The first time I experienced the effects of Post-Traumatic Stress Disorder (PTSD) was when my patient dissociated during a treatment session and relived the rape that had occurred when she was ten years old. It was devastating. I didn’t know what to do. She was unresponsive to my intervention. Her eyes didn’t see me, alternating between wide-eyed, horrified panic and clenched-closed, lip biting excruciating pain. It was my late night and I was alone in the clinic. I sat helplessly next to my sweet patient hoping and praying that her torture would end quickly. When she finally stopped writhing, she slept. Deep and hard. Finally she woke up disoriented and scared. She grabbed her things and left. For me, this experience was my initiation into the world of trauma.
 Approximately 5-6 % of men and 10-12% of women will suffer from PTSD at some point in their lives. Researchers believe that 10% of people exposed to trauma will go on to develop PTSD. The expression of PTSD symptoms can present differently in men and women. Men may have more externalizing disorders progressing along a scale that includes vigilance, resistance, defiance, aggression and homicidal thoughts. Women tend to present with internalizing disorders such as depression, anxiety, exaggerated startle responses, dissociation, and suicidal thoughts. The research is clear that both men and women with PTSD display changes in brain function. The mid brain (amygdala, basal ganglia and hippocampus) tends to be overactive in sounding alarm signals while the prefrontal cortex fails to turn off the mid brain when a threat is no longer present. Since the prefrontal cortex is not always functioning correctly, traditional talk therapy may not be as effective for treating PTSD. Instead, say many researchers, breath and movement exercises may help regulate brain functioning. Yoga, Tai Chi, and meditation have been shown to have a positive impact on down regulating the mid brain and improving cerebral output. As pelvic floor therapists we deal with trauma on a daily basis, whether we know it or not. Although we are not trained in psychology, understanding PTSD and equipping ourselves with tools to support our patients is imperative for both our patients and ourselves.
Approximately 5-6 % of men and 10-12% of women will suffer from PTSD at some point in their lives. Researchers believe that 10% of people exposed to trauma will go on to develop PTSD. The expression of PTSD symptoms can present differently in men and women. Men may have more externalizing disorders progressing along a scale that includes vigilance, resistance, defiance, aggression and homicidal thoughts. Women tend to present with internalizing disorders such as depression, anxiety, exaggerated startle responses, dissociation, and suicidal thoughts. The research is clear that both men and women with PTSD display changes in brain function. The mid brain (amygdala, basal ganglia and hippocampus) tends to be overactive in sounding alarm signals while the prefrontal cortex fails to turn off the mid brain when a threat is no longer present. Since the prefrontal cortex is not always functioning correctly, traditional talk therapy may not be as effective for treating PTSD. Instead, say many researchers, breath and movement exercises may help regulate brain functioning. Yoga, Tai Chi, and meditation have been shown to have a positive impact on down regulating the mid brain and improving cerebral output. As pelvic floor therapists we deal with trauma on a daily basis, whether we know it or not. Although we are not trained in psychology, understanding PTSD and equipping ourselves with tools to support our patients is imperative for both our patients and ourselves.
You might be wondering what happened after that frightful night in the clinic? My patient was determined to get better. She had a non-relaxing pelvic floor. She was a teacher and was plagued by urinary distress. She either had terrible urgency or would go for hours and not be able to empty her bladder. So we met with her therapist to learn strategies to help us to be able to work together without triggering dissociation. It was a slow road, but the three of us working together helped my patient not only reach her goals but to be able to be skillful enough to maintain her gains using a dilator for self-treatment.
If you would like to learn more about PTSD, meditation, yoga, chronic pain, psychologically informed practice and self-care for patients and providers please join Nari Clemons and I in Tampa in January as we present a new offering for Herman and Wallace, “Holistic Intervention and Meditation.” We would love to see you there.
Bremner, J. D. (2006). Traumatic stress: effects on the brain. Dialogues in clinical neuroscience, 8(4), 445-461.
Kerr, C. E., Jones, S. R., Wan, Q., Pritchett, D. L., Wasserman, R. H., Wexler, A., ... & Littenberg, R. (2011). Effects of mindfulness meditation training on anticipatory alpha modulation in primary somatosensory cortex. Brain research bulletin, 85(3), 96-103.
Morasco, B. J., Lovejoy, T. I., Lu, M., Turk, D. C., Lewis, L., & Dobscha, S. K. (2013). The relationship between PTSD and chronic pain: mediating role of coping strategies and depression. Pain, 154(4), 609-616.
Olff, M., Langeland, W., & Gersons, B. P. (2005). The psychobiology of PTSD: coping with trauma. Psychoneuroendocrinology, 30(10), 974-982.
