There's a lot going on in the world of pelvic rehab, and continuing education is no exception! This March, Herman & Wallace is hosting NINE courses around the country. It's a lot to keep up with, so we thought you might appreciate a brief overview of what's coming up next!
Where's this pain coming from?
Pelvic pain can have many sources, and Elizabeth Hampton wants to help you quickly get to the source. Finding the Driver in Pelvic Pain empowers you to play detective in order to help even the most complex patients. Don't miss out on Finding the Driver in Pelvic Pain in San Diego, CA on March 4-6, 2016
What goes in eventually comes out
How important is a good diet? For most of us eating healthy is important, and for many pelvic rehab patients it is a necessity. That's why Megan Pribyl wrote her "Nutrition Perspectives for the Pelvic Rehab Therapist" course. This beginner level course is intended to expand the your knowledge of the metabolic underpinnings for local to systemically complex disorders. Don't miss out on Nutrition Perspectives for the Pelvic Rehab Therapist - Kansas City, MO - March 5-6, 2016!
There's fascia everywhere!
Fascial mobilization is a rising star in pelvic rehab treatment techniques, and Ramona Horton is excited to share it with you! "Mobilization of the Myofascial Layer: Pelvis and Lower Extremity" is the best opportunity you'll get to learn about the evaluation and treatment of myofascia for pelvic dysfunction. Check it out on our continuing education course page. Ramona will be teaching these techniques in Santa Barbara, CA on March 11-13.
Giving birth hurts
Sometimes the newborn is the one to get all the attention, but what about the new mother? Be sure that you can help postpartum women with symptoms like postural dysfunction, pelvic girdle dysfunction, diastasis recti abdominis and more by attending Care of the Postpartum Patient in Seattle, WA this March 12-13, taught by the wonderful Holly Tanner!
Vulvar pain is easy to have and hard to lose
12% of women in the US have vulvar pain for 3 or more months at some stage in their life. It takes a multidisciplinary approach to address all the causes and co-morbidities, and that is exactly what you'll get at Dee Hartmann's Vulvodynia: Assessment and Treatment in Houston, TX on March 12-13, 2016. Dee aims to address the vicious cycle of pain, visceral and sexual dysfunction, and the general hit to quality of life that patients with vulvodynia suffer from.
The challenge of SI joint pain
The sacroiliac joint, pelvic girdle, and pelvic ring sure can take a beating, and Peter Philip knows how to keep you moving. Through exercise and stabilization, the pelvic rehab practitioner can quickly treat pain in the lumbopelvic-hip complex. Learn all about the direct and indirect anatomy that influences the sacroiliac joint, and then get ready to find and treat the source of pain and dysfunction in Sacroiliac Joint Treatment in Minneapolis, MN on March 19-20, 2016.
Taxes and Menopause
The menopause transition is not something many people look forward to. For some women it goes more smoothly than others, and it's the less fortunate ones who need access to a well-trained pelvic care professional. Michelle Lyons is flying in from Ireland to help you to become that pro! Be it vaginal atrophy, sexual health dysfunction, pelvic organ prolapse, or any other of the myriad possible symptoms of menopause, you'll be equipped to handle them all after attending Menopause: A Rehabilitation Approach in Atlanta, GA on March 19-20, 2016.
After menopause, more than half of women may have vulvovaginal symptoms that can impact their lifestyle, emotional well being and sexual health. What's more, the symptoms tend to co-exist with issues such as prolapse, urinary and/or bowel problems. But unfortunately many women aren't getting the help they need, despite a growing body of evidence that skilled pelvic rehab interventions are effective in the management of bladder/bowel dysfunctions, POP, sexual health issues and pelvic pain.
