One of my favorite things as the instructor of the Menopause Transitions course is when participants ask questions. Whether it is something about their own menopause journey or when a patient is struggling with symptoms, it thrills me to provide resources and clarity to help them make informed decisions.
The following are some of the questions that have come up in class or that have been brought to my attention via email after participants are back in the clinic:
Given the many benefits of hormone therapy, should every patient take it during or after perimenopause for the prevention of chronic disease?
This is an excellent question! Based on recommendations from The Menopause Society, hormone therapy is approved for the treatment of vasomotor symptoms, genitourinary symptoms, and the prevention of osteoporosis.
Hormones are often lauded as a benefit for reducing both heart disease and dementia. While it has shown some benefit for heart disease, it is not recommended as a preventative treatment. The same holds true for prevention of neurodegenerative disease. The research on the benefits of hormones in cardiovascular and neurodegenerative disease reductions is often looking a different outcomes.
Each study may use a different type of estrogen. An oral estrogen blend (Premarin), an estradiol patch, and an oral estradiol can all have different effects on the body. You simply cannot extrapolate data from one study to the next if the type of estrogen studied was different. In addition, some research shows no benefit. Based on the current data, hormones are not a slam dunk for the prevention of heart disease and dementia. More studies with the types of hormones that are currently being prescribed are needed before recommending them as prevention.
Hormone therapy is very effective for improving bone density. Osteoporosis is a painless process of bone loss. If a person is not experiencing hot flashes and is concerned about their risk for osteoporosis, they could opt for a DEXA scan and then make an informed decision with their provider regarding hormone therapy.
Is there a dose of estrogen that is more beneficial for treating osteoporosis?
In the 2021 position statement for the management of osteoporosis, the Menopause Society cites a study that shows improved bone density with increased dosage. Oral estradiol doses of .02mg, .05mg, and .075mg after 2 years of treatment correlated with an improvement in lumbar spine bone density of .4%, 2.3%, and 2.7% (Greenwald et.al, 2005). While improvement can be gained from a smaller dose, a higher dose does have more benefit. Once again, informed decision-making with a knowledgeable provider is needed.
What are your go-to resources for all things menopause?
Based on the answers to the two previous questions, I think you can see that The Menopause Society is the gold standard when it comes to all things menopause. The position statements are available on their website and can be accessed for free. This includes guidelines on hormones, non-hormonal treatments, genitourinary syndrome of menopause, and osteoporosis. They also have monthly practice pearls, which include many pertinent topics on current treatments and health concerns for the patient in the transition.
Another great resource is Jen Gutner’s The Vagenda. While complete articles require a subscription to her Substack, she does offer a free email version that shares information about many of the topics flying around in the social media sphere. Her opinions are not always popular, but they are always research-based.
A final resource would be Women Living Better. This website was started by women frustrated with their own perimenopause experience and has resources for patients wanting to know more about options for treatment and symptoms experienced during this time. The founders have also been responsible for some interesting research regarding a survey of 3200 women in perimenopause. This is also available on their website.
Keep in mind that there are many social media influencers with millions of followers who also offer information. They have YouTube channels, Instagram, and websites. Menopause seems to be everywhere! While it is extremely valuable to get the message out there, the conclusions offered are often oversimplified in the attempt to push a quick and easy narrative. If I have learned anything in my knowledge journey, it is that there is no one-size-fits-all answer. Treatment is very individualized based on health status, risk factors, and personal preferences. Nuance is the key when it comes to offering the best outcomes.
If you would like to learn more on this topic, then join me on April 26-27, 2025, in Menopause Transitions and Pelvic Rehabilitation to understand more about the physiological consequences to the body as hormones decline and how to assist our patients in lifestyle habits for successful aging.
References:
- The 2020 genitourinary syndrome of menopause position statement of The North American Menopause Society. Menopause, 2020. 27(9): p. 976-992.
- Management of osteoporosis in postmenopausal women: the 2021 position statement of The North American Menopause Society. Menopause, 2021. 28(9): p. 973-997.
- The 2022 hormone therapy position statement of The North American Menopause Society. Menopause, 2022. 29(7): p. 767-794.
- Greenwald, M.W., et al., Oral hormone therapy with 17beta-estradiol and 17beta-estradiol in combination with norethindrone acetate in the prevention of bone loss in early postmenopausal women: dose-dependent effects. Menopause, 2005. 12(6): p. 741-8.
- The Nonhormone Therapy Position Statement of The North American Menopause Society" Advisory, P., The 2023 nonhormone therapy position statement of The North American Menopause Society. Menopause, 2023. 30(6): p. 573-590.
AUTHOR BIO
Christine Stewart, PT, CMPT
 Christine Stewart, PT, CMPT (she/her) graduated from Kansas State University in 1992 and went on to pursue her master’s degree in physical therapy from the University of Kansas Medical Center, graduating in 1994. She began her career specializing in orthopedics and manual therapy, then became interested in women’s health after the birth of her second child.
Christine Stewart, PT, CMPT (she/her) graduated from Kansas State University in 1992 and went on to pursue her master’s degree in physical therapy from the University of Kansas Medical Center, graduating in 1994. She began her career specializing in orthopedics and manual therapy, then became interested in women’s health after the birth of her second child.
Christine developed her pelvic health practice in a local hospital with a focus on urinary incontinence and prolapse. She left the practice in 2010 to work at Olathe Health to further focus on pelvic rehabilitation for all genders and obtain her CMPT from the North American Institute of Manual Therapy. She completed Diane Lee’s Integrated Systems Model education series in 2018. Her passion is empowering patients through education and treatment options for the betterment of their health throughout their lifespan. She enjoys speaking to physicians and to community-based organizations on pelvic health physical therapy.

Hi, I’m Deb Gulbranson, co-creator of the course Osteoporosis Management: An Introductory Course for Healthcare Professionals. Along with my partner, Frank Ciuba, we have created a program based on the works of Sara Meeks, whom we taught with for many years.