The Role Of Yoga In Healing Trauma
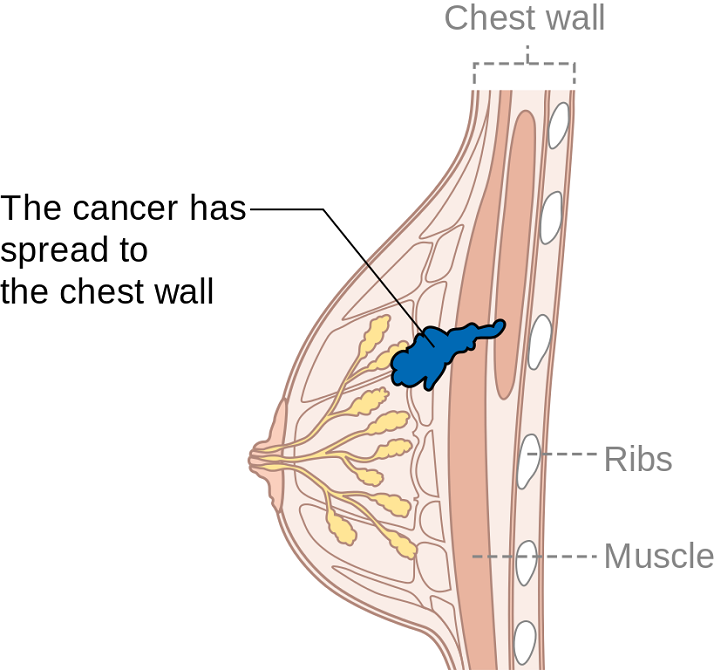
Summer can make women cringe at the thought of baring most of their bodies yet finding just the right coverage for their breasts. Some scrounge for padded tops to pump up their actual A cup. Some seek the greatest amount of coverage to support every ounce of skin. And still others search for flattering tops to accentuate cleavage and minimize tan lines. Just like one swimsuit does not fit every woman, only one aspect of post-breast cancer rehab is not generally sufficient. A combination of exercise, mindfulness, and myofascial release may need to be implemented for optimal recovery.
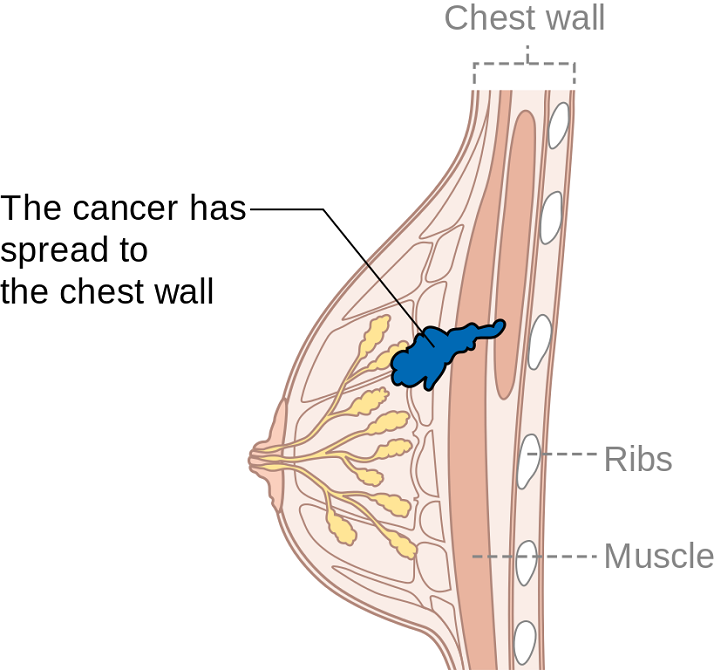
Ibrahim et al., (2017) produced a pilot randomized controlled trial considering the effects of specific exercise on upper limb function and ability to return to work after radiotherapy for breast oncology. The study involved 59 young women divided into an exercise group or a control group that received standard care. The Disability of Arm, Shoulder, and Hand (DASH), the Metabolic Equivalent of Task-hours per week (MET-hours/week), and a post hoc questionnaire on return to work were all used and recorded over 6 time periods after the 12-week post-radiation targeted exercise program. Women who had a total mastectomy still had upper limb dysfunction, but no there was no statistically significant difference in DASH scores between groups. Both groups at 18 months had returned to their pre-illness activity levels, and 86% returned to work (at just 8.5 fewer hours/week). The authors concluded exercise alone does not change the long-term outcome of upper limb function post-radiation.
Mindfulness-based cognitive therapy (MBCT) for persistent pain in women after treatment for primary breast cancer was explored by Johannsen et al., in two 2017 articles, one concerned with clinical and psychological mediators and the other focused on cost-effectiveness. Each study included 129 women with persistent pain from breast cancer, placed in a MBCT group or a wait-list control group. The first study showed attachment avoidance was a statistically significant moderator, with subjects who had a higher attachment avoidance having lower pain intensity after MBCT. In the subjects undergoing radiotherapy, MBCT had a smaller effect on pain than those not having radiotherapy. The authors’ next study focused on the minimal clinically important difference (MCID) on pain intensity. Baseline and 6 months post-treatment data on healthcare utilization and pain medication were analyzed from national registries. The average total cost of the MBCT group was 730 euros less than the control group, and more women in the MBCT group had a MCID in pain than those in the control group.
DeGroef et al., (2017) performed a randomized controlled trial to assess the efficacy of myofascial techniques for breast cancer survivors who experienced upper limb dysfunctions. Fifty women post-unilateral breast cancer received either 12 sessions of standard physical therapy with myofascial therapy or 12 sessions of standard physical therapy plus a sham intervention during a 3-month period. After intervention, no significant differences between groups were found for active shoulder range of motion, lymphedema, handheld dynamometer strength, scapular statics and dynamics, shoulder function, or quality of life. The authors concluded shoulder ROM and function in both groups showed positive effects up to 1 year follow-up, but myofascial therapy provided no additional benefit in breast cancer patients.
Treatment for any patient should be individualized, based on deficits found clinically, whether they are physiological, anatomical, or psychological. Having a beach bag overflowing with techniques and tools, each ready to be used when the appropriate time comes, makes for a more competent therapist and a better rehabilitation outcome for patients. There simply is no “one size fits all” in breast oncology rehab.
YOU can be a major contributor to a breast cancer patients medical care team. Learn new skills by attending Physical Therapy Treatment for the Breast Oncology Patient this September in Boston, MA.