 Vaginal dryness, hot flashes, night sweats, disrupted sleep, and weight gain have been listed as the top five symptoms experienced by postmenopausal women in North America and Europe, according to a study by Minkin et al 2015, and they also concluded ‘The impact of postmenopausal symptoms on relationships is greater in women from countries where symptoms are more prevalent.’ Between 17% and 45% of postmenopausal women say they find sex painful, a condition referred to medically as dyspareunia. Vaginal thinning and dryness are the most common cause of dyspareunia in women over age 50. However pain during sex can also result from vulvodynia (chronic pain in the vulva, or external genitals) and a number of other causes not specifically associated with menopause or aging, particularly orthopaedic dysfunction, which the pelvic physical therapist is in an ideal position to screen for.
Vaginal dryness, hot flashes, night sweats, disrupted sleep, and weight gain have been listed as the top five symptoms experienced by postmenopausal women in North America and Europe, according to a study by Minkin et al 2015, and they also concluded ‘The impact of postmenopausal symptoms on relationships is greater in women from countries where symptoms are more prevalent.’ Between 17% and 45% of postmenopausal women say they find sex painful, a condition referred to medically as dyspareunia. Vaginal thinning and dryness are the most common cause of dyspareunia in women over age 50. However pain during sex can also result from vulvodynia (chronic pain in the vulva, or external genitals) and a number of other causes not specifically associated with menopause or aging, particularly orthopaedic dysfunction, which the pelvic physical therapist is in an ideal position to screen for.
According to the North America Menopause Society, ‘…beyond the immediate effects of the pain itself, pain during sex (or simply fear or anticipation of pain during sex) can trigger performance anxiety or future arousal problems in some women. Worry over whether pain will come back can diminish lubrication or cause involuntary—and painful—tightening of the vaginal muscles, called vaginismus. The result can be a vicious circle, again highlighting how intertwined sexual problems can become.’
The research has demonstrated that the optimal strategy for post-menopausal stress incontinence is a combination of local hormonal treatment and pelvic floor muscle training – the strategy of combining the two approaches has been shown to be superior to either approach used individually (Castellani et al 2015, Capobianco et al 2012) and similar conclusions can be drawn for promoting sexual health peri- and post-menopausally.
The pelvic rehab specialist may be called upon to screen for orthopaedic dysfunction in the spine, hips or pelvis, to discuss sexual ergonomics such as positioning or the use of lubricant as well as providing information and education about sexual health before, during and after menopause.
To learn more about sexual health and pelvic floor function/dysfunction at menopause, join me in Atlanta in March for Menopause: A Rehab Approach.
Prevalence of postmenopausal symptoms in North America and Europe, Minkin, Mary Jane MD, NCMP1; Reiter, Suzanne RNC, NP, MM, MSN2; Maamari, Ricardo MD, NCMP3, Menopause:November 2015 - Volume 22 - Issue 11 - p 1231–1238
Low-Dose Intravaginal Estriol and Pelvic Floor Rehabilitation in Post-Menopausal Stress Urinary Incontinence, Castellani D. · Saldutto P. · Galica V. · Pace G. · Biferi D. · Paradiso Galatioto G. · Vicentini C., Urol Int 2015;95:417-421
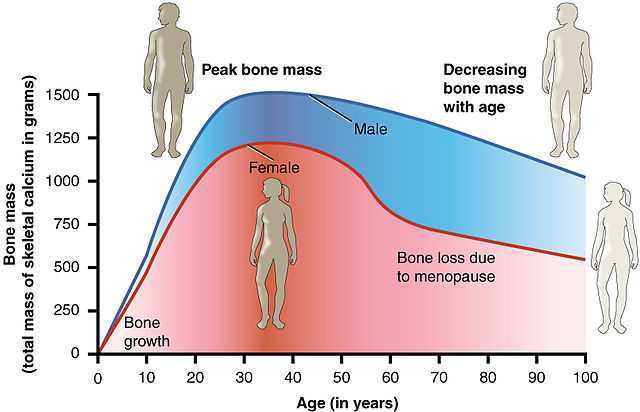
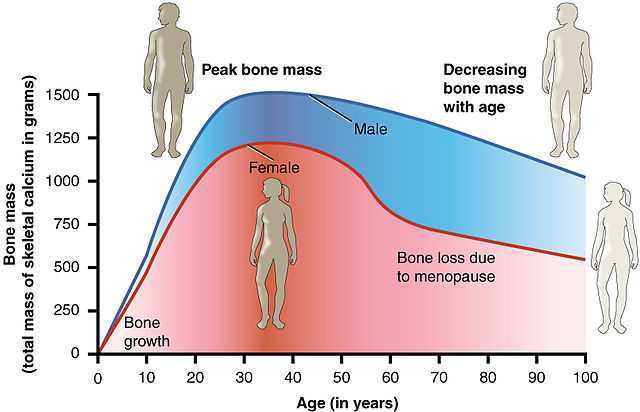