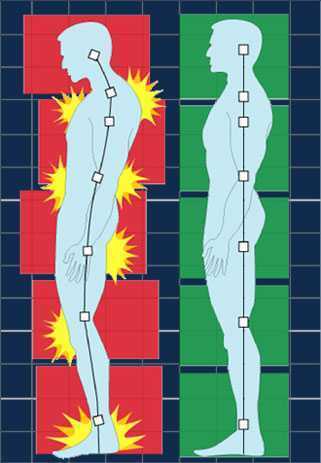
We know that posture is important, and we may include it in our evaluations, but how do we objectively measure it? How much time do we spend on education, training, exercises, and return demonstration? Chances are, not as much as we should.
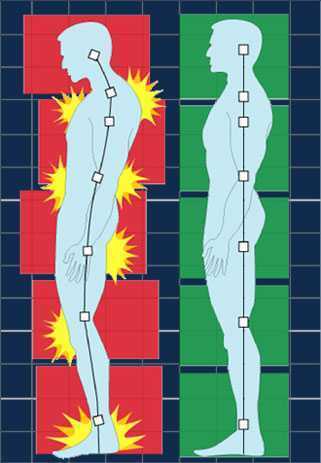
Optimal alignment affects our breathing, balance, efficiency of gait, digestion, AND bone density.
In order to increase bone density, we need to weight bear through the skeleton, not in front of it. Compression fractures occur along the anterior aspect of the vertebral bodies. Strengthening the back extensors has also been shown to increase bone density. Therefore, someone with a hyper-kyphotic posture of the thoracic spine is at risk for fracture due to increased pressure anteriorly and overstretched, weakened musculature posteriorly. Statistics show that 1:2 women and 1:4 men will have a fragility fracture due to low bone mass.
How do we objectively measure and describe a person’s alignment?
 A quick and simple way is using a wall and measuring tape. Have your patient stand with their heels, sacrum, and thoracic apex of the spine against the wall. There are two options to measure using the OWD or the TWD. Occiput to Wall Distance or Tragus to Wall Distance. The Tragus is the small bump of cartilage in front of the ear canal. Both OWD and TWD have a positive relationship with the Cobb angle, and although they’re not as specific, they are both equally effective. It’s a matter of preference. Frank prefers the TWD since it’s easier to see and measure. However, the score does not tell you how far away from the wall the head is. There will always be a positive number based on the size and shape of the head.
A quick and simple way is using a wall and measuring tape. Have your patient stand with their heels, sacrum, and thoracic apex of the spine against the wall. There are two options to measure using the OWD or the TWD. Occiput to Wall Distance or Tragus to Wall Distance. The Tragus is the small bump of cartilage in front of the ear canal. Both OWD and TWD have a positive relationship with the Cobb angle, and although they’re not as specific, they are both equally effective. It’s a matter of preference. Frank prefers the TWD since it’s easier to see and measure. However, the score does not tell you how far away from the wall the head is. There will always be a positive number based on the size and shape of the head.
I prefer the OWD because whatever the measurement is, it tells me how far forward the head is. 0 equals optimal alignment. The downside is that it’s a little harder to pinpoint the most prominent point of the occiput.
In both cases, the measurement gives us a baseline to measure against. These can be used as screens in a health fair, during a PT screen for patients without a diagnosis of low bone density, and certainly as part of a full eval for patients with known osteoporosis, a compression fracture, or even osteopenia.
These measures, taken periodically, can be very motivating for patients. Generally, we see not only a decrease in the hyper-kyphosis distance but also an increase in height.
This is only one of several ways to assess and describe posture and alignment. We hope you’ll consider joining us to learn more about the treatment protocols and exercise programs in our upcoming Osteoporosis Management course on April 26th.
AUTHOR BIO
Deb Gulbrandson, PT, DPT
 Deb Gulbrandson, DPT (she/her) has been a physical therapist for over 49 years with experience in acute care, home health, pediatrics, geriatrics, sports medicine, and consulting to business and industry. She owned a private practice for 27 years in the Chicago area specializing in orthopedics and Pilates. 5 years ago, Deb and her husband “semi-retired” to Evergreen, Colorado where she works part-time for a hospice and home-care agency, sees private patients as well as Pilates clients in her home studio and teaches Osteoporosis courses for Herman & Wallace. In her spare time, she skis and is busy checking off her Bucket List of visiting every national park in the country- currently 46 out of 63 and counting.
Deb Gulbrandson, DPT (she/her) has been a physical therapist for over 49 years with experience in acute care, home health, pediatrics, geriatrics, sports medicine, and consulting to business and industry. She owned a private practice for 27 years in the Chicago area specializing in orthopedics and Pilates. 5 years ago, Deb and her husband “semi-retired” to Evergreen, Colorado where she works part-time for a hospice and home-care agency, sees private patients as well as Pilates clients in her home studio and teaches Osteoporosis courses for Herman & Wallace. In her spare time, she skis and is busy checking off her Bucket List of visiting every national park in the country- currently 46 out of 63 and counting.
Deb is a graduate of Indiana University and a former NCAA athlete, where she competed on the IU Gymnastics team. She has always been interested in movement and function and is grateful to combine her skills as a PT and Pilates instructor. She has been certified through Polestar Pilates since 2005, a Certified Osteoporosis Exercise Specialist through the Meeks Method since 2008, and a Certified Exercise Expert for the Aging Adult through the Geriatric Section of the APTA.
Ask anyone on the street what one should do for osteoporosis and the typical answer is weight-bearing exercises - and they would be partially right. Weight-bearing, or loading, activities have been shown to increase bone density.(1) But that’s not the whole story. Different exercises have different strain magnitudes, strain rates, and strain frequencies - all of which impact bone density.
- Strain Magnitude - the force or impact of the exercise. Exercises such as gymnastics and weightlifting have a high strain magnitude.
- Strain Rate - the rate of impact of the exercise. Exercises such as jumping or plyometrics have a high strain rate.
- Strain Frequency - the frequency of impact during the exercise session. Exercises such as running have a high strain frequency.
When considering weight-bearing exercises for a home exercise program, the million-dollar question is, “How much weight-bearing is enough to stimulate bone growth, and how much is too much to compromise bone at risk for a fracture?” We know that there are incidents of individuals fracturing from just their body weight upon standing. Recently patients have been asking about heel drops and stomping, and whether they should do them. One size does not fit all.