Ibrahim, M, Muanza, T, Smirnow, N, Sateren, W, Fournier, B, Kavan, P, Palumbo, M, Dalfen, R, Dalzell, MA. (2017). Time course of upper limb function and return-to-work post-radiotherapy in young adults with breast cancer: a pilot randomized control trial on effects of targeted exercise program. Journal of Cancer Survivorship: research and practice. http://doi:10.1007/s11764-017-0617-0
Johannsen, M, O'Toole, MS, O'Connor, M, Jensen, AB, Zachariae, R. (2017). Clinical and psychological moderators of the effect of mindfulness-based cognitive therapy on persistent pain in women treated for primary breast cancer - explorative analyses from a randomized controlled trial. Acta Oncology. 56(2):321-328. http://doi:10.1080/0284186X.2016.1268713
Johannsen, M, Sørensen, J, O'Connor, M, Jensen, AB, Zachariae, R. (2017). Mindfulness-based cognitive therapy (MBCT) is cost-effective compared to a wait-list control for persistent pain in women treated for primary breast cancer-Results from a randomized controlled trial. Psychooncology. http://doi:10.1002/pon.4450
De Groef,A, Van Kampen, M, Verlvoesem N, Dieltjens, E, Vos, L, De Vrieze, T, Christiaen, MR, Neven, P, Geraerts, I, Devoogdt, N. (2017). Effect of myofascial techniques for treatment of upper limb dysfunctions in breast cancer survivors: randomized controlled trial. Support Care Cancer. 25(7):2119-2127. http://doi:10.1007/s00520-017-3616-9
Preterm birth can have deleterious health effects not only for the child, but also for the mother. A child may be born so early that various health systems are not matured, leading to susceptibility and delay in development and growth. Maternal health may also be severely impacted, with conditions such as anxiety and psychological stress. Managing the prevention of a pre-term delivery can be stressful and challenging for a pregnant woman, and authors Ha & McDonald (2016) report that this issue is not well studied. A cross-sectional survey was completed to find out not only what a woman’s preferences and concerns are, but also to find out which recommendations were likely to be followed by the patient. This is important, the authors state, because women who are actively involved in medical decisions are more likely to feel satisfied with their childbirth experience.

The survey was completed by 311 women at a median of 32 weeks gestation. Mean age was 30.9, and the majority of them identified as European/White-Caucasian. Most of them were married or in a common-law relationship and had received some level of post-secondary education. The majority of women who were told they were at increased risk of preterm labor (PTL) preferred close-monitoring rather then PTL prevention. Of interest is that the majority of women reported they would use other sources of information besides their primary provider, with the most reported source being the internet or family and friends. This point begs the question of how high is the quality level or accuracy of the available information on the internet or in the general public? Common available options for prevention included progesterone, cerclage, and pessary use. If a woman is not interested in using recommended prevention strategies, the goal of the rehabilitation clinician should be to, on a constant basis, monitor for symptoms and signs of early labor, and encourage the patient to keep any recommended provider appointments, and stay in close contact with her provider so that close-monitoring may be carried out.
An additional goal for rehabilitation is to provide the mother with strategies that may assist her in managing her anxiety, stress, movement dysfunctions, sleep, and other activities. Prior research has validated the benefits of relaxation training in pre-term labor: a cost-effective, low risk and easily implemented strategy. Training women in such a tool during pregnancy fits well into the rehab provider’s scope, and can be instructed in the clinic (or home!) for home program implementation. Larger newborns, longer gestations, and higher rates of prolonged gestations have been recorded when using relaxation training training for pre-term labor.Janke et al., 1999) Chuang et al. (2012) have documented fewer admissions to neonatal intensive care unit, decreased rates of extreme pre-term birth, and shorter stays in hospital with use of relaxation training. Meditation, mindfulness, deep breathing, visualization, and movement within recommend medical limits may all be valuable tools that make up a part of a patient’s rehabilitation experience. In an article describing how prenatal meditation influences infant behaviors, yoga, singing, and massage therapy are all cited methods for improving maternal and/or fetal health.Chan, 2014
The Herman & Wallace Institute offers a three part series on pregnancy and postpartum. Get started by attending either Care of the Pregnant Patient or Care of the Postpartum Patient. You may also be interested in any of the Mindfulness & Meditation courses, including Holistic Interventions and Meditation, Mindfulness-Based Pain Treatment, and Mindfulness for Rehabilitation Professionals.
Chan, K. P. (2014). Prenatal meditation influences infant behaviors. Infant Behavior and Development, 37(4), 556-561.
Chuang, L.-L., Lin, L.-C., Cheng, P.-J., Chen, C.-H., Wu, S.-C., & Chang, C.-L. (2012). The effectiveness of a relaxation training program for women with preterm labour on pregnancy outcomes: A controlled clinical trial. [Article]. International Journal of Nursing Studies, 49, 257-264. doi: 10.1016/j.ijnurstu.2011.09.007
Ha, V., & McDonald, S. D. (2017). Pregnant women’s preferences for and concerns about preterm birth prevention: a cross-sectional survey. BMC pregnancy and childbirth, 17(1), 49.
Janke, J. (1999). The effect of relaxation therapy on preterm labor outcomes. Journal Of Obstetric, Gynecologic, And Neonatal Nursing: JOGNN / NAACOG, 28(3), 255-263.
