More than Just Sticking It In! Getting Past Plateaus with Vaginal Trainers (Dilators) for Vaginismus

Lifelong vaginismus is a condition where a person experiences pain or difficulty with vaginal insertion from the first attempt. This could include the insertion of a tampon, gynecologic speculum, finger, penis, or sex toy. Many patients report, "I always had trouble with tampons" and may avoid using them altogether. They might also avoid pelvic exams and face significant challenges with receptive sexual activity.
Pelvic trainers, also known as dilators, vaginal trainers, or accommodators, can be effective tools for addressing lifelong vaginismus. However, as a pelvic health clinician, you may have noticed that some patients reach a plateau, getting "stuck" at a certain size trainer. Lifelong vaginismus is believed to be due to uncontrolled spasms of the pelvic floor muscles surrounding the vaginal opening. These spasms can hinder the insertion of progressively larger trainers and are not easily managed through passive stretching alone.
Instead, combining passive stretching with techniques like breathing and contract-relax exercises can be beneficial. Using muscle contractions may seem counterintuitive, but they can effectively promote muscle relaxation and control. Let's explore four scientific perspectives on how this works.
- Physiology of Skeletal Muscle
Skeletal muscle, which includes the pelvic floor muscles, responds to isometric contractions by activating Golgi Tendon Organs (GTOs) embedded in the muscle fibers. When GTOs are activated, they send signals to the spinal cord, triggering a reflex that inhibits the same muscle. Essentially, an isometric contraction causes the muscle to inhibit itself. This technique, known as "hold-relax" in Proprioceptive Neuromuscular Facilitation (PNF) stretching, may increase flexibility in the pelvic floor muscles when performed around the trainers.
- Neurological Effects
Repeated, sub-maximal contractions followed by gentle stretching and intentional relaxation can increase corticospinal excitability, promoting motor learning and performance (Christiansen et al., 2018). Over time, practicing voluntary contraction and relaxation, along with breathing exercises, helps patients gain more control over the muscles surrounding the vagina.
- Pain Science Perspective
Voluntary contractions activate the motor cortex in the brain, which has two effects on inhibiting pain (Lopes et al., 2019):
- Inhibition of the thalamic nuclei (lateral spinothalamic tract), limiting nociceptive messages.
- Activation of the periaqueductal gray, which contains enkephalin-producing cells that release endogenous opioids to suppress pain.
These effects reduce pain and facilitate the progressive insertion of vaginal trainers.
- Graded Exposure
Graded exposure involves gradually increasing exposure to an activity that causes fear or anxiety. Starting with the smallest size, trainers are inserted to the "just the start of discomfort" point (not to pain). This is followed by breathing exercises and gentle voluntary contractions and relaxations ("hold-relax" technique) along with passive stretching. As discomfort lessens, the trainer can be inserted further, repeating the steps. This process, over several sessions, allows progression to larger trainer sizes, reducing fear and anxiety while increasing functional insertion and decreasing pain.
Practical Application
During a session, a patient may insert a trainer just to the point of discomfort. The clinician can then guide them through the hold-relax routine:
- Take a breath in.
- Exhale and gently squeeze the pelvic floor muscles around the trainer – hold, hold, hold (through the full exhale).
- Release the muscles while inhaling again.
Repeat for 3-5 repetitions. After the last hold-relax, keep the muscles relaxed while gently pressing the trainer to stretch along the vaginal wall for 30-60 seconds, maintaining the same insertion depth. Repeat these steps for the posterior, left, and right vaginal walls (avoiding the anterior wall to prevent irritation of the urethra). These instructions can be adapted based on the individual patient.
In the Vaginismus and Vulvovaginal Dyspareunia course, participants learn and practice these steps, along with other techniques for addressing painful vaginal intercourse. The course covers selecting trainers, using lubricants, sexual positions, props and aids, perineal scar massage, and specific manual therapy treatments. It also provides guidance on discussing sexual activity with patients, including when to pause or continue, and how to involve partners. A rehabilitative treatment decision-making algorithm based on examination findings helps clinicians determine the most effective treatment combinations for each patient. Join us in the next Vaginismus and Vulvovaginal Dyspareunia course, scheduled for September 14, 2024.
For patients struggling with vaginal trainer progression, try these breathing, hold-relax, and gentle stretching techniques in your clinic this week. It may transform trainers from a frustrating obstacle into a useful and functional tool.
References:
Christiansen, L., Madsen, M. J., Bojsen-Møller, E., Thomas, R., Nielsen, J. B., & Lundbye-Jensen, J. (2018). Progressive practice promotes motor learning and repeated transient increases in corticospinal excitability across multiple days. Brain stimulation, 11(2), 346-357.