An alternative is to focus on odd impact loading. A study by Nikander et a (2) targeted female athletes in a variety of sports classified by the type of loading they apparently produce at the hip region; that is, high-impact loading (volleyball, hurdling), odd-impact loading (squash-playing, soccer, speed-skating, step aerobics), high magnitude loading (weightlifting), low-impact loading (orienteering, cross-country skiing), and non-impact loading (swimming, cycling). The results showed that high impact and odd impact loading sports were associated with the highest bone mineral density.
Marques et al found that odd impact has the potential for preserving bone mass density as does high impact in older women in their 2011 study (3). Activities such as side stepping, figure eights, backward walking, and walking in square patterns help “surprise the bones” due to the different angles of muscular pull on the hip. The benefit, according to Nikander, is that we can get the same osteogenic benefits with less force, moderate versus high impact. This type of bone training would offer a feasible basis for targeted exercise-based prevention of hip fragility.
I tell my osteoporosis patients that if they walk or run the same route, the same distance, and the same speed that they are not maximizing the osteogenic benefits of weight bearing. Providing variety to the bones creates increased bone mass in the femoral neck and lumbar spine.(4)
Dancing is another great activity that combines forward, side, backward, and diagonal motions to movement. In addition, it adds music to make the “weight-bearing exercises” more fun. Due to balance and fall risk, many senior exercise classes offer Chair exercise to music. Unfortunately sitting is the most compressive position for the spine and is particularly problematic with osteoporosis patients. Also, the hips do not get any weight-bearing benefit. Whenever safely possible, have patients stand; you can position two kitchen chairs on either side, much like parallel bars, to hold on to while they “dance.”
Providing creativity in weight-bearing activities using odd impact allows not only for fun and stimulation and offers more “bang for the buck!”
Build on your knowledge of osteoporosis management by joining Deb Gulbrandson and Frank Ciuba in their upcoming short course Osteoporosis Management scheduled for January 25! Not only will you gain a deeper understanding of the scope of the problems, and specific tests for patients with osteoporosis, but you will also learn skills for evaluating patients as well as appropriate safe exercises for an Osteoporosis program.
Resources:
- Mosekilde L. Age-related changes in bone mass, structure, and strength--effects of loading. Z Rheumatol (2000); 59 Suppl 1:1-9.
- Nikander et al. Targeted exercises against hip fragility. Osteoporosis International (2009)
- Marques et al. Exercise effects on bone mineral density in older adults: a meta-analysis of randomized controlled trials. Epub 2011 Sep 16
- Weidauer L. et al. Odd-impact loading results in increased cortical area and moments of inertia in collegiate athletes. Eur J Appl Physiol (2014)
- Benedetti MG, Furlini G, Zati A, Letizia Mauro G. The Effectiveness of Physical Exercise on Bone Density in Osteoporotic Patients. Biomed Res Int. 2018 Dec 23;2018:4840531. doi: 10.1155/2018/4840531. PMID: 30671455; PMCID: PMC6323511.
AUTHOR BIO:
Deb Gulbrandson, PT, DPT
 Deb Gulbrandson, DPT has been a physical therapist for over 49 years with experience in acute care, home health, pediatrics, geriatrics, sports medicine, and consulting to business and industry. She owned a private practice for 27 years in the Chicago area specializing in orthopedics and Pilates. 5 years ago, Deb and her husband “semi-retired” to Evergreen, Colorado where she works part-time for a hospice and home-care agency, sees private patients as well as Pilates clients in her home studio and teaches Osteoporosis courses for Herman & Wallace. In her spare time, she skis and is busy checking off her Bucket List of visiting every national park in the country- currently 46 out of 63 and counting.
Deb Gulbrandson, DPT has been a physical therapist for over 49 years with experience in acute care, home health, pediatrics, geriatrics, sports medicine, and consulting to business and industry. She owned a private practice for 27 years in the Chicago area specializing in orthopedics and Pilates. 5 years ago, Deb and her husband “semi-retired” to Evergreen, Colorado where she works part-time for a hospice and home-care agency, sees private patients as well as Pilates clients in her home studio and teaches Osteoporosis courses for Herman & Wallace. In her spare time, she skis and is busy checking off her Bucket List of visiting every national park in the country- currently 46 out of 63 and counting.
Deb is a graduate of Indiana University and a former NCAA athlete where she competed on the IU Gymnastics team. She has always been interested in movement and function and is grateful to combine her skills as a PT and Pilates instructor. She has been certified through Polestar Pilates since 2005, a Certified Osteoporosis Exercise Specialist through the Meeks Method since 2008, and a Certified Exercise Expert for the Aging Adult through the Geriatric Section of the APTA.
When thinking of the Developmental Sequence (Supine, Side-lying, Prone, Quadruped, Tall Kneeling, Half-kneeling, Standing, and Walking), I used to think of either pediatrics or people with strokes. However, the developmental sequence can be very useful from an orthopedic standpoint specifically with osteoporosis patients.
We know that sitting is the most compressive position for our spines, yet repeatedly, I see physical therapists start exercise programs in sitting. There are several reasons I’d like you to consider starting patients in supine.