“To me it felt like I was just sitting on bed rest, waiting to have a seizure, you know, waiting to start circling the drain.” “Every time I went to the doctor I had this…anxiety attack.” These are the words of pregnant women diagnosed with preeclampsia and on bed rest. Other phrases reported by the authors who interviewed women on bedrest included “…an impending doom…”, “…meltdown…”, “nervous wreck.” A few of the major themes that emerged in the interviews was that of negative thoughts and feelings, family stressors, and not being heard. And while using the term “crazy” is not truly appropriate, women who are forced to abruptly stop interacting and participating in their typical life activities must be regarded as being very high risk for more than just physical issues. Kehler et al., 2016
 In an ideal situation, bed rest during pregnancy is prescribed to help keep the mother and fetus healthy. Unfortunately, bed rest in itself is associated with potentially negative consequences in physical and mental health, and providers are not always up-to-date on changing recommendations for bedrest. Perhaps the cautious attitude of providers towards minimizing risk guides some choices. In addition, many women describe frustration about lack of clear guidelines, difficulty managing their stressful feelings, and varying degrees of support from medical providers.
In an ideal situation, bed rest during pregnancy is prescribed to help keep the mother and fetus healthy. Unfortunately, bed rest in itself is associated with potentially negative consequences in physical and mental health, and providers are not always up-to-date on changing recommendations for bedrest. Perhaps the cautious attitude of providers towards minimizing risk guides some choices. In addition, many women describe frustration about lack of clear guidelines, difficulty managing their stressful feelings, and varying degrees of support from medical providers.
During pregnancy-related bed rest, research has described how the entire family is affected. Physically, the mother may have changes in her circadian rhythms, increased anxiety, depression, and hostility. The rest of the family can also experience and demonstrate stress. Other children may act out, partners may be more stressed and worried, and financial strain may be a concern. Bigelow & Stone, 2011 Although we as rehab professionals may not have solutions for every issue, we may be able to facilitate accessing resources and at a minimum hear what a woman is dealing with during this stressful time. Many women, even when on bedrest, are allowed to attend medical appointments such as physical therapy, and should be provided with appropriate physical and mental activities to help minimize muscle atrophy and stress. Home health or hospital-based providers are also in a perfect position to educate providers on the value of referrals while the patient is at home or in the hospital.
We should keep these issues in mind during pregnancy as well as in the postpartum period. Maloni & Park (2005) measured postpartum symptoms in women who were on bedrest during pregnancy, and at 6 weeks postpartum, 40% of the 106 women (high-risk, singleton) complained of mood changes, difficulty concentrating, and other physical issues. Women who had a c-section had worsened symptoms, and the length of time on bed rest was highly correlated with the number of symptoms.
Bed rest affects a woman’s cognition, creates fear, a sense of lack of control, powerlessness, and even anger. “Because of this, Rodrigues and colleagues (Rodrigues et al., 2016) suggest that “…mental disorders should be routinely investigated during high-risk pregnancy, whenever possible with the use of specific instruments so that they can be detected early and so that interventions can be made in due time.” If you are interested in discussing this issue and many others, check out the Institute’s continuing education choices in peripartum health. The next Care of the Postpartum Patient course is taking place on September 16-17, 2017 in Nashville, TN.
Bigelow, C., & Stone, J. (2011). Bed rest in pregnancy. The Mount Sinai Journal Of Medicine, New York, 78(2), 291-302. doi: 10.1002/msj.20243
Kehler, S., Ashford, K., Cho, M., & Dekker, R. L. (2016). Experience of Preeclampsia and Bed Rest: Mental Health Implications. Issues in Mental Health Nursing, 37(9), 674-681.
Maloni, J. A., & Park, S. (2005). Postpartum Symptoms After Antepartum Bed Rest. Journal of Obstetric, Gynecologic, & Neonatal Nursing, 34(2).
Meher, S., Abalos, E., & Carroli, G. (2005). Bed rest with or without hospitalisation for hypertension during pregnancy. Cochrane Database of Systematic Reviews, 4.
Rodrigues, P. B., Zambaldi, C. F., Cantilino, A., & Sougey, E. B. (2016). Special features of high-risk pregnancies as factors in development of mental distress: a review. Trends in psychiatry and psychotherapy, 38(3), 136-140.
After my Dad’s 3rd trip to the emergency room not being able to breathe because of his sleep apnea and congestive heart failure, his cardiologist recommended he ”just relax” when his suffocating feelings occurred. Of course, not being able to catch his breath would always heighten anxiety, which made it even more difficult to inhale and exhale. Ultimately, what my Dad needed to learn was mindfulness to deal with his relatively benign inability to breathe, since the focus of mindfulness is acceptance of rather than control over your circumstances.
 The concept of mindfulness has been studied in adults, but it is gaining popularity among the pediatric population. Ruskin et al., (2017) used a prospective pre-post interventional study to assess how children with chronic pain respond to mindfulness-based interventions (MBI’s). For 8 weeks, 21 adolescents engaged in group sessions of MBI. Before, after, and 3 months post-treatment, the authors collected self-report measurements for a variety of factors such as disability, anxiety, pain quality, acceptance, catastrophizing, and social support. Subjects were highly satisfied with the treatment, and all would recommend the group intervention to friends. From baseline to 3-month follow-up, pain acceptance, body awareness, and ability to cope with stress all improved in the subjects. Further randomized controlled studies are needed, but the initial conclusion was MBI’s were received well by adolescents.
