
A prostate cancer diagnosis often brings more than concerns about survival. It can impact urinary control, sexual function, pelvic comfort, and overall quality of life. Men who undergo radical prostatectomy or radiation therapy frequently experience urinary incontinence and erectile dysfunction, sometimes lasting months or years. Pelvic rehabilitation offers structured, evidence-based strategies to restore function, manage symptoms, and rebuild confidence during recovery.
Understanding Prostate Cancer and Its Impact on Pelvic Health
Prostate cancer is among the most common cancers in men. Risk factors include advancing age, family history, genetic predispositions (such as BRCA2 mutations), race or ethnicity, and lifestyle factors including diet and obesity. Diagnosis typically involves PSA screening, biopsy, and imaging to determine disease stage.
Treatment for localized disease often includes radical prostatectomy, external beam radiation therapy (EBRT), or brachytherapy. Each approach carries potential side effects that can affect urinary, sexual, and pelvic function. Even a nerve-sparing prostatectomy can lead to neuropraxia and disruption of pelvic structures, resulting in urinary leakage and erectile dysfunction (5). Radiation therapy can induce fibrosis, vascular injury, and tissue changes that affect erectile function, bladder, and bowel coordination (3). Combined or salvage treatments can further compound these effects (2).
Urinary Incontinence: The Role of Pelvic Floor Training
Urinary incontinence is one of the most common and distressing post-prostatectomy complications. Pelvic floor muscle training (PFMT) is widely recommended as a first-line intervention. Evidence demonstrates that men who engage in PFMT pre- or early postoperatively regain continence faster and experience less severe leakage than those who do not (3).
