This blog contains excerpts from an interview with Pamela A. Downey, PT, DPT, WCS, BCB-PMD, PRPC, Pamela is a Board Certified Clinical Specialist in Women’s Health Physical Therapy and Board Certified in Biofeedback for Pelvic Muscle Dysfunction. She is the owner of Partnership in Therapy, private practice in Coral Gables, Florida. Dr. Downey's treatment focuses are pelvic floor dysfunction, urogynecological and colorectal issues, spine dysfunction, osteoporosis, and complaints associated with pregnancy and postpartum. Her mission is to educate and integrate healthy lifestyles for patients on the road to wellness.
Physical therapists often require special training to treat pudendal neuralgia. Pamela A. Downey is partnering with H&W to teach the Pudendal Neuralgia and Nerve Entrapment Remote Course, scheduled for June 19-20, 2021. This course teaches pudendal neuralgia diagnostic skills for practitioners to have an improved impact in treating patients with pudendal nerve/pelvic floor muscle dysfunctions.
Pudendal neuralgia is also known as Alcock’s syndrome, pudendal canal syndrome, or cyclist syndrome. This condition is caused by tension, compression, or entrapment of the pudendal nerve, and leads to pelvic pain, sexual dysfunction, difficulty with urination and defecation, among other issues.
Pudendal neuralgia is often unrecognized by physicians, including gynecologists, urologists, and neurologists. Dr. Downey observes that “Organizing your clinical decision-making process is key in determining the source of seated pain. Pudendal neuralgia can be a chicken and egg clinical phenomenon. My success comes from relying on a solid anatomy background in helping solve the pudendal puzzle.”
Successful treatments can include connective tissue mobilization, neural mobilization, and a home exercise program. Poor movement patterns can contribute to the symptoms of pudendal neuralgia. Physical therapy evaluation in these cases can include movement assessment and a gentle internal assessment of the patient's pelvic muscles. This provides information about the muscles’ ability to contract and relax. Exercises recommended to relax the pudendal nerve and provide temporary relief include cobra pose, side-lying hip abduction and extension, and wide-leg bridges.
Dr. Downey shares that she loves teaching the Pudendal Neuralgia and Nerve Entrapment Remote Course. “We teach the participants, in real-time, how to use evidence-based criteria to see if pudendal neuralgia makes sense as the driving diagnosis. Then we develop this confidence by careful dissection of case studies of real patients treated out over multiple visits, just like you do in the clinic."
Hone your decision-making process and gain confidence in the Pudendal Neuralgia and Nerve Entrapment Remote Course to treat pelvic pain with Pamela Downey on June 19-20, 2021.

Working with Physiatry for Pelvic Pain is a new remote course created by Dr. Allyson Shrikhande, scheduled for Jun 27, 2021. This course overviews the synergistic nature of pelvic physiatry with pelvic floor physical therapy, in hopes of promoting collaboration for the care of male and female chronic pelvic pain patients.
Dr. Allyson Shrikhande is a board-certified Physical Medicine and Rehabilitation specialist and is the Chair of the Medical Education Committee for the International Pelvic Pain Society. Allyson has published peer-reviewed articles on the treatment of muscle pain in academic journals and works closely with renowned pelvic pain gynecologists and urologists. Taking a team approach, she works with specialists in pelvic floor physical therapy, kinetics and movement, as well as acupuncturists, nutritionists, cognitive-behavioral therapists, and functional medicine physicians.
The following is our interview with Allyson Shrikhande on physiatry.
Q: What is a physiatrist?
A: A physiatrist is an MD or DO with a specialty in Physical Medicine and Rehabilitation. This non-operative medical discipline involves focusing on the neuromusculoskeletal system to help patients recover their functional well-being and quality of life. We describe physiatry as an extension of physical therapy because a physiatrist diagnoses, manages, and treats pain from injury, illness, or medical conditions, incorporating other methods in concert with physical therapy to rehabilitate the body. Physiatrists are trained not solely in one organ system – rather, they take a holistic, full-body approach that accounts for the interplay of different organ systems, both with each other and with the neuromuscular and myofascial systems.