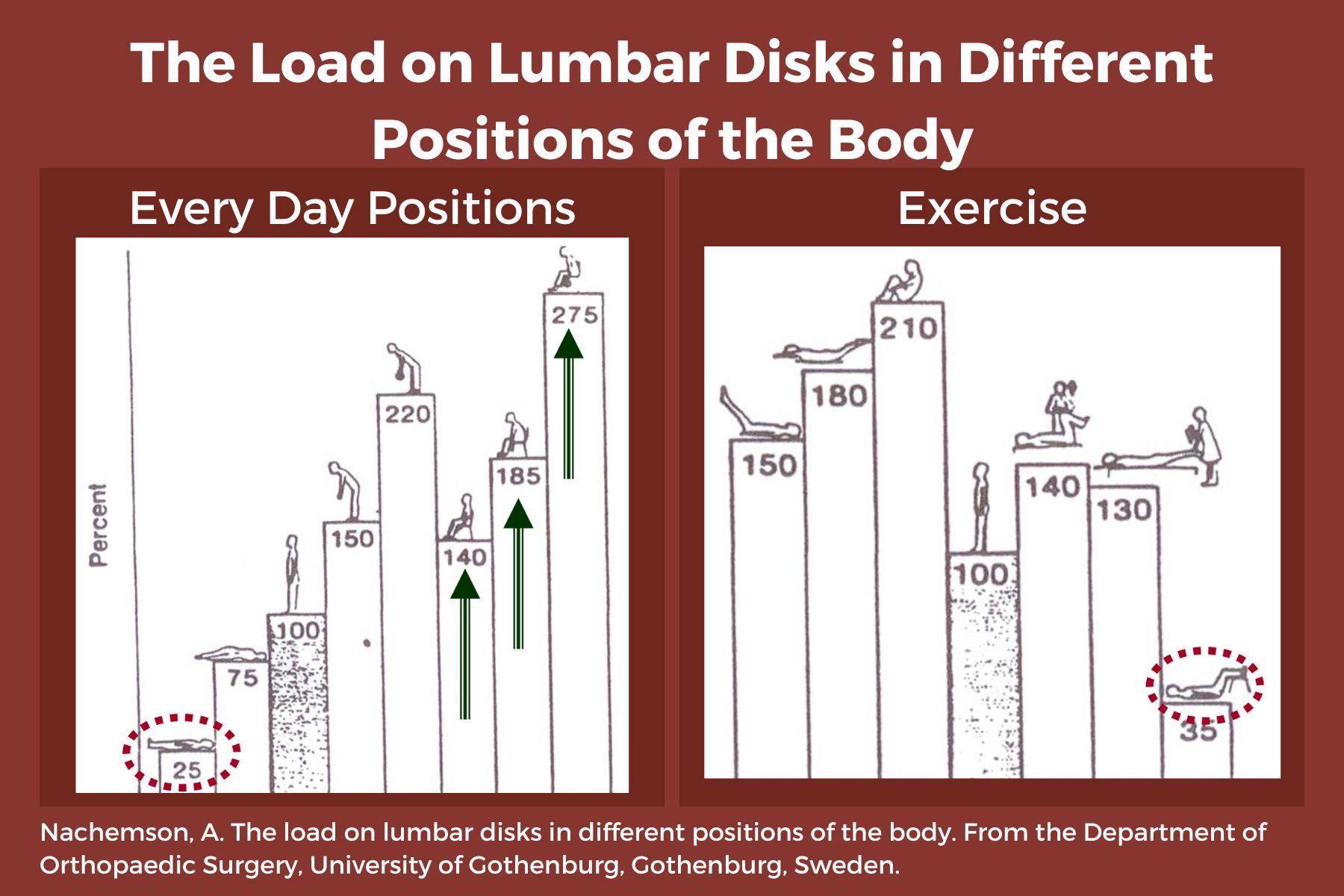
- Sitting increases intradiscal pressure. (1)
- Supine is a restful position, allowing tense muscles to relax, and can be a great way to reduce anxiety and cortisol running through the body. Ensure that the patient is propped with knees flexed or pillows under the knees, and forearms supported if there is tightness in the biceps.
- Patients can now concentrate on their breath, become aware of any “holding patterns” of tension throughout their body, and free up the mind to focus on learning new skills.
- When we are in higher levels of positioning-sitting, standing, or walking, our brain is focused on survival such as “not falling”. We have many more muscles and joints to control - ankles, knees, hips, etc. This reduces our ability to focus on learning new skills such as engaging the core muscles, relaxing the neck, stop clenching the fingers, etc.
- Preparation is key. We must help our patients gain mastery at one level and then move to the next. Once a patient can understand and find a neutral spine in prone, they are ready to move to side-lying.
- Side-lying can be very beneficial in teaching neutral spine because side-lying is “discombobulating.” We get lost in space and default to the fetal position - a flexed, contra-indicated posture for people with osteoporosis. Use a dowel rod or broom handle to provide feedback from the occiput to the mid-thoracic spine to the sacrum. Have your patient straighten their knees and hips so that, “If you were lying with your back against an imaginary wall, the back of your head, upper back, sacrum, and heels would touch the wall.”
- Prone: Not every osteoporosis patient you see will be able to ultimately transition to prone, but a high majority can and should. Again, propping is critical to allow any anatomical limitations such as shoulder tightness. Use a pillow longitudinally rather than transversely across the abdomen to elevate the shoulders so they can flex to allow the forehead on the hands. If not, keep arms by their side and provide a towel roll under the forehead. This position requires several “stages” of advancement over time and education to engage transversus abdominus, especially for those with spinal stenosis and/or tight hip flexors. The feet should be off the edge of the bed to allow for tightness in plantarflexion.
Working with patients in these three basic positions, while focusing on intercostal breathing, muscle relaxation of the neck, fingers, and other compensatory patterns as we move up the chain, builds a foundation to prepare for functional activities of sit-to-stand, static standing, and movement. These are not stepping stones to be skipped in order to jump into the higher-level functional activities. You would not build a house without a firm foundation. Make sure your patient has the building blocks necessary for the best possible outcomes.
Please join Frank Ciuba and me for our upcoming remote course: Osteoporosis Management: An Introductory Course for Healthcare Professionals on Saturday, Nov 2, 2024. We will discuss osteoporosis-safe exercises, balance and gait activities, and additional ways to help your patients build a strong foundation for movement competence!
Reference:
- Comparison of In Vivo Intradiscal Pressure between Sitting and Standing in Human Lumbar Spine: A Systematic Review and Meta-Analysis. Journal ListLife (Basel) PMC8950176 Jia-Qi Li,1 Wai-Hang Kwong,1,* Yuk-Lam Chan,1 and Masato Kawabata2
AUTHOR BIO:
Deb Gulbrandson, PT, DPT
 Deb Gulbrandson, DPT has been a physical therapist for over 49 years with experience in acute care, home health, pediatrics, geriatrics, sports medicine, and consulting to business and industry. She owned a private practice for 27 years in the Chicago area specializing in orthopedics and Pilates. 5 years ago, Deb and her husband “semi-retired” to Evergreen, Colorado where she works part-time for a hospice and home-care agency, sees private patients as well as Pilates clients in her home studio and teaches Osteoporosis courses for Herman & Wallace. In her spare time, she skis and is busy checking off her Bucket List of visiting every national park in the country- currently 46 out of 63 and counting.