Lopes, P. S. S., Campos, A. C. P., Fonoff, E. T., Britto, L. R. G., & Pagano, R. L. (2019). Motor cortex and pain control: exploring the descending relay analgesic pathways and spinal nociceptive neurons in healthy conscious rats. Behavioral and Brain Functions, 15(1), 1-13.
AUTHOR BIO
Darla Cathcart, PT, DPT, PhD, WCS, CLT

Darla graduated from Louisiana State University (Shreveport, LA) with her physical therapy degree, performed residency training in Women’s Health PT at Duke University, and completed a Ph.D. at the University of Arkansas Medical Sciences. Her dissertation research focused on using non-invasive brain stimulation to augment behavioral interventions for women with lifelong vaginismus, and her ongoing line of research focuses on painful intercourse and post-Cesarean rehabilitation.
Darla’s certifications and training include Women’s Health Certified Specialist (WCS, board certification through the American Board of Physical Therapy Specialties). Certificate of Achievement in Pelvic Physical Therapy (CAPP-Pelvic). Certificate of Achievement in Pregnancy & Postpartum Physical Therapy (CAPP-OB). Certified Lymphedema Therapist (CLT).
Darla began her women’s health physical therapy career in her first job while working with pregnant women with musculoskeletal problems in a private outpatient therapy clinic in Shreveport, LA (with a focus on spine rehab). While there, she developed and hosted an exercise class for pregnant women. She would go on to develop a mom-and-baby postpartum exercise class while in her Duke residency in Durham, NC. She went on to develop the pelvic, pregnancy, and post-breast cancer/lymphedema PT program at Christus-Schumpert Health System in Shreveport, LA. During this time, she participated in educating women in the labor and birth preparatory classes hosted by the hospital; she also taught the women’s health course for physical therapy students at LSU-Shreveport. Darla went on to serve as a full-time faculty member in the physical therapy program at the University of Central Arkansas in Conway, AR, where she taught women’s health topics, documentation, therapeutic exercise, professional development, and human physiology. She recently owned a private PT practice that is dedicated to pelvic (bowel, bladder, and pelvic pain) and pregnancy/postpartum conditions in Conway, AR. Darla now is a full-time faculty member in the entry-level Physical Therapy program at Graceland University.
Darla currently serves as the President of the Academy of Pelvic Health of the American Physical Therapy Association. She has several peer-reviewed and non-peer-reviewed scientific publications. Amongst some of these, she co-authored “Clinical Summary: Urinary Incontinence” for PTNow.org in April 2015. She authored the chapter titled “The Female Hip and Pelvis” in Orthopedic Management of the Hip and Pelvis (S Cheatham, M Kolber, Elsevier, 2015). She chaired the committee for and participated heavily in the development of the Certificate of Achievement in Pregnancy/Postpartum (CAPP-OB) course series for the Section on Women’s Health of the American Physical Therapy Association. Darla has spoken and instructed many courses in local, national, and international settings on a variety of pelvic, pregnancy/postpartum, and other women’s health physical therapy topics. Darla has served as the Director of Education (2011-2014) and as Vice President (2015-2016) for the Section on Women’s Health, American Physical Therapy Association. She also served as a technical expert panel member on Treatments for Fecal Incontinence, Agency for Healthcare Research and Quality in 2014-2015. She also volunteered as a Women’s Health Certified Specialist Exam Standardization Task Force member in May 2013. Darla received several awards from the Section on Women’s Health: CAPP-OB Instructor of the Year (2017); Course Site Hostess of the Year (2018); and Volunteer of the Year (2015). She also received Clinical Instructor of the Year while serving as a clinical instructor a pelvic health physical therapy student from Elon University in 2011.
Darla Cathcart, PT, DPT, Ph.D., WCS, CLT graduated from Louisiana State University (Shreveport, LA) with her physical therapy degree, performed residency training in Women’s Health PT at Duke University, and received her Ph.D. from the University of Arkansas Medical Sciences. Her dissertation research focus was on using non-invasive brain stimulation to augment behavioral interventions for women with lifelong vaginismus, and her ongoing line of research will continue to center around pain with intercourse. Darla is part of Herman & Wallace's core faculty and recently launched her own course Vaginismus and Vulvovaginal Dyspareunia. She sat down with the Pelvic Rehab Report to discuss working with vaginismus and vulvovaginal dyspareunia patients.
I believe one of the most important things that we as pelvic therapists can do for patients experiencing vaginismus and vulvovaginal dyspareunia is to offer HOPE!
These patients often arrive at therapy with a belief that something is uniquely wrong with them. Often, they have been to more than a handful of other doctors and care providers who are unfamiliar with pelvic floor problems causing pain with sex (which is substantiated by the research) who have maybe given them messages of "I can't find anything wrong with you" and "You just need to relax."
If I had a dollar for every time a patient told me that another care provider told them to "Just drink a glass of wine before sex to help you relax" (palm to forehead!)...These messages often cause these patients to feel as if their pain with sex is made up in their heads, or that a scary diagnosis is being overlooked.