The concept of mindfulness has been studied in adults, but it is gaining popularity among the pediatric population. Ruskin et al., (2017) used a prospective pre-post interventional study to assess how children with chronic pain respond to mindfulness-based interventions (MBI’s). For 8 weeks, 21 adolescents engaged in group sessions of MBI. Before, after, and 3 months post-treatment, the authors collected self-report measurements for a variety of factors such as disability, anxiety, pain quality, acceptance, catastrophizing, and social support. Subjects were highly satisfied with the treatment, and all would recommend the group intervention to friends. From baseline to 3-month follow-up, pain acceptance, body awareness, and ability to cope with stress all improved in the subjects. Further randomized controlled studies are needed, but the initial conclusion was MBI’s were received well by adolescents.
A feasibility study performed by Anclair, Hjärthag, and Hiltunen in 2017 considered the effect of mindfulness and cognitive behavioral therapy for the parents of children with chronic conditions, looking at Health-Related Quality of Life (HRQOL), measured with Short Form-36 (SF-36), and life satisfaction. Ten parents received group-based cognitive behavioral therapy (CBT), and 9 participated in a group-based mindfulness program (MF). Treatment was implemented for 2-hour weekly sessions over the course of 8 weeks. The CBT treatment was based on the Acceptance and Commitment Therapy, focusing on changing thoughts and emotions about stressful issues as well as behaviors. They avoided the acceptance aspect, as it would overlap the MF intervention. The MF therapy used the Here and Now Version 2.0 (including daily themes on knowing your body, observing breathing, acceptance, meditation, coping, understanding thoughts versus facts, and self-care reinforcement). The parents in each group significantly improved their Mental Component Summary (MCS), Vitality, Social functioning, and Mental health scores. The MF group even showed notable improvement in Role emotional and some of the physical subscales (Bodily pain, General health, and Role physical). The CBT group showed improved satisfaction with Spare time and Relation to partner, and CBT and MF groups improved life satisfaction Relation to child. The authors conclude CBT and MF may positively affect HRQOL and life satisfaction of parents with chronically ill children.
Whether young or old or in between, how we perceive stressful situations and chronic pain can impact our health. The neurodevelopmental aspect of mindfulness is still being studied. The “Mindfulness Based Pain Treatment” course applies the concept to treating chronic pain patients. This approach brings to mind the Serenity Prayer by Reinhold Niebuhr: “Lord grant me the serenity to accept the things I cannot change, the courage to change the things I can, and the wisdom to know the difference.”
Ruskin ,DA, Gagnon, MM, Kohut SA, Stinson JN, Walker KS. (2017). A Mindfulness Program Adapted for Adolescents With Chronic Pain: Feasibility, Acceptability, and Initial Outcomes. The Clinical Journal of Pain. http://www.doi:10.1097/AJP.0000000000000490
Anclair, M., Hjärthag, F., & Hiltunen, A. J. (2017). Cognitive Behavioural Therapy and Mindfulness for Health-Related Quality of Life: Comparing Treatments for Parents of Children with Chronic Conditions - A Pilot Feasibility Study. Clinical Practice and Epidemiology in Mental Health : CP & EMH, 13, 1–9. http://doi.org/10.2174/1745017901713010001
After greeting a patient referred for temporomandibular joint dysfunction, the conversation began with an outpouring of emotion over a failed bladder sling surgery that left the woman with significant chronic pain, causing her to clench her jaw all the time. No matter what I was to find objectively with the examination, there was no doubt the treatment had to extend beyond joint mobilization, soft tissue work, and exercise. This woman clearly saw her cup as half empty, so filling her mind with a new approach to thinking about and dealing with her pain was essential for relieving her secondary jaw pain.
 Su et al. published a study called, “Pain Perception Can Be Modulated by Mindfulness Training: A Resting-State fMRI Study” (2016). The pain-afflicted group had 18 participants while the control group had 16. Brain behavior response of all subjects was measured per resting-state functional magnetic resonance imaging and 3 forms (Dallas Pain Questionnaire, Short Form McGill Pain Questionnaire-SFMPQ, and Kentucky Inventory of Mindfulness) before and after 6 weeks of mindfulness-based stress reduction treatment. Training consisted of mindfulness meditations such as a body scan, hatha yoga, walking and sitting meditation, and instruction on how to use the methods for pain management. After six 2.5-hour sessions/week and one 8-hour non-verbal session in the 4th week, the fMRI showed an increased connection from the anterior insular cortex (AIC) to the dorsal anterior midcingulate cortex (daMCC), and the SFMPQ scores were significantly improved in the pain-afflicted group. The authors suggested mindfulness training can change the brain connectivity responsible for our perception of pain.
Su et al. published a study called, “Pain Perception Can Be Modulated by Mindfulness Training: A Resting-State fMRI Study” (2016). The pain-afflicted group had 18 participants while the control group had 16. Brain behavior response of all subjects was measured per resting-state functional magnetic resonance imaging and 3 forms (Dallas Pain Questionnaire, Short Form McGill Pain Questionnaire-SFMPQ, and Kentucky Inventory of Mindfulness) before and after 6 weeks of mindfulness-based stress reduction treatment. Training consisted of mindfulness meditations such as a body scan, hatha yoga, walking and sitting meditation, and instruction on how to use the methods for pain management. After six 2.5-hour sessions/week and one 8-hour non-verbal session in the 4th week, the fMRI showed an increased connection from the anterior insular cortex (AIC) to the dorsal anterior midcingulate cortex (daMCC), and the SFMPQ scores were significantly improved in the pain-afflicted group. The authors suggested mindfulness training can change the brain connectivity responsible for our perception of pain.