Deb Gulbrandson, DPT has been a physical therapist for over 49 years with experience in acute care, home health, pediatrics, geriatrics, sports medicine, and consulting to business and industry. She owned a private practice for 27 years in the Chicago area specializing in orthopedics and Pilates. 5 years ago, Deb and her husband “semi-retired” to Evergreen, Colorado where she works part-time for a hospice and home-care agency, sees private patients as well as Pilates clients in her home studio and teaches Osteoporosis courses for Herman & Wallace. In her spare time, she skis and is busy checking off her Bucket List of visiting every national park in the country- currently 46 out of 63 and counting.
Deb is a graduate of Indiana University and a former NCAA athlete where she competed on the IU Gymnastics team. She has always been interested in movement and function and is grateful to combine her skills as a PT and Pilates instructor. She has been certified through Polestar Pilates since 2005, a Certified Osteoporosis Exercise Specialist through the Meeks Method since 2008, and a Certified Exercise Expert for the Aging Adult through the Geriatric Section of the APTA.
When thinking of the Developmental Sequence (Supine, Side-lying, Prone, Quadruped, Tall Kneeling, Half-kneeling, Standing, and Walking), I used to think of either pediatrics or people with strokes. However, the developmental sequence can be very useful from an orthopedic standpoint specifically with osteoporosis patients.
We know that sitting is the most compressive position for our spines, yet repeatedly, I see physical therapists start exercise programs in sitting. There are several reasons I’d like you to consider starting patients in supine.
- Sitting increases intradiscal pressure. (1)
- It is a restful position, allowing tense muscles to relax, and can be a great way to reduce anxiety and cortisol running through the body. Ensure that the patient is propped with knees flexed or pillows under the knees, and forearms supported if there is tightness in the biceps.
- Patients can now concentrate on their breath, become aware of any “holding patterns” of tension throughout their body, and free up the mind to focus on learning new skills.
- When we are in higher levels of positioning-sitting, standing, or walking, our brain is focused on survival such as “not falling”. We have many more muscles and joints to control - ankles, knees, hips, etc. This reduces our ability to focus on learning new skills such as engaging the core muscles, relaxing the neck, stop clenching the fingers, etc.
- Preparation is key. We must help our patients gain mastery at one level and then move to the next. Once a patient can understand and find a neutral spine in prone, they are ready to move to side-lying.
- Side-lying can be very beneficial in teaching neutral spine because side-lying is “discombobulating.” We get lost in space and default to the fetal position - a flexed, contra-indicated posture for people with osteoporosis. Use a dowel rod or broom handle to provide feedback from the occiput to the mid-thoracic spine to the sacrum. Have your patient straighten their knees and hips so that, “If you were lying with your back against an imaginary wall, the back of your head, upper back, sacrum, and heels would touch the wall.”
- Prone: Not every osteoporosis patient you see will be able to ultimately transition to prone, but a high majority can and should. Again, propping is critical to allow any anatomical limitations such as shoulder tightness. Use a pillow longitudinally rather than transversely across the abdomen to elevate the shoulders so they can flex to allow the forehead on the hands. If not, keep arms by their side and provide a towel roll under the forehead. This position requires several “stages” of advancement over time and education to engage transversus abdominus, especially for those with spinal stenosis and/or tight hip flexors. The feet should be off the edge of the bed to allow for tightness in plantarflexion.
Working with patients in these three basic positions, while focusing on intercostal breathing, muscle relaxation of the neck, fingers, and other compensatory patterns as we move up the chain, builds a foundation to prepare for functional activities of sit-to-stand, static standing, and movement. These are not stepping stones to be skipped in order to jump into the higher-level functional activities. You would not build a house without a firm foundation. Make sure your patient has the building blocks necessary for the best possible outcomes.
Please join Frank Ciuba and me for our upcoming remote course: Osteoporosis Management: An Introductory Course for Healthcare Professionals on Saturday, Nov 2, 2024. We will discuss osteoporosis-safe exercises, balance and gait activities, and additional ways to help your patients build a strong foundation for movement competence!
Reference:
- Comparison of In Vivo Intradiscal Pressure between Sitting and Standing in Human Lumbar Spine: A Systematic Review and Meta-Analysis. Journal ListLife (Basel) PMC8950176 Jia-Qi Li,1 Wai-Hang Kwong,1,* Yuk-Lam Chan,1 and Masato Kawabata2
AUTHOR BIO:
Deb Gulbrandson, PT, DPT
 Deb Gulbrandson, DPT has been a physical therapist for over 49 years with experience in acute care, home health, pediatrics, geriatrics, sports medicine, and consulting to business and industry. She owned a private practice for 27 years in the Chicago area specializing in orthopedics and Pilates. 5 years ago, Deb and her husband “semi-retired” to Evergreen, Colorado where she works part-time for a hospice and home-care agency, sees private patients as well as Pilates clients in her home studio and teaches Osteoporosis courses for Herman & Wallace. In her spare time, she skis and is busy checking off her Bucket List of visiting every national park in the country- currently 46 out of 63 and counting.
Deb Gulbrandson, DPT has been a physical therapist for over 49 years with experience in acute care, home health, pediatrics, geriatrics, sports medicine, and consulting to business and industry. She owned a private practice for 27 years in the Chicago area specializing in orthopedics and Pilates. 5 years ago, Deb and her husband “semi-retired” to Evergreen, Colorado where she works part-time for a hospice and home-care agency, sees private patients as well as Pilates clients in her home studio and teaches Osteoporosis courses for Herman & Wallace. In her spare time, she skis and is busy checking off her Bucket List of visiting every national park in the country- currently 46 out of 63 and counting.
Deb is a graduate of Indiana University and a former NCAA athlete where she competed on the IU Gymnastics team. She has always been interested in movement and function and is grateful to combine her skills as a PT and Pilates instructor. She has been certified through Polestar Pilates since 2005, a Certified Osteoporosis Exercise Specialist through the Meeks Method since 2008, and a Certified Exercise Expert for the Aging Adult through the Geriatric Section of the APTA.

Movement competence (or Movement Literacy) is defined as the development of sufficient skills to ensure successful performance in different physical activities. Often used in the world of sports and youth, it also applies to our everyday activities. For example, standing up from a chair or toilet, getting in/out of a car, moving our body from Point A to Point B (and the difference between the ground being even and dry vs uneven and icy).