Unfortunately, unless they have found a provider who can quickly identify that the patient has a musculoskeletal problem with the pelvic floor that needs a pelvic therapy referral, then the patient has often gone for many months, years, or even a decade or more without being properly heard or getting the right help.
When I sit down with a patient, after hearing a bit of that person's story, I typically start the conversation with "Thank you for sharing your story. I want you to know that you are not alone - a big percentage of my patients have pain with sex. I also want you to know that based on what you are telling me, you will likely get better as most of them have done."
Patients often express relief, sometimes disbelief, or both, mixed with some hope - a bit of "Ah, this person hears me and knows what I'm talking about, and says I can get better!" The belief of being able to get better, even if mixed with some doubt, is an extremely valuable start on their healing journeys.
There are many factors that the pelvic therapist could consider to facilitate conversations around pain with sex.
As with all of our patients seeking pelvic rehab, communication requires non-judgment and respecting a patient's boundaries. Asking a patient "Have you been sexually abused or had sexual trauma in the past?" can feel unnerving and alarming for a patient who is not ready to have that conversation with their pelvic therapist. However, asking a patient "Have you had any negative sexual experiences that you would like to share, that you feel may be impacting your symptoms?" allows the patient to decline until they feel ready to engage in such a conversation.
This softer approach lets the patient know that the therapist is open to a conversation about impactful events and respects that patient's autonomy in sharing that history. Putting the patient in the driver's seat is also critical. For instance, consider a patient who, theoretically, would benefit greatly from using vaginal trainers (dilators) but declines to use them. An approach of "but using trainers will be the only way to get better" may result in the patient quitting therapy, or worse, feeling traumatized from the therapy experience. Alternatively, affirming to patients that the treatments chosen are their prerogative keeps the path for ongoing healing and provider trust.
A statement of "Not using vaginal trainers is your choice, but we can always consider them again in the future if you change your mind. Let me talk you through the alternative treatments, and how their effects will differ from that of the vaginal trainer use" leaves the door open to return to that treatment down the road if the patient chooses, and also respects the choice of the patient in the moment. The key is to not be pushy about pursuing the undesired treatment down the road! It could be mentioned again, but use judgment and caution in the approach.
A final highlight is being sure to give patients space to share their story, as often they have not been heard by previous providers or their symptoms have been discounted.
My course Vaginismus and Vulvovaginal Dyspareunia, is scheduled for March 3rd and September 14th this year and takes a deep dive into the detail of how to make the rubber meet the road to not only get treatment started but to really help progress a patient into a satisfying sex life. This course was developed so that the participant could leave this course and understand how to really approach the examination, history taking, and step-by-step procedures in instructing and using vaginal trainers and other tools for patients having painful intercourse. Additionally, this course should increase the practitioner's confidence in incorporating instructions and education related to a patient's concerns about the female sexual cycle and response (arousal, desire, orgasm), sexual positioning, lubrication, and partner integration.
Darla Cathcart, PT, DPT, WCS, CLT graduated from Louisiana State University (Shreveport, LA) with her physical therapy degree, performed residency training in Women’s Health PT at Duke University, and received her Ph.D. from the University of Arkansas Medical Sciences. Her dissertation research focus was on using non-invasive brain stimulation to augment behavioral interventions for women with lifelong vaginismus, and her ongoing line of research will continue to center around pain with intercourse. Darla is part of Herman & Wallace's core faculty and instructs Pelvic Floor Level 1, Level 2A, and Level 2B, the Pregnancy & Postpartum Series, and recently launched her own course Vaginismus and Vulvovaginal Dyspareunia.
How is this class different from the information in Pelvic Floor 2B?
The main difference is in the questions that these two courses answer: "what treatments can I use" versus "how can I use those treatments effectively?" In Pelvic Floor Level 2B, participants are told about various methods for addressing pain with intercourse (such as using vaginal trainers/dilators and manual therapy techniques), with brief descriptions of how to use some of these tools. In this Vaginismus and Vulvovaginal Dyspareunia course, we go into depth on how to use these treatments specifically based on a patient's examination findings and goals.
What are the top 5 takeaways a practitioner could hope to gain from this class?
1. Vaginal Trainers (dilators) can be more effective when going beyond "just sticking them in."Traditionally, patients have been taught to just insert "dilators" to a point of stretching and discomfort, and to hold that stretch, maybe even distract themselves from the activity by watching TV or reading a book. As with other areas of the body, using active methods to increase tissue flexibility, such as incorporating contract-relax and breathing techniques, can really enhance the treatment! During the labs in this 100% remote course (a combination of self-paced preview videos and live online instruction), participants will be guided through step-by-step instructions for using and progressing through vaginal trainers and other treatments (the same step-by-step instructions you can use with your patients on Monday morning!). Additionally, as in other areas of the body, focusing on the body part that is being worked on is beneficial for increasing motor control, which is also desirable for addressing pelvic floor muscles that have too much tone and tenderness or pain with attempts at insertion. Participants will also be walked through activities that increase the brain's connection with and control of the pelvic floor and genitals, thus tapping into contemporary pain science concepts as well. And speaking of pain science . . .
