Capstone is designed to really take the experienced pelvic health therapist to the next level of understanding and treating more complex patients. I can't wait to see the impact this material has on participants and their patients."
"Designing and creating Capstone with Nari and Allison was an incredible experience. My own knowledge and clinical expertise grew profoundly while researching and writing this material. Capstone is designed to really take the experienced pelvic health therapist to the next level of understanding and treating more complex patients. I can't wait to see the impact this material has on participants and their patients."
There is still time to register for the few remaining seats in Denver this weekend!