In our course, Osteoporosis Management: An Introductory Course for Healthcare Professionals, Dr Frank Ciuba and I approach the starting point for individuals with low bone mass (osteopenia or osteoporosis), from an “optimal alignment position.” Patients start supine with hips and knees flexed and are educated on what optimal alignment feels like. Many need to be propped using pillows, towels, or blocks behind their heads, forearms, or between their knees to achieve “their optimal alignment.” Breathing and awareness play a huge role in activating core musculature to sustain this alignment when moving to a vertical position such as sitting or standing. In vertical, our weight-bearing forces and gravity should pass down through the skeleton to take advantage of bone-building benefits. We use dowel rods, broom handles, and walls to give feedback. Optimal alignment can and should be taught in a variety of positions: side-lying, prone, hands and knees, ½ kneeling as we move up the developmental chain.
Hip Hinging, a well-known concept by therapists, must be practiced and mastered for patients with low bone mass to reduce the risk of vertebral fractures. Activities that involve bending at the waist such as brushing teeth, making a bed, and putting dishes in the dishwasher all place the anterior portion of the vertebral bodies under pressure and increase fracture risk.
Advancing from static optimal alignment postures to dynamic optimal alignment is a whole different ballgame; akin to advancing from sitting in a car to driving a car. There are many moving parts - pun intended.
Just as in athletics, mastery comes from repetition. It is not enough to teach patients a safe movement pattern one time, hand them a sheet of paper with pictures, and expect them to be able to comply and gain competence. Reinforcing proper technique and helping them become aware of compensation strategies (hunching shoulders when lifting objects, overarching the back when reaching overhead, etc.) are critical if Movement Competency is to “stick.”
I like to think of movement competency as building a house. First, you need a firm foundation before putting up the walls and roof. Our patients require that foundation to be able to layer on more complicated patterns of movement.
Please join us for this one-day course on September 14th or November 2nd to learn more Osteoporosis-safe exercises, balance and gait activities, and additional ways to help your patients build a strong foundation for movement competence!
AUTHOR BIO:
Deb Gulbrandson, PT, DPT
 Deb Gulbrandson, DPT has been a physical therapist for over 49 years with experience in acute care, home health, pediatrics, geriatrics, sports medicine, and consulting to business and industry. She owned a private practice for 27 years in the Chicago area specializing in orthopedics and Pilates. 5 years ago, Deb and her husband “semi-retired” to Evergreen, Colorado where she works part-time for a hospice and home-care agency, sees private patients as well as Pilates clients in her home studio and teaches Osteoporosis courses for Herman & Wallace. In her spare time, she skis and is busy checking off her Bucket List of visiting every national park in the country- currently 46 out of 63 and counting.
Deb Gulbrandson, DPT has been a physical therapist for over 49 years with experience in acute care, home health, pediatrics, geriatrics, sports medicine, and consulting to business and industry. She owned a private practice for 27 years in the Chicago area specializing in orthopedics and Pilates. 5 years ago, Deb and her husband “semi-retired” to Evergreen, Colorado where she works part-time for a hospice and home-care agency, sees private patients as well as Pilates clients in her home studio and teaches Osteoporosis courses for Herman & Wallace. In her spare time, she skis and is busy checking off her Bucket List of visiting every national park in the country- currently 46 out of 63 and counting.
Deb is a graduate of Indiana University and a former NCAA athlete where she competed on the IU Gymnastics team. She has always been interested in movement and function and is grateful to combine her skills as a PT and Pilates instructor. She has been certified through Polestar Pilates since 2005, a Certified Osteoporosis Exercise Specialist through the Meeks Method since 2008, and a Certified Exercise Expert for the Aging Adult through the Geriatric Section of the APTA.
An interview with Frank Ciuba.
Frank Ciuba, co-instructor of Osteoporosis Management< alongside Deb Gulbrandson, explains that practitioners need the information provided in their course. "This course is the latest up-to-date research compiled by my partner Deb Gulbrandson and myself in the management of osteoporosis for clinicians." He shares that similar to learning about the pelvic floor, "when physical therapists go to school they get only a small amount of what osteoporosis is and very little on how to treat a patient."
Frank explains that he became interested in teaching osteoporosis management when he learned "that one in four men statistically will get osteoporosis or an osteoporosis-related fracture in their lifetime and they're really not being identified." Osteoporosis Management provides an exercise-oriented approach to treating these patients and it covers specific tests for evaluation, appropriate safe exercises and dosing, basic nutrition, and ideas for marketing your osteoporosis program.
In pelvic health rehabilitation, it's seen that osteoporosis-related kyphosis (curvature of the spine) can affect pelvic organ prolapse, breathing, and digestion. Patients who go through the osteoporosis management program with Frank and Deb, are shown that they reduce the likelihood of compression fracture by 80%.
This course, Osteoporosis Management, is not just for practitioners working with osteoporosis or osteopenia patients. Frank lists the types of patients he's been able to help. "I've used this on high school backpack syndrome, whiplash injuries, adhesive capsulitis, spinal stenosis, low back pain, lumbar strain, even some hip pathologies." He concludes with "We just need to get the word out to more individuals that this a program that can help them. Not only in the short term, but in the long term. This is a program for life."
Holly Tanner Short Interview Series - Episode 2 featuring Deb Gulbrandson
Holly Tanner and Deb Gulbrandson sat down to discuss the Osteoporosis Management Remote Course and why it is important for practitioners to recognize and know how to safely treat and manage osteoporosis patients in their practices.
Deb Gulbrandson shares the goal of the Osteoporosis Management remote course: "This course is based on the Meeks Method created by Sara Meeks, PT, MS, GCS...we have branched out to add information on sleep hygiene, exercise dosing, and basic nutrition for a person with low bone mass. Knowing how to recognize signs, screen for osteoporosis, and design an effective and safe program can be life-changing for these patients."
Join H&W at the Osteoporosis Management remote course, scheduled for September 18-19, 2021, to learn more about treating patients with osteoporosis.

Osteoporosis is known to be a painless, progressive condition that leads to a weakening of the bones and can lead to a higher risk for broken bones. The upcoming remote course, Osteoporosis Management, scheduled for September 18-19, 2021, will discuss the scope of problems, specific tests for evaluating patients, appropriate safe exercises and dosing, and basic nutrition.
