Birthing can be an unpredictable process for mothers and babies. With cases of fetal distress, the baby can require rapid delivery. Alternatively, in cases with cephalo-pelvic disproportion, the baby has a larger head, or the mother has a decreased capacity within the pelvis to allow the fetus to travel through the birthing canal. Additionally, the baby may have posterior presentation, colloquially known as “sunny side up” in which the baby’s occipital bone is toward the sacrum. With any of these situations, it is good to know c-sections are an option to safely deliver the child.
 Women may also be inclined to try to get a c-section to avoid pelvic complication or tears or because of a history of a severe prior tear. As pelvic therapists, we know that the number of vaginal births and history of vaginal tears increase the risk of urinary incontinence and prolapse. Yet, many therapists are unfamiliar with the effects of c-section and the impact of rehab for diastasis.
Women may also be inclined to try to get a c-section to avoid pelvic complication or tears or because of a history of a severe prior tear. As pelvic therapists, we know that the number of vaginal births and history of vaginal tears increase the risk of urinary incontinence and prolapse. Yet, many therapists are unfamiliar with the effects of c-section and the impact of rehab for diastasis.
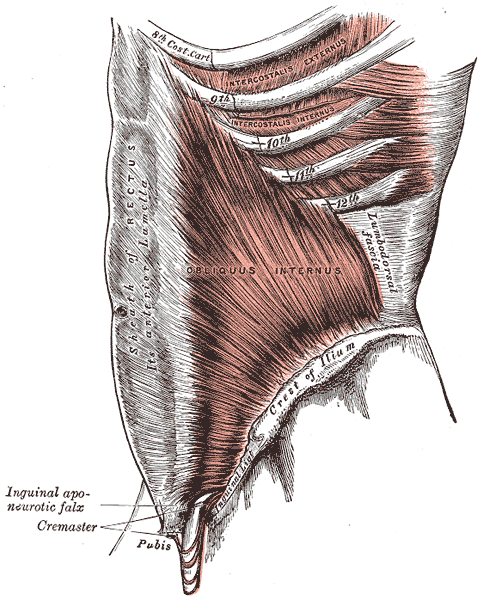
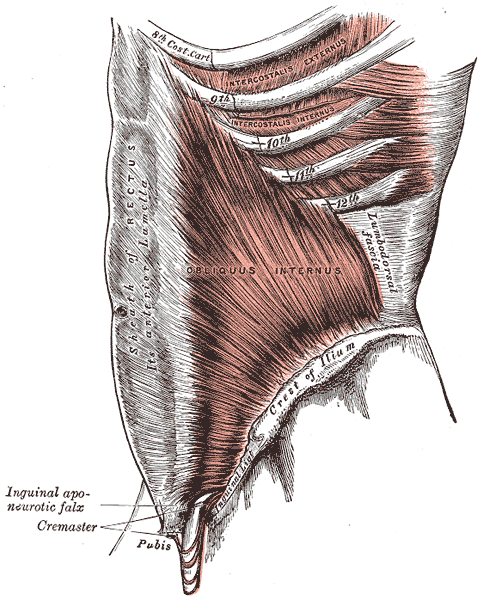
A 2008 dissection study of 37 cadavers studied the path of the ilioinguinal and Iliohypogastric nerves. The course of the nerves was compared with standard abdominal surgical incisions, including appendectomy, inguinal, pfannestiel incisions (the latter used in cesarean sections). The study concluded that surgical incisions performed below the level of the anterior superior iliac spines (ASIS) carry the risk of injury to the ilioinguinal and iloiohypogastric nerves 1. Another 2005 study reported low transverse fascial incision risk injury to the ilioinguinal and Iliohypogastric nerves, and the pain of entrapment of these nerves may benefit from neurectomy in recalcitrant cases.2
Why does injury to the nerves matter? After pregnancy, patients may need rehab and retraining of their abdominal recruitment patterns for diastasis and stability. The ilioinguinal and Iliohypogastric nerves are the innervation for both the transverse abdominus and the obliques below the umbilicus. When we are working to retrain the muscles, certainly neural entrapment or poor firing can greatly impact the success of our intervention as rehab professionals. Interestingly, a study from Turkey showed patients had a significant increase in diastasis recti abdominis (DRA) with a history of 2 cesarean sections and increased parity and recurrent abdominal surgery increase the risk of DRA.2
A fourth study looked at 23 patients with ilioinguinal and Iliohypogastric nerve entrapment syndrome following transverse lower abdominal incision (such as a c-section). In this study, the diagnostic triad of ilioinguinal and Iliohypogastric nerve entrapment after operation was defined as 1) typical burning or lancinating pain near the incision that radiates to the area supplied by the nerve, 2). Clear evidence of impaired sensory perception of that nerve, and 3) pain relieved by local anaesthetic.4
One of the other symptoms we may see in an area of nerve damage is a small outpouching in the area of decreased innervation on the front lower abdominal wall.