Commonly in physical therapy we treat patients with osteopenia or osteoporosis, however, they are usually in our office for another diagnosis such as back, hip, or pelvic pain as the primary complaint and we learn about the osteoporosis from health history review. Physical therapy is an opportunity to provide them with not just relief from their primary complaint, but a chance to learn from a professional how to move in a more healthy way and learn the right ways to exercises to make a regular routine that can help them to protect their body and even slow or stop bone mineral density loss. This is important as the primary concern for a patient with the diagnosis of osteoporosis is risk of fracture (especially of the hip or spine) due to minimal trauma because of low bone mineral density. So let’s make sure we are giving patients comprehensive exercise programs that address their primary complaint, however be comprehensive and include exercise modes that may reduce fractures and may improve bone mineral density.
 An interesting article by Palombaro et al1 in 2013 from Physical Therapy discusses a Cochrane review by Howe et al2 and applies the findings from this review to an example patient similar to the participants reviewed in the study. The goal of the article is to link evidence in the literature with how we practice as PT’s. The topic explored in the systematic review by Howe et al was exercise for the management of osteoporosis in women postmenopause and which exercise approaches reduce the loss of bone mineral density or reduce chance of fractures in women who are healthy postmenopause. The systematic review2 included 43 randomized controlled studies of postmenopausal women age 45-70 where the intervention groups included exercises that improved aerobic capacity or improved aerobic capacity and muscle strength and had a comparison group completing “usual activity: or placebo intervention. The duration of exercise lasted from 6 months to 2 years in the various studies. The results of the review demonstrated decreased bone loss (of the spine or hips) in groups who performed any type of exercise compared to the control groups. The review also performed additional sub group analysis to take into account the various types of exercise programs in the studies and found favorable effect for all types of exercises completed (dynamic, low force, high force, weight bearing, or non-weight bearing) all had favorable effect on bone density. The take home message from this systematic review is that exercise programs combining various forms of exercises lasting 6 months to 2 years resulted in reduced risk for fracture, and a slightly beneficial effect on bone mineral density of the spine, trochanter, and neck of the femur in postmenopausal women with osteoporosis.
An interesting article by Palombaro et al1 in 2013 from Physical Therapy discusses a Cochrane review by Howe et al2 and applies the findings from this review to an example patient similar to the participants reviewed in the study. The goal of the article is to link evidence in the literature with how we practice as PT’s. The topic explored in the systematic review by Howe et al was exercise for the management of osteoporosis in women postmenopause and which exercise approaches reduce the loss of bone mineral density or reduce chance of fractures in women who are healthy postmenopause. The systematic review2 included 43 randomized controlled studies of postmenopausal women age 45-70 where the intervention groups included exercises that improved aerobic capacity or improved aerobic capacity and muscle strength and had a comparison group completing “usual activity: or placebo intervention. The duration of exercise lasted from 6 months to 2 years in the various studies. The results of the review demonstrated decreased bone loss (of the spine or hips) in groups who performed any type of exercise compared to the control groups. The review also performed additional sub group analysis to take into account the various types of exercise programs in the studies and found favorable effect for all types of exercises completed (dynamic, low force, high force, weight bearing, or non-weight bearing) all had favorable effect on bone density. The take home message from this systematic review is that exercise programs combining various forms of exercises lasting 6 months to 2 years resulted in reduced risk for fracture, and a slightly beneficial effect on bone mineral density of the spine, trochanter, and neck of the femur in postmenopausal women with osteoporosis.