2. As a practitioner, you likely already know that our words, verbiage for questions and instruction, and analogies and stories matter! Throughout the course, we will talk about why some words or terms can be harmful or less helpful, and how to replace them with healing or more neutral terms. For instance, we will talk about how the traditional term "dilator" can be a bit scary and anxiety-provoking for someone who has had lifelong vaginismus; but the term "trainer" suggests that the muscles are being taught and retrained on how to function. We will also walk through examples of approaching and discussing sexual abuse and trauma, general sexual history and activity, and patient goals. We will review some basics about contemporary pain science, and analogies that we can share with our patients to help decrease their fear and anxiety surrounding treatment for and engaging in sexual function. Participants should leave the course feeling more confident in talking about sex with their patients!
3. How do we incorporate the female sexual cycle/response (arousal, desire, orgasm), sexual positioning, and sexual assist devices and props into helping our patients? These are topics that will be tackled and broken down in both the preview material, with key concepts being reviewed or covered during the live remote portion of the course. We will talk about using the timing of sexual responses to a patient's advantage with transitioning to sexual function.
4. When should a patient move from vaginal trainers to the bedroom? Should the patient's partner(s) be involved? How do I answer questions about specific sexual positions? How do I answer my patient's questions about libido concerns? These are all concepts that will be tackled, with both specific examples and cases and also with general guidelines for applying the information to your individual patients.
5. You will have the opportunity to practice or follow along with the very things you will teach your patients during the live remote lab portion of the course, from the privacy of your own home or private treatment room in your office. I believe a great advantage that rehabilitation professionals have in treating patients is that we have experienced many of the examination and treatment techniques while practicing them in a class, course, or another setting. Personally testing out these techniques gives you, as a practitioner, a strong advantage in knowing how to best describe the nuances of applying treatments to aid in your patient's understanding. It also gives you a good dose of empathy for being the person on the table!
What special interest do you have in this topic?
As a pelvic health therapist for over 20 years, working with patients who have lifelong vaginismus, acquired vaginismus, and dyspareunia has been one of my primary passions. In completing a Ph.D. in 2020, my line of research began with a clinical randomized controlled trial working with patients with lifelong vaginismus and vaginal trainers, using neuroscience and pain science concepts to incorporate contract-relax and breathing techniques to enhance treatment. I never tire of having a patient return to the clinic excited that they finally had pain-free intercourse! I am passionate about teaching other therapists, healthcare providers, patients, and their partners about the concepts I've learned in my many years of practice.
Who is the audience for this class?
This course is for any pelvic health rehabilitation or health care provider who is a novice or wants to enhance their skills for working with patients with vaginismus and vulvovaginal dyspareunia.
Why was it needed and developed?
This course, Vaginismus and Vulvovaginal Dyspareunia, is needed to move beyond the basic concepts about what we can do to help patients having pain with intercourse. This course takes a deep dive into the detail of how to make the rubber meet the road to not only get treatment started but to really help progress a patient into a satisfying sex life. This course was developed so that the participant could leave this course and understand how to really approach the examination, history taking, and step-by-step procedures in instructing and using vaginal trainers and other tools for patients having painful intercourse. Additionally, this course should increase the practitioner's confidence in incorporating instructions and education related to a patient's concerns about the female sexual cycle and response (arousal, desire, orgasm), sexual positioning, lubrication, and partner integration.
Vaginismus and Vulvovaginal Dyspareunia
Course Date:
February 4
Price: $375
Experience Level: Beginner
Contact Hours: 15
Description: This course is for the pelvic health practitioner who is new to treating patients with vaginismus/vulvovaginal dyspareunia or to vaginal trainer(dilator) use or pelvic health rehabilitation; or for the experienced practitioner who has found that patients with vaginismus/vulvovaginal dyspareunia plateau with vaginal trainers or other treatments. In this course, pelvic health rehabilitation providers will learn about the different types of vaginismus and dyspareunia. Definitions and history of terminology will be explained related to pain with sexual activity and intercourse, including Genito-Pelvic Pain/Penetration Disorder, Lifelong or Primary Vaginismus, Acquired or Secondary Vaginismus, Dyspareunia, Vulvodynia, and others.