So, what can we do with this information? The good news is that as rehab professionals, we can treat along the fascial pathway of the nerve to release in key areas of entrapment. We can mobilize the nerve directly. Neural tension testing can help us differentiate the nerve in question and we can use neural glides and slides after having freed up the nerve from the area of compression. Then, we can increase the communication of the nerve with the muscles by using specific, localized strengthening and stretch in areas of prior compression. All of these techniques are taught in in our course, Lumbar Nerve Manual Treatment and Assessment. Come join us in San Diego May 3-5, 2019 to learn how to differentially diagnose and treat entrapment of all of the nerves of the lumbar plexus.
Okiemy, G., Ele, N., Odzebe, A. S., Chocolat, R., & Massengo, R. (2008). The ilioinguinal and iliohypogastric nerves. The anatomic bases in preventing postoperative neuropathies after appendectomy, inguinal herniorraphy, caesareans. Le Mali medical, 23(4), 1-4.
Whiteside, J. L., & Barber, M. D. (2005). Ilioinguinal/iliohypogastric neurectomy for management of intractable right lower quadrant pain after cesarean section: a case report. The Journal of reproductive medicine, 50(11), 857-859.
Turan, V., Colluoglu, C., Turkuilmaz, E., & Korucuoglu, U. (2011). Prevalence of diastasis recti abdominis in the population of young multiparous adults in Turkey. Ginekologia polska, 82(11).
Stulz, P., & Pfeiffer, K. M. (1982). Peripheral nerve injuries resulting from common surgical procedures in the lower portion of the abdomen. Archives of Surgery, 117(3), 324-327.
Today's guest post comes to us from Kelly Feddema, PT, PRPC. Kelly practices pelvic floor physical therapy in the Mayo Clinic Health System in Mankato, MN, and she became a Certified Pelvic Rehabilitation Practitioner in February of 2014. To learn more about diastasis recti abdominis, consider attending Care of the Postpartum Patient!
It can be a struggle to treat patients with diastasis recti if they don't seek treatment early after giving birth. Many therapists may often find themselves thinking “if I only could have started them sooner.” Why does this condition often get missed at postpartum examinations? I personally deal with symptoms from an undiagnosed diastasis, and I'm a therapist! I didn’t really pay attention to it until I started down the road of becoming a pelvic floor therapist.
 Diastasis recti can be a difficult diagnosis to treat, as the patient may come to us when they are already one year postpartum, and not everyone agrees on the what are the best treatments. To crunch or not crunch? To use a brace or not to brace? It would be great if we had a similar healthcare system to France, where the norm is to have 10-20 postpartum rehabilitation visits with women after child birth. While therapy is available in the United States, women must ask for it.
Diastasis recti can be a difficult diagnosis to treat, as the patient may come to us when they are already one year postpartum, and not everyone agrees on the what are the best treatments. To crunch or not crunch? To use a brace or not to brace? It would be great if we had a similar healthcare system to France, where the norm is to have 10-20 postpartum rehabilitation visits with women after child birth. While therapy is available in the United States, women must ask for it.
There are many programs out there from the more well-known Tupler Technique and Mutu programs to others that come up when searching for exercise ideas. The American Physical Therapy Association (APTA) has a basic program to work on isolating the transverse abdominis (TrA) muscle and then progressing movements in the legs while keeping the TrA activated.
Some research by Paul Hodges and Diane Lee from 2016 in the Journal of Orthopedic Sports Physical Therapy indicates that narrowing the inter-rectus distance with a TrA contraction might improve force transfer between the sides of the abdominals and in turn, improve abdominal mechanics.
Another study in Physiotherapy from December of 2014 by AG Pascoal, et.al. utilized ultrasound to determine the effect of isometric contraction of the abdominal muscles on inter-rectus distance in postpartum women. They found that the while the inter-rectus distance in postpartum women was understandably higher than controls, it significantly lowered during an isometric contraction of the abdominal muscles.
One year later, a study in the same journal by MF Sancho, et.al. had similar findings when studying women who had a vaginal delivery and women who had Cesarean deliveries. They found that abdominal crunch exercises were successful in reducing inter-rectus distance, but drawing-in exercises were not.
As with a lot of research, the findings lead to more questions and ideas to explore. I think it is safe to say that starting safe re-education of the muscles as early as possible is going to provide women the most benefit in reducing diastasis recti, and that will help to prevent further issues in the abdominal and pelvic region.
The following post comes to us in part from Ginger Garner, PT, ATC, PYT, who teaches three yoga courses for Herman & Wallace; Yoga for Pelvic Pain, Yoga as Medicine for Pregnancy, and Yoga as Medicine for Labor and Postpartum. Check out her poster at the Combined Sections Meeting this weekend in Anaheim!

Maternal health care in the United States is abysmal. Especially wretched is care and support of women post-partum. Our insurance system is partially to blame by dictating that women receive only one visit with the provider who participated in the delivery of their baby 6 weeks after the baby is born, no matter the method of delivery. This is often after most of the scary, unexpected side effects of delivery, like heavy bleeding, nipple pain, urinary incontinence, difficulty with bowel movements, scar pain and tremendous mood swings have begun to ease. Only the women who are the most persistent, or those who have chosen unique care models (like out of hospital births with midwives), seem to get real support post-partum, leaving marginalized and less self-driven women to fend for themselves.