Chadi et al.2016 performed a pilot study of female adolescents with chronic pain regarding the efficacy of mindfulness-based treatment. The experimental group (n=10) and the wait-list control group (n=9) consisted of girls between the ages of 13 and 18. For 8 weeks they met for a 90 minute session led by a psychiatry resident. Some of the mindfulness practices in this study included body scan, sitting and walking meditations, love and kindness meditations, mindful eating, compassion and deep listening, and breathing exercises. The wait-list control group also completed the 8-week program. Although all participants reported a positive change in the way they coped with pain, no statistically significant changes in quality of life, depression, anxiety, pain perception, and psychological distress were found. Significant salivary cortisol level improvements were observed (p<0.001) post mindful-based treatment session, indicating feasibility in pursuing further research with a larger randomized controlled trial.
Panahi and Faramarzi2016 studied mindfulness therapy effects on anxiety and depression for premenstrual syndrome (PMS). Sixty students (30 experimental, 30 control with no treatment) with mild to moderate PMS with depression underwent 8 weekly 120 minute sessions of mindfulness-based cognitive therapy (MBCT). Mean score improvements in depression, anxiety, and PMS were statistically significant from pre to post treatment for the subjects receiving MBCT. The authors stated MBCT psychotherapy could be considered beneficial for depression in mild to moderate PMS.
If jaw-clenching chronic pain owns a patient, he or she could benefit from managing the relationship through mindfulness. Our perception of pain is at the core of “whole body” treatment. The Mindfulness Based Pain Treatment course could help fill your patients’ as well as your own cup with healing.
If you're interested in learning more about mindfulness-based treatment techniques, Herman & Wallace offers three courses which you should consider. Mindfulness-Based Pain Treatment focuses on patient treatment, and the Mindfulness for Rehabilitation Professionals.
Su, I.-W., Wu, F.-W., Liang, K.-C., Cheng, K.-Y., Hsieh, S.-T., Sun, W.-Z., & Chou, T.-L. (2016). Pain Perception Can Be Modulated by Mindfulness Training: A Resting-State fMRI Study. Frontiers in Human Neuroscience, 10, 570. http://doi.org/10.3389/fnhum.2016.00570
Chadi, N., McMahon, A., Vadnais, M., Malboeuf-Hurtubise, C., Djemli, A., Dobkin, P. L., … Haley, N. (2016). Mindfulness-based Intervention for Female Adolescents with Chronic Pain: A Pilot Randomized Trial. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 25(3), 159–168.
Panahi, F., & Faramarzi, M. (2016). The Effects of Mindfulness-Based Cognitive Therapy on Depression and Anxiety in Women with Premenstrual Syndrome. Depression Research and Treatment, 2016, 9816481. http://doi.org/10.1155/2016/9816481
Faculty member Jennafer Vande Vegte, MSPT, BCB-PMD, PRPC has written in to encourage us all to practice kindness and patience. A positive attitude can affect more than just your friends and family; your patients will benefit in so many ways as well!
 First a little personal story. Several years ago my daughter was going through a tough time and we worked with a child psychologist. He was a wonderful man who taught my husband and I so much about how to raise a challenging kiddo. The foundation of what we needed to learn was the power of positive. People need nine (or so) positive interactions to override a negative one. Poor kid was definitely at a deficit! So if she did something that needed correcting, we were to give her a chance at a "do over" where sometimes we had to coach her to choose a better action. After she got it right, we lavished praise on our little pumpkin. And would you believe, not only did all that positiveness make a difference for her, it made a difference for her parents too!
First a little personal story. Several years ago my daughter was going through a tough time and we worked with a child psychologist. He was a wonderful man who taught my husband and I so much about how to raise a challenging kiddo. The foundation of what we needed to learn was the power of positive. People need nine (or so) positive interactions to override a negative one. Poor kid was definitely at a deficit! So if she did something that needed correcting, we were to give her a chance at a "do over" where sometimes we had to coach her to choose a better action. After she got it right, we lavished praise on our little pumpkin. And would you believe, not only did all that positiveness make a difference for her, it made a difference for her parents too!
Now back to the clinical. Just about two years ago I had the privilege of teaching with Nari Clemons. We taught PF2B together. Nari said something during one of her lectures that revolutionized my PT practice. She challenged us in lab to find three positive things about our lab partner and share those things before recognizing any deficits. How many times do we get finished with an evaluation and sit down with a patient and list all the things we found that need correction or help, perhaps drawing on our Netter images to fully illustrate the parts of their body that are broken or need fixing.
So I changed things up a bit and started remarking about the positive things I found on exam. "Wow, your hips are really strong and stable." "You've got a really coordinated breathing pattern, that is going to work in your favor." "You're pelvic muscles are really strong." and then later drawing on those positives outline how we could use the patient's strengths to help them overcome their challenges. "Because you have a great breathing strategy we are going to use that to help your whole nervous system to relax which with help your pelvic floor relax," for example.
The results were shocking. Person after person told me how much it meant to them to leave feeling positive and hopeful. One delightful woman who I saw for a diastasis had amazing leg muscles and I told her so. When she returned she said, "I've felt so self conscious about my flabby belly, but this week all I could think about were my strong leg muscles. Thanks for telling me that."
We do know is that our attitudes and beliefs as providers influence not only our clinical management but patient outcomes as well. Darlow et. al. performed a comprehensive literature review looking at how attitudes and beliefs among health care providers affected outcomes in patients with low back pain and discovered, "There is strong evidence that health care provider beliefs about back pain are associated with the beliefs of their patients."
Why not use that truth to our advantage and be positive? Would love to hear about your experiences!