From a pain-science viewpoint, verbiage and terminology to reduce patient fear and anxiety will be discussed and incorporated throughout the course. Evidence for focalized dystonia as a component of lifelong vaginismus and how that impacts treatment will be reviewed. Causes for acquired vaginismus (such as postpartum healing or hormonal changes) will be addressed. Treatment approaches for reducing patient fear and anxiety, addressing medical and/or sexual trauma/abuse history, and promoting patient empowerment will be covered. The remote live portion of the course will also focus on rehabilitation treatments, including walking the participant through the functional use of vaginal trainers (commonly known as dilators), and methods for progressing their use. Clinical cases will be provided to illustrate a variety of treatment approaches based on different patients’ treatment goals, history, examination findings, and sexual pain diagnosis.
I recently assisted at a Pelvic Floor Level 2B course which has been updated with recent research, new sections, and less repetition from Pelvic Floor Level 1. In the course they mentioned this article which sparked a lively discussion and I had to learn more. It is rare to see a study with a large number of participants in pelvic health and especially with a vaginismus diagnosis.
Vaginismus is defined as a genito-pelvic pain/penetration disorder along with dyspareunia under the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders; Fifth Edition) in which penetration is often impossible due to pain and fear. Vaginismus is both a physical and psychological disorder as it exhibits both muscle spasms and fear/anxiety of penetration. Symptoms vary by severity. Common presentation is an inability or discomfort to insert/remove a tampon, pain with penetration, and complaints of “hitting a wall” in attempted penetration; and inability to participate in gynecological exams.
 The authors of this study evaluated the severity of vaginismus. The penetrative history was used in addition to presentation at pelvic exam, and then given a level. There are 2 grading systems, Lamont and Pacik, that indicate the level of fear and anxiety about being touched. They found that those with severe vaginismus were Lamont levels 3 and 4, and Pacik level 5. For example, a Pacik Level 5 includes Lamont grade 4 “generalized retreat: buttocks lift up; thighs close, patient retreats” plus a visceral reaction such as “palpitations, hyperventilation, sweating, severe trembling, uncontrollable shaking, screaming, hysteria, wanting to jump off the table, a feeling of going unconscious, nausea, vomiting and even a desire to attack the doctor”.
The authors of this study evaluated the severity of vaginismus. The penetrative history was used in addition to presentation at pelvic exam, and then given a level. There are 2 grading systems, Lamont and Pacik, that indicate the level of fear and anxiety about being touched. They found that those with severe vaginismus were Lamont levels 3 and 4, and Pacik level 5. For example, a Pacik Level 5 includes Lamont grade 4 “generalized retreat: buttocks lift up; thighs close, patient retreats” plus a visceral reaction such as “palpitations, hyperventilation, sweating, severe trembling, uncontrollable shaking, screaming, hysteria, wanting to jump off the table, a feeling of going unconscious, nausea, vomiting and even a desire to attack the doctor”.
241 patients participated in this study, with a mean duration of 7.8 years. 70% of participants were a Lamont level 4 or Pacik level 5 at baseline. The authors looked at previous treatments tried and coping strategies; 74% had tried lube, 73% had tried dilators, 50% had tried Kegels, 28% had tried physical therapy, 3% had tried a surgical vestibulectomy. The full table 2 is in the article. Most participants had a mean of at least 4 failed treatments.
The aim was to help these women to achieve pain free intercourse after treatment. In order to tolerate the treatment, many were sedated with midazolam before the Q-tip test, and more sedation given as needed. The treatment lasted for about 30 minutes and consisted of:
- Q-tip test with as minimal sedation as possible to rule out vulvodynia and provoked vestibulodynia
- Digital exam of tolerance in order to assess the level of spasm in introitus. Graded 0 (no spasm) to 4 (severe spasm where digital insertion was difficult)
- Botox 50 U injections to right and left submucosal space near the bulbospongiosus muscle administered with a pediatric speculum placed. Additional Botox was injected submucosally into levator ani muscles if also in spasm/tight
- Injections 0.25% bupivacaine (a numbing agent) 1 mL increments along right and left lateral vaginal walls (9 mL per side) from cervix to introitus
- Progressive dilation; circumference 3 inches (#4), 4 inches (#5), 5 inches (#6)
- Reassessed with digital examination
- Re-insert #5 or #6 dilator and patient was awakened and taken to recovery
If the patient consented, her partner could be present during the procedure and was allowed to palpate the level of spasm with gloved digit and was educated on dilator insertion. The authors noted that many partners had a ‘profound’ experience.
A nurse worked with the couple for about two hours in the recovery room to help them be more comfortable moving the dilator in and out with minimal-to-no pain as the numbing agent lasts 6-8 hours. Three participants were treated each time and consented to meet each other. Patients were discharged with #4 dilator in place and asked to keep in until the next day. They were given Ibuprofen and sleeping aids as needed.