What if research could show that immediately treating some of the side effects of birth, like diastasis recti abdominus, which occurs in 50-60% of post-partum women, could result in improved outcomes in the long run? What if someone could prove that retraining and strengthening the abdominal wall as part of a biopsychosocial model empowering women could change the costly effects of prolapse and urinary incontinence treatment later on in life? What if that research aimed to show that treating women in partnership will all care providers was the most effective? These are big questions, but through research beginning with Diastasis Recti Abdominis (DRA), some Women’s Health Physical Therapists trained in Medical Therapeutic Yoga are hoping to highlight some answers.
At CSM in San Diego next month, these researchers (listed below) are presenting a poster via the Section on Women’s Health showcasing their paper, Diastasis Recti Abdominis: A Narrative Review. They found that good, solid research focusing on the co-morbidities and treatment of DRA is really lacking. Most well-done studies focus on the reliability and validity of measurement techniques, showing that calipers and ultrasound are the most valid and reliable ways to measure the gap. There is not even agreement on what precise measurement technically constitutes a DRA, though most agree that normal inter-recti distance is 15-25mm supraumbilically among parous females with digital calipers. (Chiarello 2013).
Besides the obvious cosmetic and general strengthening concerns, why do we care about physical therapy care for a post-partum DRA? Spitznagle’s retrospective chart review of women presenting for gynecological care with a mean age of 52 found that 52% had DRA and 66% of them had a least one support-related pelvic floor muscle dysfunction. Those with DRA were more likely to have pelvic organ prolapse, urinary incontinence and fecal incontinence. Another study by Parker found a DRA prevalence of 74.4% among women with back or pelvic area pain who had delivered at least one child and sought PT. They found a significant difference in VAS pain levels in those with DRA and abdominal or pelvic pain compared to those without DRA. More well-done, prospective studies are really needed to correlate these sequalea in later life to DRA post-partum.
The topic of how to retrain the abdominal wall to restore optimal function and cosmetic appearance is hot in the blogosphere right now. Does it matter if the width of the diastasis recti is reduced? Or is it a matter of having tension in the linea alba as the clinician sinks his/her fingers toward the spine? Biomechanically we know that in order to improve stiffness in the trunk, we need synergistic and symmetrical firing of the diaphragm, transversus abdominis, multifidus and the pelvic floor with proper timing and contraction of the hip and external abdominal muscles. Benjamin completed a review of the research on the effects of exercise in the antenatal and postnatal periods and concluded that antenatal exercise may be protective against the formation of a DRA, but that the available studies are of such poor quality and varied in the way that abdominal/core strengthening was applied in the post-partum population, that it is impossible to tell how or why exercise may or may not help with DRA!
There is clearly a huge hole in the literature and as usual, new mothers are suffering. Women are spending money on programs they find on the internet that are not backed by solid research, because there is not any! Regarding DRA, post-partum women in our country desperately need well-done, high quality studies promoting a specific and well-described exercise for healing. In addition, in our patriarchal health care model, we need to show without a shadow of a doubt that treating post-partum muscle weakness, body mechanics issues and DRA is essential for saving money in the long run on prolapse and urinary incontinence surgery, as well as decreasing expenditure on back pain treatments.
If our discipline could provide this research, ALL women could have access to personal, post-partum recovery. As an established part of the health care system and with longer treatment times and the chance to get to know our patients better, physical therapists are the IDEAL healthcare practitioners to ensure that post-partum women are getting adequate physical retraining, but also psycho-social support that is so lacking in the United States.
The Women’s Health Poster Presentations at CSM in Anaheim will be on Saturday, Feb 20 from 1-3PM. I look forward to meeting with some of you and visiting about what you are working on to further the cause of improving maternal health care and DRA treatment.
Ginger Garner PT, ATC, PYT, Professional Yoga Therapy Institute, Emerald Isle, NC
Elizabeth Trausch, DPT, PYT Des Moines University, Des Moines IA
Stefanie Foster, PT, PYT Asana with Intelligence, Houston, TX
Paige Raffo, PT, PYT, CPI, Balance+Flow Physio, Bellevue, WA
Janet Drake, PT, LCCE, FACCE, PYT, Central Bucks Physical Therapy, Doylestown, PA
Stacie Razzino, PT, PYT, Free Motion Physical Therapy, Melbourne, FL
Blog post by Libby Trausch, DPT
Spitznagle T, Leong F, Van Dillen L, Prevalence of diastasis recti abdominis in a urogynecological patient population, International Urogynecology Journal. 2007; 18: 321-328.
Chiarello CM, Mcauley JA. Concurrent validity of calipers and ultrasound imaging to measure interrecti distance. Orthop Sports Phys Ther. 2013; 43(7): 495-503
Benjamin DR, et al., Effects of exercise on diastasis of the rectus abdominis muscle in the antenatal and postnatal periods: a systematic review. Physiotherapy. 2014 Mar;100(1):1-8.