H&W faculty member Deb Gulbrandson recommends using the National Osteoporosis Foundation database for a resource and emphasizes the prevalence of osteoporosis is in a past interview for the Pelvic Rehab Report. "Approximately 1 in 2 women over the age of 50 will suffer a fragility fracture in their lifetime...According to the US Census Bureau, there are 72 million baby boomers (age 51-72) in 2019. Currently, over 10 million Americans have osteoporosis and 44 million have low bone mass."
A well-known consequence of osteoporosis is the increased risk of fragility fractures. A fragility fracture is often the first sign of osteoporosis and can be the cause of pain, disability, and quality of life for the patient. Research by Marsha van Oostwaard provided data that suggests about 13 percent of men and 40 percent of women with osteoporosis will experience a fragility fracture in their lifetime. Men also have a higher rate of mortality from fragility fractures relative to women (1).
The International Osteoporosis Foundation reports that patients who have suffered from a fragility fracture are at a high risk of experiencing secondary fractures, especially within two years of the initial fracture. Fragility fractures can result in osteoporotic patients from events that would not elicit an injury in a healthy adult. These events can include falling from a standing position and other low-energy traumas.
Fragility fractures are characterized by low bone mineral density and have an increased incidence with age (2). The risk of a fragility fracture is also influenced by bone geometry and microstructure. The most serious fracture sites are at the hip and vertebrae, but fractures can occur also on the ribs and other locations. Healthcare practitioners can assist patients in adapting lifestyle factors including exercise, sleep positions, and nutrition with the aim of helping prevent falls from occurring.
Deb Gulbrandson shares the goal of the Osteoporosis Management remote course: "This course is based on the Meeks Method created by Sara Meeks, PT, MS, GCS...we have branched out to add information on sleep hygiene, exercise dosing, and basic nutrition for a person with low bone mass. Knowing how to recognize signs, screen for osteoporosis, and design an effective and safe program can be life-changing for these patients."
Join H&W at the Osteoporosis Management remote course, scheduled for September 18-19, 2021, to learn more about treating patients with osteoporosis.
- Fragility Fracture Nursing: Holistic Care and Management of the Orthogeriatric Patient [Internet]. Marsha van Oostwaard. Hertz K, Santy-Tomlinson J. Springer; 2018.
- The burden of osteoporotic fractures: a method for setting intervention thresholds. Kanis, J.A., et al. Osteoporos Int, 2001. 12(5): p. 417-27.
Deb Gulbrandson, PT, DPT, along with Frank J Ciuba DPT, MS, is the author and instructor for a new course on osteoporisis that is launching remotely this month. Join Deb in Osteoporosis Management: A Comprehensive Approach for Healthcare Professionals!
Osteoporosis is a disease of increasingly porous bones that are at greater risk for fracture. The normal “bone remodeling” of breaking down and building up bone as we age is out of balance. Similar to a bank account with withdrawals outpacing deposits, as time goes on there is more breaking down than building back up. This leaves the bone more vulnerable for fracture.
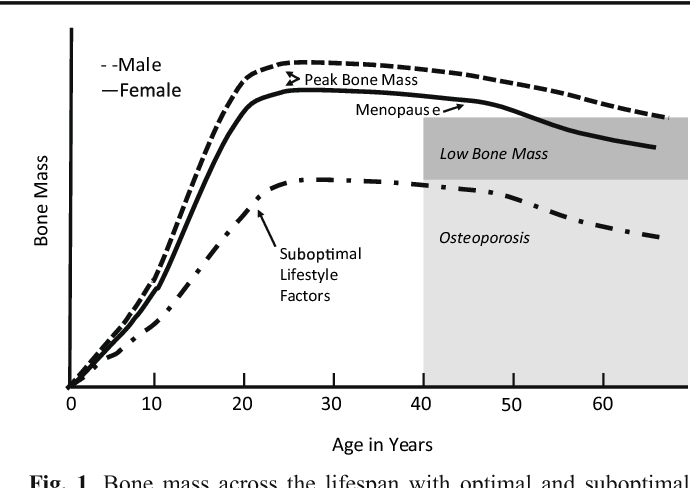
We tend to think of Osteoporosis as an old person’s disease and in fact age is certainly a risk factor. We see a sharp decline in bone density the first few years following menopause; a withdrawal from the “bone bank account.” But let me share a startling statistic. At the age of 20 we have 98% of the bone density we will ever achieve. We achieve Peak Bone Mass by age thirty when our bones have reached their maximum strength and density.
Factors affecting Peak Bone Mass include both Non-modifiable and Modifiable. Among the non-modifiable factors are gender (peak bone mass is higher in men), race (peak bone mass is higher in African Americans), and hormonal factors (early onset of menstruation and use of oral contraceptives tend to have higher peak bone mass). A family history of osteoporosis is another important factor.
Modifiable factors include nutrition (adequate calcium in the diets of young people), physical activity during the early years (specifically weight bearing and resistance exercises). Poor lifestyle behaviors (smoking, high alcohol intake, and sedentary lifestyle) have all been linked to low bone density in adolescents.
The American Physical Therapy Association website includes a section on “Container Baby Syndrome” (CBS). CBS is the name used to describe a range of physical, cognitive, and developmental conditions caused by a baby or infant spending too much time in containers such as baby carriers, strollers, and Bumpo seats. Bone mass can certainly be affected by reduced movement and weight bearing activities. Due to the SIDS scare, many young parents are fearful of allowing their children to spend time on their abdomens. Educate and share the “Supine to Sleep, Prone to Play” mantra.
The graph below shows a comparison of the Peak Bone Mass of males to females and to individuals with suboptimal lifestyle factors. You can see that the suboptimal group never catches up and enters the osteoporosis stage at around age 40.