Join Jennafer at one of her upcoming courses, Pelvic Floor Level 2B - Trenton, NJ - February 24-26, 2017, Pelvic Floor Series Capstone - Arlington, VA - May 5-7, 2017, Pelvic Floor Series Capstone - Columbus, OH - August 18-20, 2017, and Pelvic Floor Series Capstone - Tampa, FL - December 2-4, 2016.
With menopause and the hormonal shifts that take place, some women suffer more than others with symptoms such as hot flashes. If you have ever been near someone during a hot flash, you know that this curious condition is more than feeling a little hot under the collar. During a hot flash, women will suddenly disrobe, wake from a deep sleep covered in sweat (so much so that they have to change the sheets!), or otherwise appear distressed and oftentimes suffer interference in whatever activity in which they were engaging. As we reported in an earlier post, women on average may have hot flashes for 5 years after the date of her last period. Some women (up to 1/3 in the referenced study) will report hot flashes for 10 or more years after menopause.
 Hot flashes and night sweats also significantly disrupt sleep, according to research by Baker and colleagues. Menopausal women with insomnia may also have higher levels of psychologic, somatic, vasomotor symptoms, and score lower on the Beck Depression Inventory, and sleep efficiency and duration scores. Poor sleep can be associated with morbidity such as hypertension, stroke, diabetes and depression, so interrupted sleep is more than an inconvenience, but potentially a serious health issue.
Hot flashes and night sweats also significantly disrupt sleep, according to research by Baker and colleagues. Menopausal women with insomnia may also have higher levels of psychologic, somatic, vasomotor symptoms, and score lower on the Beck Depression Inventory, and sleep efficiency and duration scores. Poor sleep can be associated with morbidity such as hypertension, stroke, diabetes and depression, so interrupted sleep is more than an inconvenience, but potentially a serious health issue.
A more recent study linked anxiety as a potential risk factor for menopausal hot flashes. In 233 women who are premenopausal at baseline and who were followed for at least a year after their final menstrual cycle, anxiety symptoms, hormone levels, hot flashes and other psychosocial variables were assessed. During the 14 year follow-up 72% of the women reported having moderate to severe hot flashes, and the researchers correlated somatic anxiety as a potential predictive association with anxiety. Somatic anxiety refers to the physical symptoms of anxiety, such as stomach ache, increased heart rate, sweating, muscle aches.
In order to help a woman support her wellness during menopausal transitions, being able to address somatic anxiety and conditions like hot flashes is imperative. Teaching skills such as breathing, relaxation training, meditation, or mindfulness may positively impact the anxiety, and therefore have the potential to reduce hot flashes and other adverse symptoms. Herman & Wallace's Menopause Rehabilitation and Symptom Management course is an excellent opportunity to learn some of these valuable skills.
Baker, F. C., Willoughby, A. R., Sassoon, S. A., Colrain, I. M., & de Zambotti, M. (2015). Insomnia in women approaching menopause: beyond perception. Psychoneuroendocrinology, 60, 96-104.
Freeman, E. W., & Sammel, M. D. (2016). Anxiety as a risk factor for menopausal hot flashes: evidence from the Penn Ovarian Aging cohort. Menopause, 23(9), 942-949.
Freeman, E. W., Sammel, M. D., & Sanders, R. J. (2014). Risk of long term hot flashes after natural menopause: Evidence from the Penn Ovarian Aging Cohort. Menopause (New York, NY), 21(9), 924.
Help others by helping ourselves
As pelvic rehabilitation practitioners, we have all been there, looking ahead to see what patients are on our schedules and recognizing that several will require immense energy from us… all afternoon! Then we prepare ourselves, hoping we have enough stamina to get through, and do a good job to help meet the needs of these patients. Then we still have to go home, spend time with our families, do chores, run errands, and have endless endurance. This can happen day after day. Naturally, as rehabilitation practitioners, we are helpers and problems solvers. However, this requires that we work in emotionally demanding situations. Often in healthcare, we experience burnout. We endure prolonged stress and/or frustration resulting in exhaustion of physical and/or emotional strength and lack of motivation. Do we have any vitality left for ourselves and our loved ones? How can we help ourselves do a good job with our patients, but to also honor our own needs for our energy?
 How do we as health care practitioners’ prevent burnout?
How do we as health care practitioners’ prevent burnout?
Ever hear of “mindfulness” ... I am being facetious. The last several years we have been hearing a lot about “mindfulness” (behavioral therapy or mindfulness-based stress reduction) and its positive effects in helping patients cope with chronic pain conditions. Mindfulness is defined as “the practice of maintaining a nonjudgmental state of heightened or complete awareness of one's thoughts, emotions, or experiences on a moment-to-moment basis,” according to Merriam-Webster’s Dictionary. One can practice mindfulness in many forms. Examples of mindfulness-based practice include, body scans, progressive relaxation, meditation, or mindful movement. Many of us pelvic rehabilitation providers teach our patients with pelvic pain some form of mindfulness in clinic, at home, or both, to help them holistically manage their pain. Whether it is as simple as diaphragmatic breathing, awareness of toileting schedules/behavior, or actual guided practices for their home exercise program, we are teaching mindfulness behavioral therapy daily.
Why don’t we practice what we preach?
As working professionals, we are stressed, tired, our schedules too full, and we feel pain too, right? Mindfulness behavioral therapy interventions are often used in health care to manage pain, reduce stress, and control anxiety. Isn’t the goal of using such interventions to improve health, wellness, and quality of life? Mindfulness training for healthcare providers can reduce burnout by decreasing emotional exhaustion, depersonalization, and increasing sense of personal accomplishment. Additionally, it can improve mood, empathy for patients, and communication.1 All of these improvements, leads to improved patient satisfaction.