At the end of this article1 the authors give a case of an active, postmenopausal female patient with history of osteopenia without a fracture seeking PT for an unrelated complaint. The authors took the findings from this review and showed the relevance of the findings, applying it to the patient and the outcome of care for this patient when giving her an exercise program. We can implement findings from this review simply to the common question posed by our patients… “what exercises should I be doing to help with my osteoporosis?”
Exercises for a patient with osteoporosis should be forms of exercises that may improve bone density by loading bones (weight bearing exercise) and by increasing muscle mass (strengthening resistive exercise) to produce mechanical load and stress to the bone. Also as we age we tend to experience changes with not just a reduction of bone mineral density, but also a reduction of muscle mass. Additionally complicating the natural progression of aging are balance and gait changes leading to impaired physical performance. We should be giving our patients a comprehensive exercise program including safe weight bearing exercises and a strengthening program. Common examples of weight bearing exercises include regular walking, jogging, jumping, dancing, and racquet sports. Common examples of strengthening activities would include use of resistive exercises for upper and lower body with bands, free weights or resistive equipment. All of these classifications of exercise were considered as beneficial in the review.
To learn more about helping postmenopausal patients, consider joining Michelle Lyons, PT, MISCP for "Menopause Rehabilitation and Symptom Management". This course will be taking place March 19, 2016 - March 20, 2016 in Atlanta, GA. Another great resource to consider is "Geriatric Pelvic Floor Rehab: Modifying Treatments for Seniors and Older Patients" with Heather S. Rader, PT, DPT, BCB-PMD, taking place January 16-17, 2016 in Tampa, FL.
1 Palombaro, K. M., Black, J. D., Buchbinder, R., & Jette, D. U. (2013). Effectiveness of exercise for managing osteoporosis in women postmenopause. Physical Therapy, 93(8), 1021-1025.
2 Howe, T. E., Shea, B., Dawson, L. J., Downie, F., Murray, A., Ross, C., ... & Creed, G. (2011). Exercise for preventing and treating osteoporosis in postmenopausal women (Review).
![By Mikael Häggström (Own work) [CC0], via Wikimedia Commons](https://upload.wikimedia.org/wikipedia/commons/thumb/d/d9/Symptoms_of_menopause_%28raster%29.png/512px-Symptoms_of_menopause_%28raster%29.png) Sleep difficulties are a common problem among women in the menopausal period, with hot flashes and night sweats commonly interfering with a restful night’s sleep. According to Baker and colleaguesBaker, 2015 , disturbed sleep is present in 40-60% of women in the menopausal transition. The authors also point out that insomnia is not well characterized, with poor identification of a physiologic basis for the sleep disturbances. In the research linked above, perimenopausal women diagnosed with clinical insomnia (n=38) were compared to women who did not have insomnia (n=34). Outcome measures included the Beck Depression Inventory, the Greene Climacteric Scale, sleep diaries, sleep studies, and nocturnal hot flashes via dermal conductance meters.
Sleep difficulties are a common problem among women in the menopausal period, with hot flashes and night sweats commonly interfering with a restful night’s sleep. According to Baker and colleaguesBaker, 2015 , disturbed sleep is present in 40-60% of women in the menopausal transition. The authors also point out that insomnia is not well characterized, with poor identification of a physiologic basis for the sleep disturbances. In the research linked above, perimenopausal women diagnosed with clinical insomnia (n=38) were compared to women who did not have insomnia (n=34). Outcome measures included the Beck Depression Inventory, the Greene Climacteric Scale, sleep diaries, sleep studies, and nocturnal hot flashes via dermal conductance meters.