Q: What does a physiatrist do?
A: Physiatrists work with physical therapy to rehabilitate the neuromuscular system. A core underlying theme in physiatry is the concept of Neuroplasticity. This is the understanding that the nervous system has the ability to form and reorganize synaptic connections, especially in response to experience or learning following injury.
Q: What do physiatrists treat?
A: Because physiatrists focus on the interconnected systems of the entire body, they treat a wide range of injuries and disorders. Physiatrists commonly work with patients who have pelvic, back or neck pain who are recovering from issues such as sports injuries, neuromuscular disorders, arthritis, or injuries to the brain or spinal cord.
Q: Why would I see a physiatrist?
A: At Pelvic Rehabilitation Medicine, our Pelvic Physiatrists diagnose and treat the structures of the pelvis – the muscles, nerves, and joints. One of our physiatrists can provide non-operative options to medically manage and treat pelvic pain and pelvic floor muscle dysfunction. We treat an array of symptoms under the umbrella of pelvic pain which includes pain with intercourse, urinary urgency/frequency or pain with urination, constipation or painful bowel movements, and pain affecting the coccyx, groin, pelvis, lower back, and lower abdomen.
Q: As a pelvic floor physical therapist, what can I learn from a physiatrist?
A: The relationship between physiatry and physical therapy is vital to the collaborative approach that our pelvic pain patients require. Physiatrists perform a full neuromuscular exam (including an internal pelvic floor exam) and can order imaging, prescribe oral medications, suppositories, and topical medications for some patients. Our physiatrists can also perform safe outpatient ultrasound-guided procedures to treat underlying neuromuscular dysfunction, all in combination with continued pelvic floor PT when appropriate.
Megan Pribyl, PT, CMPT is a practicing physical therapist at the Olathe Medical Center in Olathe, KS treating a diverse outpatient population in orthopedics including pelvic rehabilitation. Megan’s longstanding passion for both nutritional sciences and manual therapy has culminated in the creation of her remote course, Nutrition Perspectives for the Pelvic Rehab Therapist, designed to propel understanding of human physiology as it relates to pelvic conditions, pain, healing, and therapeutic response. She harnesses her passion to continually update this course with cutting-edge discoveries creating a unique experience sure to elevate your level of appreciation for the complex and fascinating nature of clinical presentations in orthopedic manual therapy and pelvic rehabilitation.
As a course developer and instructor for the Herman & Wallace Pelvic Rehab Institute, it is a privilege to continue sharing my passion for nutrition and pelvic rehabilitation with professionals nationwide. Interest in the topic continues to grow, and many pelvic rehab providers have identified nutrition as the “missing link” in their clinical practice. Nutrition Perspectives for the Pelvic Rehab Therapist has helped hundreds of pelvic rehab professionals integrate nutrition-related information into their clinical practice since 2015.

In the realm of nutrition, few questions provoke discussion with the same fervor as our title question: Organic Food vs. Conventional: Is There Any Difference? This question deserves a multi-dimensional answer - not unlike many topics in nutrition - including accessibility concerns, ethical factors for farmers, socio-economic factors, and our unique agricultural construct here in the United States. But the question about organic vs. conventional might just be the most important one deserving a thoughtful discussion to unravel the complexities around the topic of food.
You see, the answer to this question has profound implications for us. As we expand our ability to identify potential root contributors to conditions commonly encountered in pelvic rehabilitation, we must factor in nutrition. At first glance, it might be a stretch to see how one might link organic foods and potential effects on conditions such as constipation, inflammatory bowel diseases, IBS, PBS, and endometriosis for example. However, looking at food in a functional way, we acknowledge there may be under-appreciated qualitative differences between foods grown organically or produced conventionally.
Take, for example, the recent article by Kesse-Guyot et.al., 2020. which discusses the prospective association between organic food consumption and the risk of type 2 diabetes. In this study of over 30,000 participants, those with the highest quintile of organic food consumption compared to those with the lowest quintile had a 35% lower risk of having type 2 diabetes. The conclusion made by the authors was that organic food consumption was inversely associated with the risk of type 2 diabetes.