Effective PFMT focuses on both slow- and fast-twitch muscle contractions, integrating exercises into functional activities, and employing biofeedback or ultrasound to ensure proper engagement (4). Although differences in long-term continence may diminish, early training significantly improves quality of life and independence during the initial recovery months.
 Addressing Erectile Dysfunction Through Rehabilitation
Addressing Erectile Dysfunction Through Rehabilitation
Erectile dysfunction (ED) affects 30–80% of men after prostate cancer treatment, depending on nerve-sparing technique, age, baseline function, and comorbidities. Neurovascular damage, fibrosis, and ischemia are key contributors.
Radiation therapy further increases risk over time (1).
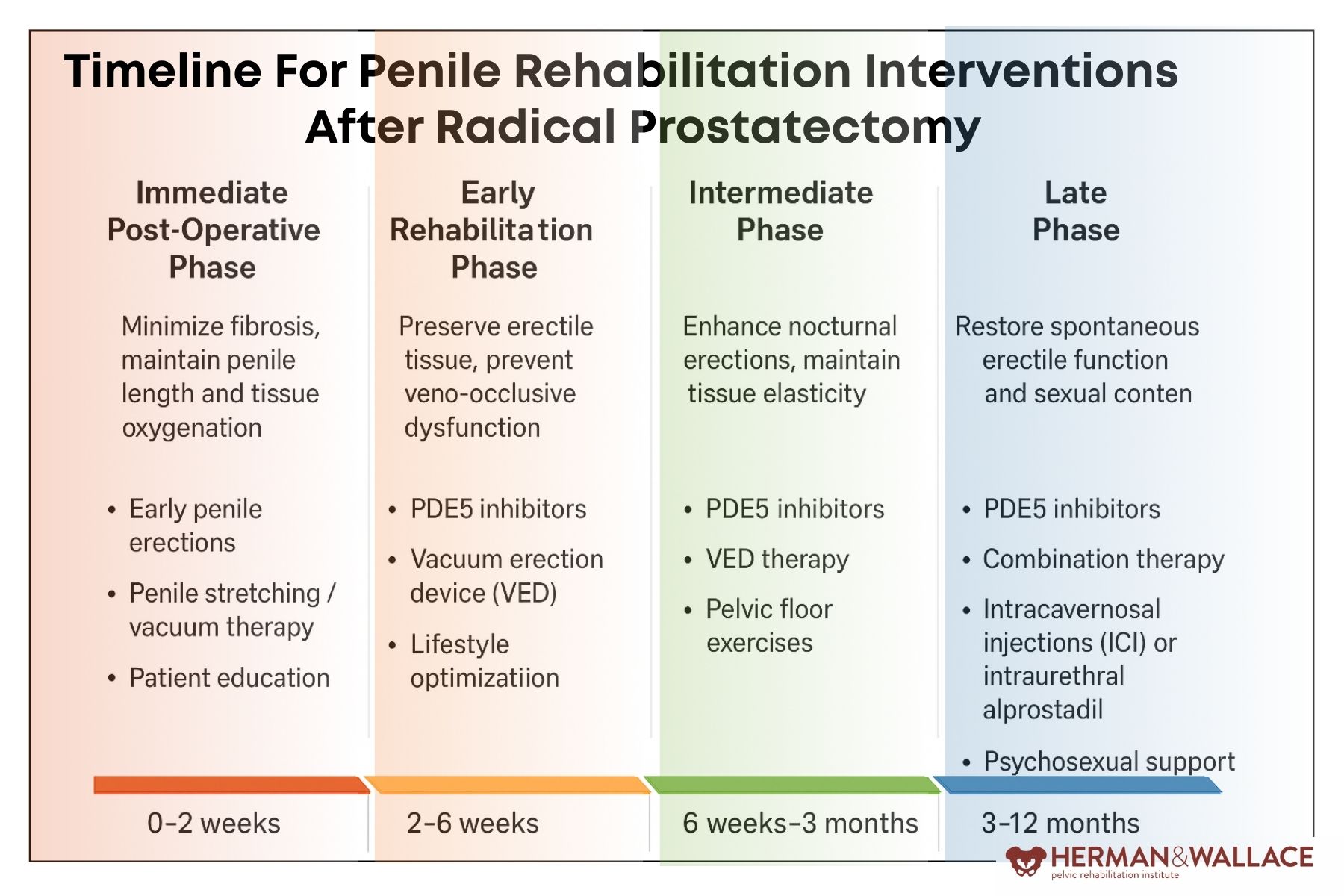
Penile rehabilitation, initiated early, promotes tissue health and functional recovery. Strategies include PDE5 inhibitors, vacuum erection devices, intracavernosal injections, and emerging techniques such as low-intensity shockwave therapy. PFMT complements these strategies by strengthening pelvic floor support, reducing coexisting muscle hypertonicity, and enhancing neuromuscular coordination. Combined interventions yield better outcomes than single-modality approaches.
Managing Pain, Fibrosis, and Pelvic Discomfort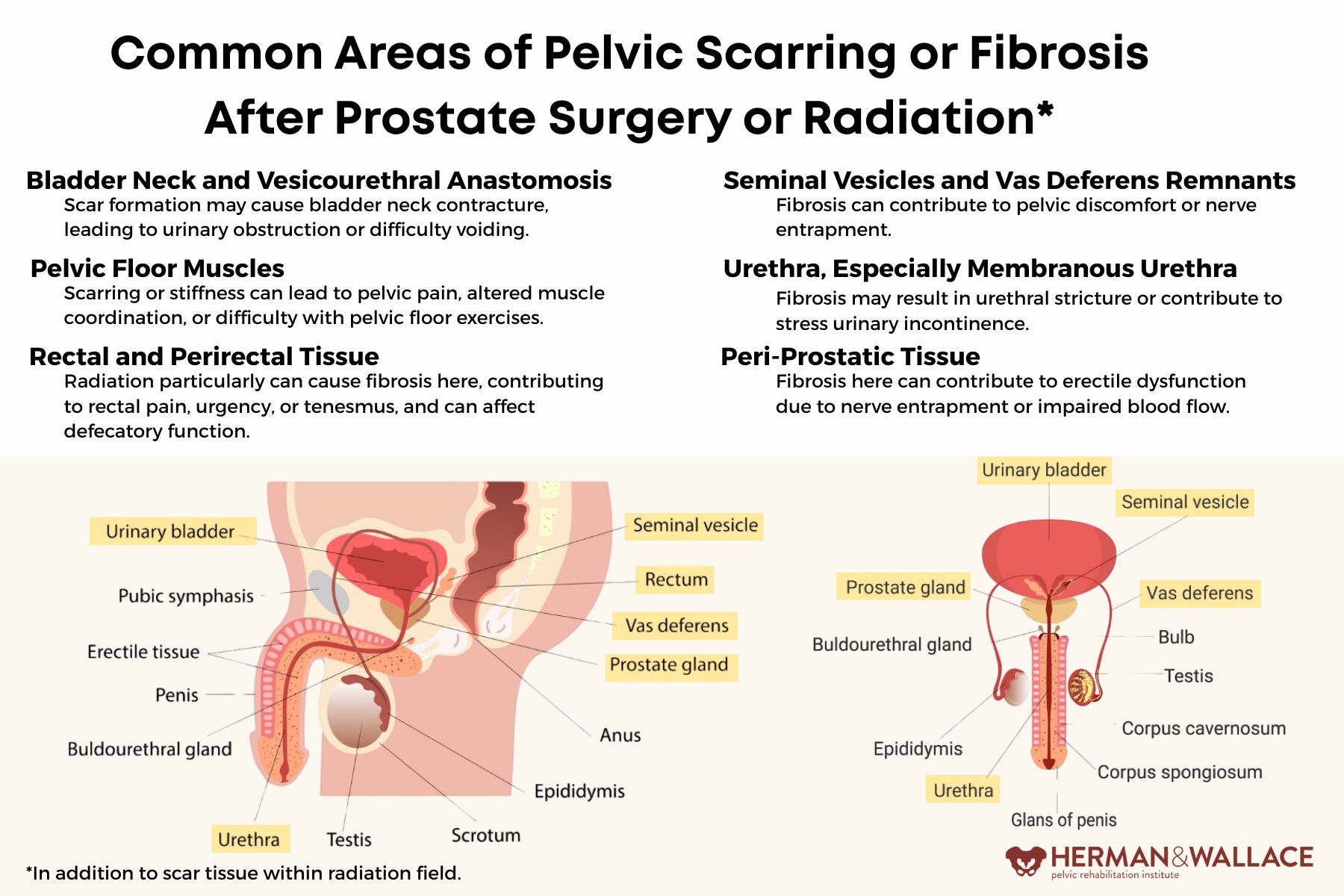
Men may also experience pelvic pain, scar adhesions, muscle hypertonicity, or radiation-induced fibrosis, which can interfere with mobility and rehabilitation adherence. Pelvic rehabilitation addresses these challenges through manual therapy, myofascial release, scar mobilization, neural desensitization, stretching, and relaxation techniques. A holistic approach ensures that pain and fibrosis do not amplify guarding or disrupt neuromuscular coordination, allowing patients to regain functional independence.