Results of the study concluded that women with insomnia, compared with controls, had higher levels of psychologic, somatic, vasomotor symptoms, and had higher scores on the depression inventory, shorter sleep duration, and lower sleep efficiency. Women with insomnia were also more likely to have hot flashes, with number of hot flashes predicting awakenings during the sleep study. Episodes of wakefulness after sleep onset, and decreased time of sleep were noted in the women who were diagnosed with new-onset insomnia.
Because untreated insomnia is associated with negative consequences including hypertension, stroke, diabetes, and depression, the authors suggest that women who are diagnosed with insomnia should be treated for their insomnia. If you are interested in learning about natural methods to manage and reduce hot flashes, among many other interesting topics, you will likely enjoy Herman & Wallace faculty Michelle Lyons and her newer course: Special Topics in Women’s Health. The next chance to hear Michelle discuss these topics is in Denver in January. Bring your skis!
Baker, Fiona C. et al. "Insomnia in women approaching menopause: Beyond perception" Psychoneuroendocrinology, Volume 60, 96-104 October 2015
Cognition in later years may be affected by premature menopause, according to an article published online in the British Journal of Obstetrics and Gynaecology. In the study 4,868 women at least 65 years old were assessed on a cognitive test battery and were evaluated for clinical dementia. Associations between the subject’s age at menopause, surgical versus natural menopause, use of menopausal hormone therapy, and cognitive function later in life were studied. According to introductory concepts described in the article, estrogen level changes postmenopause are associated with brain atrophy and memory complaints.
Tests were administered at baseline, and again at 2, 4 and 7 years from baseline. Tools included the Mini-Mental State Examination (MMSE) for global cognitive function, Benton’s Visual Retention Test (BVRT) for visual memory assessment, Isaacs Set Test for verbal fluency or semantic access, and the Trail Making Tests A and B for timed visual motor tasks of psychomotor speed and attention and executive function. Unrelated to cognitive function, The Rosow and Breslau mobility and Instrumental Activities of Daily Living scales, the Centre for Epidemiology Studies Depression Scale (CES-D), and other instruments were used to assess socioeconomic, demographic, lifestyle and health information. Dementia was also evaluated by a trained psychologist (or neurologist if subject was suspected to have dementia) and cases were assessed by a panel of dementia experts as a third step in the process.
Natural menopause was noted in 79% of the subjects, surgical menopause in 10%, and 11% due to other causes including radiation, chemotherapy, or unknown. Less than 1 in 7 women was currently using hormone therapy, and over 1/5 used hormone therapy at menopause (most commonly reported treatment was transdermal estradiol- median time of use was 10 years).
The authors concluded that variables such as verbal fluency, visual memory, psychomotor speed and global cognitive function can be negatively impacted by premature menopause. Specifically, premature menopause including premature ovarian failure or surgical menopause at 40 years of age or less was independently associated with increased risk of poor verbal fluency and visual memory later in life. Premature menopause was also associated with increased risk of psychomotor speed and global cognitive decline. The primary conclusion of the article is that when an ovariectomy is being considering in younger women, the potential negative impact on cognitive function should make up part of the risk/benefit discussion. Hormonal influence during various stages of a woman’s life can have a dramatic impact on many variables impacting quality of life and rehabilitation efforts. To learn more about menopause, the Institute offers several courses that contain information about rehabilitation for women throughout the lifespan.
Herman & Wallace offers an excellent course called "Menopause Rehabilitation and Symptom Management ", where you can learn about evaluating and treating menopause patients. Forward thinking therapists can provide an integrative, safe and effective/evidence based approach, such as menopausal weight loss, cardiovascular health promotion and mind body awareness, and Menopause: A Rehabilitation Approach - Atlanta, GA on March 19-20, 2016 is a great opportunity to learn such skills.