Day 1
Participants return with partners and progress up to larger sizes (#5 and #6). They participate in group counseling with the primary researcher Dr. Pacik. This lasted about 5 hours; and consisted of education of dilator progression, returning to intercourse and lubricants. If participants wished to have private counseling instead that was granted. Many exchanged contact information. They were encouraged to continue seeing their healthcare clinicians as indicated; sex therapists, physical therapists, psychologists.
Dilator Progression
Month 1
- 2 hours of dilator per day. Either in 1 sitting or 1 hour of dilator work x2 per day
- Progress to bigger sizes until #5 or #6 is comfortable
Month 2
- 1 hour of dilator use per day and continue toward larger sizes
Month 3
- 15-30 minutes of dilator use per day
Months 4-12
- 10-15 minutes of dilator use per day or every other day
During the counseling session post-procedure, the recommendations for returning to intercourse included:
- Delaying intercourse until #5 dilator was able to be easily inserted
- It is helpful to do 1 hour of dilator work before attempting intercourse for the first time
- If partner’s penis is larger progress to larger dilators (#7 - 6 inch circumference or #8 7 inch circumference)
- Goal of the first few attempts is to insert tip of dilator only
- Once tip can be inserted easily then progress to full penetration; restrain from thrusting
- Try “spooning position” if ‘leg lock’ occurs
- Try different positions with dilator work and intercourse to see what works best
71% of participants achieved pain-free coitus 5 weeks after the procedure. 2.5% could not achieve coitus within one-year period although they could use #5 or #6 dilators. The participants were given a validated outcome tool, the Female Sexual Function Index (FSFI), before and after the procedure and at 1-month, 3-months, 6-months, and 1-year; with significant improvement at each interval. The patients were followed for one year, and often remained in contact with the authors for much longer ranging from 16-months to 9-years.
The authors propose that use of dilators at the time of botox and post procedure counseling and support help participants ‘break through’, whereas previous treatment may not be as multidimensional and limit efficacy. Botox lasts 2-4 months and allowed for dilation progression.
Initially after reading this article the treatment seemed a little drastic to me, but then I considered the women with this level of vaginismus are often not coming into my clinic. They may need this level of structure, consistently, and multidimensional treatment as half measures have failed them. I am so glad they were persistent and found the help they needed.
Pacik, P., Geletta, S. Vaginismus Treatment: Clinical Trials Follow Up 241 Patients. Sex Med 2017;5:e114-e123
My job as a pelvic floor therapist is rewarding and challenging in so many ways. I have to say that one of my favorite "job duties" is differential diagnosis. Some days I feel like a detective, hunting down and piecing together important clues that join like the pieces of a puzzle and reveal the mystery of the root of a particular patient's problem. When I can accurately pinpoint the cause of someone's pain, then I can both offer hope and plan a road to healing.
 Recently a lovely young woman came into my office with the diagnosis of dyspareunia. As you may know dyspareunia means painful penetration and is somewhat akin to getting a script that says "lower back pain." As a therapist you still have to use your skills to determine the cause of the pain and develop an appropriate treatment plan.
Recently a lovely young woman came into my office with the diagnosis of dyspareunia. As you may know dyspareunia means painful penetration and is somewhat akin to getting a script that says "lower back pain." As a therapist you still have to use your skills to determine the cause of the pain and develop an appropriate treatment plan.
My patient relayed that she was 6 months post partum with her first child. She was nursing. Her labor and delivery were unremarkable but she tore a bit during the delivery. She had tried to have intercourse with her husband a few times. It was painful and she thought she needed more time to heal but the pain was not changing. She was a 0 on the Marinoff scare. She was convinced that her scar was restricted. "Oh Goodie," I thought. "I love working with scars!" But I said to her, "Well, we will certainly check your scar mobility but we will also look at the nerves and muscles and skin in that area and test each as a potential pain source, while also completing a musculoskeletal assessment of the rest of you."
Her "external" exam was unremarkable except for adductor and abdominal muscle overactivity. Her internal exam actually revealed excellent scar healing and mobility. There was significant erythemia around the vestibule and a cotton swab test was positive for pain in several areas. There was also significant muscle overactivity in the bulbospongiosis, urethrovaginal sphincter and pubococcygeus muscles. Also her vaginal pH was a 7 (it should normally be a 4, this could indicate low vaginal estrogen). I gave her the diagnosis of provoked vestibulodynia with vaginismus. Her scar was not the problem after all.
Initially for homework she removed all vulvar irritants, talked to her doctor about trying a small amount of vaginal estrogen cream, and worked on awareness of her tendency to clench her abdominal, adductor, and pelvic floor muscles followed by focused relaxation and deep breathing. In the clinic I performed biofeedback for down training, manual therapy to the involved muscles, and instructed her in a dilator program for home. This particular patient did beautifully and her symptoms resolved quite quickly. She sent me a very satisfied email from a weekend holiday with her husband and daughter.