Said a different way, the study described a phenomenon where, for example, you might eat an organic bowl of oatmeal for breakfast and I might eat the same serving size conventional bowl of oatmeal for breakfast. If we extrapolate the comparison over our entire dietary intake pattern, you would have a 35% lower risk for developing type 2 diabetes compared to me…..despite you and I “eating the same foods”. How can this be possible? And might this begin to explain the sheer exasperation and frustration that can evolve in persons trying to make positive dietary changes - only to find they have no notable effect? How many times do you hear someone say “I am trying to eat healthily but it doesn’t seem to make a difference”.

Keeping in the context of type 2 diabetes, it is very well established that reductions in the richness and diversity of healthy microbes inhabiting the large intestine (gut dysbiosis) are correlative to metabolic syndrome. In those with type 2 diabetes, microbiomes showed a decrease in anti-inflammatory, probiotic, and other [beneficial] bacteria that could be pathogenic. (Das et al, 2021) Appreciating the differences between organic vs conventional - it is also well established that organic foods do carry less residue of herbicides and pesticides. These residues - which are found in higher concentration in conventionally produced foods - have been implicated in the same reduction in richness and diversity of microorganisms in the gut - which is contributory to dysbiosis. (Rueda-Ruzafa et all, 2019) Therefore it now seems not just plausible - but probable that there is a distinguishable difference between organic and conventional diets - to a degree at which all health care providers would do well to take notice.
In a report on the history of organic agriculture, author George Kuepper points out that:
“Pioneers of the organic movement believed that healthy food produced healthy people and that healthy people were the basis for a healthy society.”
And if organic foods can be a part of that, our patients deserve to know that these scientifically documented differences exist.
As our awareness of the connection between nutrition and health grows, so does the need to follow the science to share evidence-based and evidence-informed information. It is now more important than ever to have a working knowledge of nutrition basics as a pelvic rehabilitation professional. Plan to join us at one of our upcoming remote offerings of “Nutrition Perspectives for the Pelvic Rehab Therapist”: June 19-20 where we will explore this and many additional - and fascinating facets of the nutrition discussion.
Das, T., Jayasudha, R., Chakravarthy, S., Prashanthi, G. S., Bhargava, A., Tyagi, M., . . . Shivaji, S. (2021). Alterations in the gut bacterial microbiome in people with type 2 diabetes mellitus and diabetic retinopathy. Sci Rep, 11(1), 2738. doi:10.1038/s41598-021-82538-0
Kesse-Guyot, E., Rebouillat, P., Payrastre, L., Alles, B., Fezeu, L. K., Druesne-Pecollo, N., . . . Baudry, J. (2020). Prospective association between organic food consumption and the risk of type 2 diabetes: findings from the NutriNet-Sante cohort study. Int J Behav Nutr Phys Act, 17(1), 136. doi:10.1186/s12966-020-01038-y
Kuepper, George. (2010) A Brief Overview of the History and Philosophy of Organic Agriculture. Kerr Center for Sustainable Agriculture. http://kerrcenter.com/wp-content/uploads/2014/08/organic-philosophy-report.pdf Accessed May 14, 2021.
Rueda-Ruzafa, L., Cruz, F., Roman, P., & Cardona, D. (2019). Gut microbiota and neurological effects of glyphosate. Neurotoxicology, 75, 1-8. doi:10.1016/j.neuro.2019.08.006
Images:Par, Cecilia for Unsplash.
USDA organic seal.svg. Public Domain.

Deb Gulbrandson, PT, DPT has been a physical therapist for over 42 years with experience in acute care, home health, pediatrics, geriatrics, sports medicine, and consulting to business and industry. Dr. Gulbrandson frequently presents community talks on topics related to Osteoporosis and safe ways to develop Core Strength. She is a member of the APTA Geriatric and Private Practice Sections, a Certified Osteoporosis Exercise Specialist using the Meeks Method, and is a CEEAA (Certified Exercise Expert for the Aging Adult) through the Geriatric Section of the APTA.