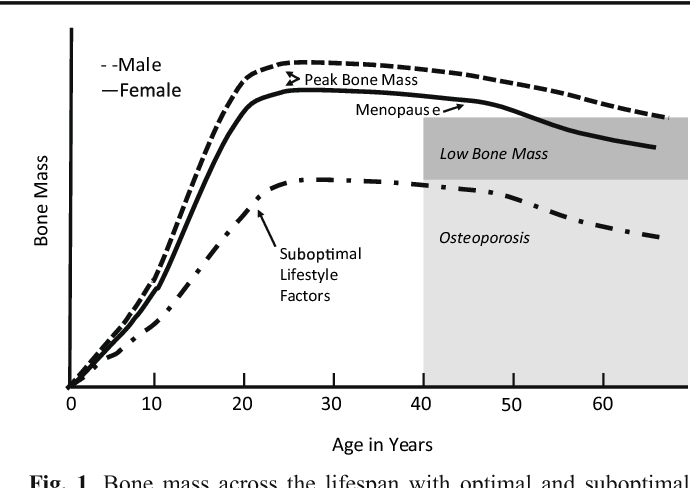
According to the Department of Human Services “Osteoporosis is a pediatric disease with geriatric consequences. Peak bone mass is built during our first three decades. Failure to build strong bones during childhood and adolescent years manifests in fractures later in life.”
What can we do?
• Start early: Encourage young children (and their parents) to move more and sit less.
• Spread the word: Speak to Young Mothers’ Clubs, Girl Scout Troops; anywhere to influence adolescent and teens about the importance of proper exercise and good nutrition.
• Write a blog: Share this information in newspapers, social media, and on your website. Get the word out! Because the bones of our future generation depend on it.
NIH Osteoporosis and Related Bone Diseases National Resource Center
Department of Human Services
American Physical Therapy Association
Deb Gulbrandson, PT, DPT is teaming up with Frank J Ciuba DPT, MS to create a new course called Osteoporosis Management: A Comprehensive Approach for Healthcare Professionals! This new course is launching remotely this July 25-26, 2020, and it emphasizes visual imagery cues which leads to enhanced performance for patients. Both course authors are trained by Sara Meeks, and have adapted her method to create this updated, evidence-based course on osteoporosis management.
How many times have you told your patients to stand up straight and stop looking down while walking? How’d that work out? Probably not so good. At best you may have noticed a temporary correction only for the patient to return to the formerly mentioned poor posture. We know that balance is affected by alignment of our trunk and spine. 1 Everyone needs to avoid falls but it’s particularly important with osteoporosis patients due to bone fragility.
 We want our patients not only to move, but to move with optimal alignment. According to Fritz, et al 2 in the vhitepaper: “Walking Speed: The Sixth Vital Sign”, walking is a complex functional activity. Our ability to influence motor control, muscle performance, sensory and perceptual function, endurance and habitual activity level can result in a more efficient and safer gait.
We want our patients not only to move, but to move with optimal alignment. According to Fritz, et al 2 in the vhitepaper: “Walking Speed: The Sixth Vital Sign”, walking is a complex functional activity. Our ability to influence motor control, muscle performance, sensory and perceptual function, endurance and habitual activity level can result in a more efficient and safer gait.
Visual imagery cuing had been popular in the sports world for decades. By changing one or two words, physical performance has been shown to improve. 3 In a study involving standing long jump, Wu et al instructed undergraduate students to either “Jump as far as you can and think about extending your legs” (internal focus) or “Jump as far as you can and think about jumping as close to the green target as possible” (external focus). The external focus group jumped 10% farther. Lohse et al 4 and Zachry et al 5 surmised that an external focus reduces the "noise" in the motor system which affects muscular tension and optimal function.
It Starts with Posture
Before you can expect your patients to walk well, they have to stand well- stability before mobility. Assess their posture from all angles and determine where to start. One visual image may change a host of problems. A common postural fault, “slumping” is seen as forward head, increased thoracic kyphosis accompanied with either lumbar hyper or hypo lordosis. Your goal is to get the optimal alignment image that you have in your mind……. into their body.
Most people think in pictures rather than words. 6 Yet the medical industry uses words to communicate. Often we say, “Don’t slouch. Don’t look down.” Telling your patient what not to do is not helpful. Our brain hears the words, “Slouch or look down.” We don’t discern the negative. If I say to you, “Don’t think of a pink elephant,” what does your mind see? How can you not see a pink elephant?
Below are five common visual cues to improve a patient’s posture in standing and walking. These tend to follow the Pareto Principle. 20% of your cues work 80% of the time.
- “In standing, imagine a bungee cord running from the top of your head to the ceiling. Visualize a mother cat lifting her kitten up by the scruff of the neck.”
- “When breathing, imagine an umbrella inside your ribcage, opening up upon inhale, and closing on exhale. Breathe in all directions including into the back of your lungs as if you were filling up the sails of a sailboat.”
- “When walking, widen your collarbones as if they were arrows, shooting off the tips of your shoulders. Imagine your head is a floating balloon, gliding along above your shoulders.”
- “Pretend you are the King (or Queen) of England as you walk among your subjects. “
- “Slide your shoulder blades down toward your opposite hip pockets.”
Choose a cue and instruct your patient. Observe changes in posture, alignment, efficiency of movement, or length of step during gait. Ask your patient for feedback. “What did you notice?” Certain cues resonate more than others. Give them variety and options. The best cues are the ones they create themselves. When a patient says, “You mean like………..?” you know it’s a great cue for them. They have an intuitive understanding and relate to it which translates into their body. A patient’s response to the bungee cord cue was, “You mean like a Christmas ornament hanging from the tree?” My response? Absolutely!
While some visual cues may seem too flowery or not “medical” enough, the research is solid the impact powerful. Plus your patients love it! Visual cues are sticky. They help remind us when we’re out in the real world. Isn’t that the ultimate goal – helping patients become independent in their pursuit of health and safety?
1. Shiro Imagam, et all. Influence of spinal sagittal alignment, body balance, muscle strength, and physical ability on falling of middle-aged and elderly males. Eur Spine J. 2013 Jun;
2. Fritz S. et al White Paper: “Walking Speed: The Sixth Vital Sign” J Geriatr Phys Ther. 2009
3. Wu, et al Effect of Attentional Focus Strategies on Peak Force and Performance in the Standing Long Jump. Joun of Strength and Conditioning Research 2012
4. Lohse and Sherwood Defining the Focus of Attention: Effects of Attention on Perceived Exertion and Fatigue
5. Zachry, T et al. Increased Movement Accuracy and Reduced EMG Activity as a Result of Adopting an External Focus of Attention. Brain Research Bulletin Oct 2005
6. Dynamic Alignment Through Imagery. Franklin, Eric. Second Edition, 2012