Although this case was fairly straightforward, it is a great example of how differential diagnosis is imperative to deciding and implementing an effective treatment plan for our patients. In Herman & Wallace courses you will gain confidence in your evaluation skills and learn evidence based treatment processes that will enable you to be more confident in your care of both straightforward and complex pelvic pain cases. Hope to see you in class!
In case you’ve been under a rock (or maybe studying for the Pelvic Rehabilitation Provider Certification (PRPC) exam, the latest Netflix series starring Maria Bamford is out, and it is, as the kids say, amazeballs. We have Maria Bamford and team, and Lady Dynamite, to thank for getting the term vaginismus out in the public as the title of Season 1, Episode 8. The episode is named “A Vaginismus Miracle.” In this episode Maria is answering the question of when she last had sex. She answers that is was a year ago, which reminds her that the annual date of "Vaginismus" must be coming up. Maria further explains that she must have sex once per year because then everything is good "under the hood", and if she doesn't have sex once a year, her "vagina could close up." It's a nail biter of an episode as Maria's assistant has messed up the schedule, and Maria finds out that "Vaginismus" is that very night, and she must find a partner before midnight.
As a pelvic health provider, I knew that neither myself nor my colleagues would be able to sit back and worry about Maria suffering through another year with “Vaginismus” on her calendar, a looming deadline when we all know that with a little bit of rehabilitation, the issue could be much, much better, or maybe resolved altogether. The episode inspired me to write an open letter to Maria. Feel free to share and tag your friends who you think would love to watch a smart, funny show that puts real life issues including mental health in the spotlight.
![]()
Dear Lady Dynamite,
I recently saw your Netflix show and I have to say that it is brilliant. I love how you weave humor, the messiness of life, and important topics into an unpredictable series of events. You are clearly one smart cookie, but I’m not convinced that your new agent, Karen Grisham, is such a great influence on you (or anyone for that matter).
I wanted to reach out and let you know that, as a pelvic rehabilitation therapist and faculty member at the Herman & Wallace Pelvic Rehabilitation Institute, I really appreciate that you brought the term vaginismus into the big time. So many women suffer needlessly because there is so much that pelvic rehab can do for women like you! It does seem that you have figured out a system that works for you, but what if things hadn’t worked out with Scott that night? Hanging out in a bar hoping that you can find someone to hook up with is just so 80’s. Your condition of vaginismus, a tightening of the muscles around your Lady Dynamite parts, does often cause pain with sex, and that’s called dyspareunia. This is a condition that we pelvic rehab specialists treat every day with a heck of a lot of success. Your new boyfriend Scott (he is still your boyfriend after Thanksgiving and all, right?) could even help you overcome some tenderness and tightness by learning to help you release your vaginal muscle tension. Now if that doesn’t sound like great fodder for some stand-up I don’t know what does!
It’s hard to know sometimes why vaginismus starts, maybe it was the years of freezing temperatures in Duluth that led to your tight muscles, or sliding down Chester Bowl on the ice. Maybe it was spending too much time sitting in a wheelchair while medicated, or caused by medication itself (that happens too- even birth control pills can cause pelvic pain!) My point is, there’s no need to put so much pressure on yourself and have this horrible deadline of “vaginismus” hanging over your head when you can see a kind, smart health care provider about the issue. If you, dear Lady Dynamite, need a referral for a great pelvic rehab therapist in your neighborhood, let us know! We train hundreds of therapists every year, and can help you find the perfect fit (pun intended!) Ha! (We know you can handle a little “adult humor.”) Wishing you all the best, and thanks again for talking about your vagina!
Yours in Pelvic Health,
Holly Tanner
P.S. Good luck with the Pussy Noodles representation!
P.P.S Go ‘Toppers!
P.P.P.S Can’t wait for Season 2!
P.P.P.P.S And if you see Mark McGrath around, say “hi” for me!
![]()
So, dear readers, if you would like to enjoy a smart and really funny show, check out Lady Dynamite. And if you want to learn more about vaginismus, Herman & Wallace offers several courses which would be up your alley. Consider joining faculty member Dee Hartmann, PT, DPT at Vulvodynia: Assessment and Treatment - Denver, CO this October 15-16.