Hello, my name is Deb Gulbrandson. May is National Osteoporosis Month, and my colleague, Frank Ciuba, and I are creators of the upcoming remote course Osteoporosis Management on June 12-13, 2021.
Did you know that approximately half of all women and a quarter of all men will break a bone due to osteoporosis? Equally disheartening, every year about one-third of adults in the US age 65 and older will fall. Many of these falls will result in broken bones.
Frank and I developed the Osteoporosis Management course to bring treatment protocols to practitioners in an organized and easily implementable format. This course is based on the Meeks Method created by Sara Meeks, PT, MS, GCS, with whom Frank and I taught for several years. With Sara’s blessing, we have branched out to add information on sleep hygiene, exercise dosing, and basic nutrition for a person with low bone mass. Knowing how to recognize signs, screen for osteoporosis, and design an effective and safe program can be life-changing for these patients.
In all likelihood, you are working with osteoporosis patients right now whether you know it or not. Osteoporosis affects all ages and stages of life including young and middle-aged men and women. Often we see patients with orthopedic or neurologic diagnoses who also have osteoporosis- known or unknown. Being able to address patients’ comorbidities helps ensure safety and quality of life. Many of the techniques we use can apply across several patient demographics. After all, who doesn’t benefit from postural alignment, back extensor/glute strengthening, and balance activities?
Working with this population has been extremely rewarding, because similar to pelvic health patients, these patients have been told there’s nothing you can do about it. They are incredibly grateful to find out that there IS something you can do about osteoporosis. They enthusiastically take an active role in their rehabilitation.
In addition, as a private practice owner for over 30 years, I’ve found osteoporosis to be a great business opportunity. An incredible niche practice, bringing in patients who have actively sought out my clinic with their self-referrals or by word of mouth.
We hope that you will join us this June 12-13 for our course Osteoporosis Management for an opportunity to experience posture, power, visual cueing, strengthening, and balance activities along with osteoporosis screening, evaluation, and evidence-based practice.

In this blog, instructor Heather Rader, PT, DPT, PRPC, BCB-PMD, discusses the concerns and fears therapists have when treating mothers recovering from childbirth and how her upcoming course can prepare therapists to confidently treat patients within hours to weeks after childbirth.
When is it OK for a new mom to start therapy?
When a new pelvic therapist asks me this question at courses, my answer begins by shifting the focus towards the birth itself. Childbirth is a mechanism of injury, not a “special population.” The real question then is when is it OK to start therapy after perineal or abdominal tissue trauma? When your clinical reasoning begins from this point of view, it removes biases you may have about childbirth and instills confidence in your skills as a trained clinician. Every therapist learns acute care skills - how to treat wounds, how to mobilize post-op patients, and how to screen for medical complications. Simply put, dear clinician, you know more than you think you do.
On average, 3.75 million women give birth in the US per year (1.) 100% will have some level of injury because of it. Those injuries will be perineal, abdominal, or both. There will be muscle strains and ligamentous sprains. There will be soft tissue bruising and swelling.
There are risks of immobility and re-injury without proper patient education. There might be stitches or staples in the abdominal or vulvar skin. There will be pain issues, mobility issues, safety issues, and definitely body mechanics and ergonomic issues. Given these obvious musculoskeletal and mobility impairments, I ask you to ponder this - what profession is better prepared to assess the acute and sub-acute needs of a new mother than rehab professionals?
Let’s imagine the same question posed to an acute care therapist about newly injured trauma patients.
Every lecture on the history of rehabilitation highlights the early days when bed rest was thought to be therapeutic.
Through research and clinical observations, we know immobility was, in some cases, deadly. Nowadays, it is considered standard of care to begin mobilization as early as medically possible, even in the ICU. And so should it be with new mothers. When should a person who was in an accident start rehab? What information would our therapist need to determine when to start and what early intervention is medically appropriate?