Integrating Rehabilitation into Recovery
Prehabilitation by initiating pelvic floor training before surgery can “prime” the neuromuscular system, improving early outcomes. Interventions should be individualized, taking into account anatomy, treatment modality, and comorbidities. Functional progression from isolated contractions to daily activities ensures that strength and coordination translate into meaningful improvements in continence, sexual function, and mobility.
Interdisciplinary collaboration with urologists, radiation oncologists, sexual medicine specialists, psychologists, and nurses enhances recovery, supports timely referrals, and addresses psychosocial aspects of treatment. Realistic expectations and patient education about recovery timelines are critical; while continence may return within months, sexual function may take longer.
Case Example: A 62-year-old man undergoing nerve-sparing robotic prostatectomy began PFMT preoperatively and continued structured pelvic rehabilitation postoperatively. Eight weeks after surgery, he initiated penile rehabilitation with PDE5 inhibitors and vacuum devices alongside ongoing PFMT. At six months, he regained urinary continence, and by 12 months reported meaningful improvements in erectile function. This phased, individualized approach exemplifies how rehabilitation supports functional recovery and quality of life.
Conclusion
Prostate cancer treatment affects multiple systems: neuromuscular, vascular, connective tissue, and psychological. Pelvic rehabilitation offers structured strategies to address urinary incontinence, erectile dysfunction, pelvic pain, and mobility deficits. By combining PFMT, penile rehabilitation, manual therapy, and individualized functional progression, rehabilitation professionals play a crucial role in helping men regain independence and confidence.
This two-day course focuses on male pelvic cancers, including prostate, penile, and testicular cancers, as well as colorectal and anal cancers. Participants will learn about diagnosis, prognosis, medical treatment sequelae, rehabilitation strategies, nutritional considerations, and home program interventions. Hands-on labs provide immediate application of skills, and participants must register with a partner or arrange a volunteer for rectal and perineal exams. Register today to expand your clinical expertise and elevate the care you provide to men recovering from pelvic cancers.
References:
- Nicolai, M., Urkmez, A., Sarikaya, S., Fode, M., Falcone, M., Albersen, M., Gul, M., Hatzichristodoulou, G., Capogrosso, P., & Russo, G. I. (2021). Penile Rehabilitation and Treatment Options for Erectile Dysfunction Following Radical Prostatectomy and Radiotherapy: A Systematic Review. Frontiers in Surgery, 8, 636974. https://doi.org/10.3389/fsurg.2021.636974
- Al Hussein Al Awamlh B, Wallis CJD, Penson DF, et al. Functional Outcomes After Localized Prostate Cancer Treatment. JAMA. 2024; 331(4): 302–317. doi:10.1001/jama.2023.26491. https://jamanetwork.com/journals/jama/fullarticle/2814131
- Milios, J.E., Ackland, T.R. & Green, D.J. Pelvic floor muscle training in radical prostatectomy: a randomized controlled trial of the impacts on pelvic floor muscle function and urinary incontinence. BMC Urol 19, 116 (2019). https://doi.org/10.1186/s12894-019-0546-5
- Milios JE, Ackland TR, Green DJ. Pelvic Floor Muscle Training and Erectile Dysfunction in Radical Prostatectomy: A Randomized Controlled Trial Investigating a Non-Invasive Addition to Penile Rehabilitation. Sex Med. 2020 Sep; 8 (3): 414-421. doi: 10.1016/j.esxm.2020.03.005. Epub 2020 May 14. PMID: 32418881; PMCID: PMC7471070. https://pmc.ncbi.nlm.nih.gov/articles/PMC7471070/
- Newman, D. (2024, December 9). Pelvic muscle rehabilitation after radical prostatectomy. UroToday. https://www.urotoday.com/video-lectures/localized-prostate-cancer/video/4446-pelvic-muscle-rehabilitation-after-radical-prostatectomy-diane-newman.html








