Let’s take what we teach our patients every day and start applying it to ourselves. An informal way to integrate mindfulness is by building it into your day. Such as when washing hands in between patients, or before you walk into the room to greet the patient. However, sometimes we have a need for a tangible strategy to combat stress and the desire to be guided by an expert with this strategy.2 I think one of the easiest ways to begin practicing mindfulness is to try a meditation application (app) on a smart phone or home computer. Meditation is one of the most common or popular ways to practice mindfulness and is often a nice starting point to try meditation for yourself or to suggest to a motivated patient. Many popular guided meditation apps include Headspace, Insight Timer, and Calm, just to name a few. Generally, these guided meditation apps have free versions and paid upgrades. Challenge yourself to complete a 10-minute guided meditation app, daily, for three weeks, and see how you feel. It takes three weeks to make a new habit. Hopefully, guided meditation will be a new habit to help you be present with your patients and improve your awareness and energy. After all, how can we help others heal, if we can’t help ourselves?
To learn more about ways, you as a professional can help yourself or your patients with meditation, consider attending Meditation for Patients and Providers.
1)Krasner, M.S., Epstein, R.M., Beckman, H., Suchman, A.L., Chapman, B., Mooney C.J., et al. (2009). Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA 302(12):1284–93.
2)Willgens, A. M., Craig, S., DeLuca, M., DeSanto, C., Forenza, A., Kenton, T., ... & Yakimec, G. (2016). Physical Therapists' Perceptions of Mindfulness for Stress Reduction: An Exploratory Study. Journal of Physical Therapy Education, 30(2).
The following comes to us from Carolyn McManus, PT, MS, MA, our resident expert in the power of mindfulness and it's applications to rehabilitation. Carolyn was recently featured in a video from the Journal of the American Medical Association for her contributions to a newly published research article. Join Carolyn at her course, Mindfulness Based Pain Treatment: A Biopsychosocial Approach to the Treatment of Chronic Pain on May 14th and 15th in California's Bay Area!
 Neuroimaging studies show that cortical and sub-cortical brain regions associated with cognitive and emotional processing connect directly with descending pain modulating circuits arising in the brainstem. As diminished nociceptive inhibition by descending pain modulation is a likely contributing factor to the persistence of pain, these cortical and sub-cortical connections to relevant brainstem regions provide a means by which maladaptive cognitive and emotional processing can contribute to the persistence of pain1. It is possible that strategies to help patients self-regulate cognitions and emotions could promote pain reduction through restoring the balance between excitatory and inhibitory mechanisms of the descending pain modulatory system.
Neuroimaging studies show that cortical and sub-cortical brain regions associated with cognitive and emotional processing connect directly with descending pain modulating circuits arising in the brainstem. As diminished nociceptive inhibition by descending pain modulation is a likely contributing factor to the persistence of pain, these cortical and sub-cortical connections to relevant brainstem regions provide a means by which maladaptive cognitive and emotional processing can contribute to the persistence of pain1. It is possible that strategies to help patients self-regulate cognitions and emotions could promote pain reduction through restoring the balance between excitatory and inhibitory mechanisms of the descending pain modulatory system.
To be mindful is to rest the mind in the present moment with stability and acceptance and without additional cognitive or emotional elaboration. Mindful body awareness is a central component. Training in mindful awareness has been shown to improve attention regulation, emotional processing and body awareness and contribute to reduced pain intensity, catastrophizing, depression and anxiety2,3,4,5. Training in mindfulness has also been shown to modulate brain activity in areas associated with body awareness and pain processing6,7. It is possible that the adaptive modulation of cortical and sub-cortical areas engaged with mindful cognitive, emotional and physical self-regulation could contribute to reducing pain through improving the balance between excitatory and inhibitory mechanisms of the descending pain modulatory system.
One of my patients reflected the clinical benefits of mindfulness training when he said, “I needed to learn how to not freak out when my exercises or daily activities increased my pain. Focusing my mind on the present moment was enormously helpful. I would tell myself, “Breathe. Just be here. Calm down.” By breathing and relaxing I could take control of how I was reacting and I immediately saw a difference. My pain did not increase out of control.”
I am thrilled to be sharing my 30+ year experience in mindfulness and patient care in my upcoming course through Herman and Wallace.
1. Ossipov M, Morimura K, Porreca F. Descending pain modulation and chronification of pain. Curr Opin Support Palliat Care 2014;8(2):143-151.
2. Holzel BK, Lazar SW, Guard T, et al. How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspect Psychol Science. 2011;6: 537–559.
3. Reiner K, Tibi L, Lipsitz JD. Do mindfulness-based interventions reduce pain intensity? A critical review of the literature. Pain Med. 2013 Feb;14(2):230-42.
4. Lakhan SE, Schofield KL. Mindfulness-based therapies in the treatment of somatization disorders: a systematic review and meta-analysis. PLoS One. 2013 Aug 26;8(8):e71834.
5. Schutze , Slater H, O’Sullivan P, et al. Mindfulness-based functional therapy: A preliminary open trial of an integrated model of care for people with persistent low back pain. Front Psychol. 2014 Aug 4;5:839.
6. Zeidan F, Martucci KT, Kraft RA, et al. Brain mechanisms supporting modulation of pain by mindfulness meditation. J Neurosci. 2011 Apr 6;31(14):5540-8.
7. Nakata H, Sakamoto K, Kakigi R. Meditation reduces pain-related activity in the anterior cingulated cortex, insula, secondary somatosensory cortex and thalamus. Front psychol. 2014;5:1489.