Brady, P. & Hurwitz, M. (Creators). (2016). Lady Dynamite: Season 1, Episode 8. Retrieved from http://netflix.com
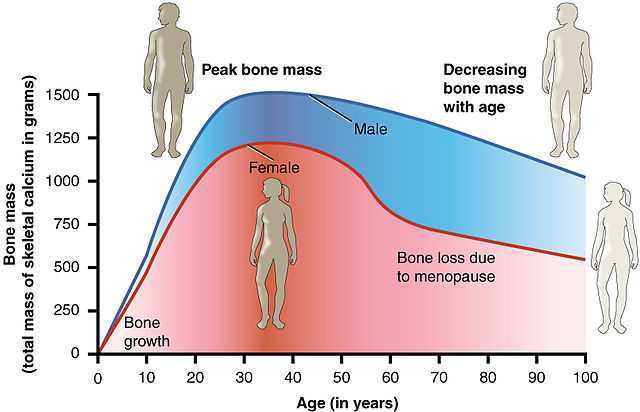
After menopause, more than half of women may have vulvovaginal symptoms that can impact their lifestyle, emotional well being and sexual health. What's more, the symptoms tend to co-exist with issues such as prolapse, urinary and/or bowel problems. But unfortunately many women aren't getting the help they need, despite a growing body of evidence that skilled pelvic rehab interventions are effective in the management of bladder/bowel dysfunctions, POP, sexual health issues and pelvic pain.
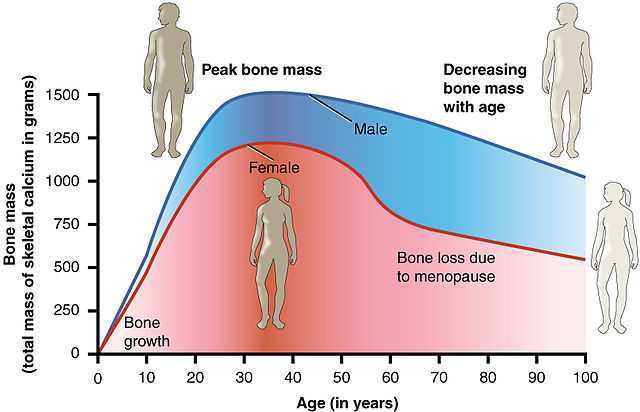 Vaginal dryness, hot flashes, night sweats, disrupted sleep, and weight gain have been listed as the top five symptoms experienced by postmenopausal women in North America and Europe, according to a study by Minkin et al 2015, and they also concluded ‘The impact of postmenopausal symptoms on relationships is greater in women from countries where symptoms are more prevalent.’ Between 17% and 45% of postmenopausal women say they find sex painful, a condition referred to medically as dyspareunia. Vaginal thinning and dryness are the most common cause of dyspareunia in women over age 50. However pain during sex can also result from vulvodynia (chronic pain in the vulva, or external genitals) and a number of other causes not specifically associated with menopause or aging, particularly orthopaedic dysfunction, which the pelvic physical therapist is in an ideal position to screen for.
Vaginal dryness, hot flashes, night sweats, disrupted sleep, and weight gain have been listed as the top five symptoms experienced by postmenopausal women in North America and Europe, according to a study by Minkin et al 2015, and they also concluded ‘The impact of postmenopausal symptoms on relationships is greater in women from countries where symptoms are more prevalent.’ Between 17% and 45% of postmenopausal women say they find sex painful, a condition referred to medically as dyspareunia. Vaginal thinning and dryness are the most common cause of dyspareunia in women over age 50. However pain during sex can also result from vulvodynia (chronic pain in the vulva, or external genitals) and a number of other causes not specifically associated with menopause or aging, particularly orthopaedic dysfunction, which the pelvic physical therapist is in an ideal position to screen for.
According to the North America Menopause Society, ‘…beyond the immediate effects of the pain itself, pain during sex (or simply fear or anticipation of pain during sex) can trigger performance anxiety or future arousal problems in some women. Worry over whether pain will come back can diminish lubrication or cause involuntary—and painful—tightening of the vaginal muscles, called vaginismus. The result can be a vicious circle, again highlighting how intertwined sexual problems can become.’
The research has demonstrated that the optimal strategy for post-menopausal stress incontinence is a combination of local hormonal treatment and pelvic floor muscle training – the strategy of combining the two approaches has been shown to be superior to either approach used individually (Castellani et al 2015, Capobianco et al 2012) and similar conclusions can be drawn for promoting sexual health peri- and post-menopausally.
The pelvic rehab specialist may be called upon to screen for orthopaedic dysfunction in the spine, hips or pelvis, to discuss sexual ergonomics such as positioning or the use of lubricant as well as providing information and education about sexual health before, during and after menopause.
To learn more about sexual health and pelvic floor function/dysfunction at menopause, join me in Atlanta in March for Menopause: A Rehab Approach.
Prevalence of postmenopausal symptoms in North America and Europe, Minkin, Mary Jane MD, NCMP1; Reiter, Suzanne RNC, NP, MM, MSN2; Maamari, Ricardo MD, NCMP3, Menopause:November 2015 - Volume 22 - Issue 11 - p 1231–1238
Low-Dose Intravaginal Estriol and Pelvic Floor Rehabilitation in Post-Menopausal Stress Urinary Incontinence, Castellani D. · Saldutto P. · Galica V. · Pace G. · Biferi D. · Paradiso Galatioto G. · Vicentini C., Urol Int 2015;95:417-421