- Is the patient medically stable?
- Are the injured tissues structurally stable?
- Have any problems developed as a result of being immobilized in the hospital?
- Are there other co-morbidities to complicate the recovery?
- How is the patient’s mental status after the trauma?
- What social support is in place to assist with short-term and long-term needs?
- Can the patient function independently? Need home health? Benefit from outpatient therapy?
The clinical decision-making and critical thinking necessary to manage the care of an acute care patient is not much different than that of a pelvic therapist managing the recovery of a new or “acute” mother. More and more hospitals and birthing centers are incorporating acute care therapy within hours of birth. There are anatomical and physiological differences because of the effects of pregnancy itself that the clinician must learn, however. While the patient is recovering from childbirth, the body is returning to its pre-pregnancy state. Having a better understanding of the late pregnancy, birth, and the peripartum state has on healing can assist the motivated clinician in adding maternal-based therapy to their skill set.
The course Peripartum Advanced Topics covers medical screening, early exercise, patient education, hospital-based programming, and treatment strategies, as well as early outpatient care and fitness transition planning, such as returning to running.
If you are contemplating expanding your outpatient practice to see patients early in the “4th Trimester” or even earlier in the acute setting after the 4th stage of labor (recovery), consider signing up for the course.
- 1. https://www.cdc.gov/nchs/fastats/births.htm accessed 5/19/2021 10:30 AM

Mia Fine, MS, LMFT, CST, CIIP has written and instructing her remote course, Sexual Interviewing for Pelvic Health Therapists, with H&W on June 5-6, 2021. Mia (they/she) is a student of Queer Theory, Intersectionality, and Social Justice, and offers holistic, anti-oppressive, and trauma-informed therapy. This is a course intended for pelvic rehab therapists who want to learn tools and strategies from a sex therapist’s toolkit who work with patients experiencing pelvic pain, pelvic floor hypertonicity, and other pelvic floor concerns.
Let’s talk terms: Dyspareunia and Vaginismus
- Vaginismus: involuntary contraction of vaginal muscles preventing insertion/penetration
- Dyspareunia: pain felt during penetration
Symptoms (not limited to): pain - painful penetration, painful orgasms, painful periods, painful pelvic exams, inability to use tampons/cups, urinary or bowel hesitancy, feeling “too tight”
Causes (not limited to): stress, relationship concerns, mood concerns (anxiety, depression), insufficient arousal/desire/interest, trauma, side effects of meds, negative attitudes towards sex, and other pelvic pain concerns such as a tilted uterus.
The deal is, when it comes to dyspareunia and vaginismus there’s a cycle that can be difficult to break. The cycle is: you feel pain, then you feel broken (shame about feeling pain), then anxiety that pain will happen again, then you tighten your pelvic floor, and the cycle repeats. It becomes a self-fulfilling prophecy.
Often unwanted sexual pain goes unaddressed. Why? Because we are not taught about the interactions between feelings, relationships, and our body. We are not taught that sex should not be painful; that pain is (likely) our body giving us information that something is going on (Hello crappy sex education and the stigma of sexual health and body awareness!). It’s not uncommon that most people who experience sexual pain often feel they are broken.
You are not broken
How to heal from unwanted sexual pain? There’s a trifecta! Effective healing comes from working with a sex-positive medical provider, sex therapist, and pelvic floor PT. We will all collaborate!
Sex is not supposed to be painful. You are not broken.
Mia ️
#therapy #sextherapy #wellness #health #awareness #mentalhealth #bodyawareness

Steve Dischiavi holds credentials as a licensed physical therapist and a certified athletic trainer. He also has a manual therapy certification from the Ola Grimsby Institute and is board certified by the American Physical Therapy Association as a Sports Clinical Specialist (SCS).
The blog you’re about to read is targeted at clinicians just like myself. I was taught in PT school to evaluate the sacroiliac joint (SIJ) via a movement-based analysis. I even went on for a certification in manual therapy nearly 2 decades ago, and again was taught the movement-based approach. Well, as the song goes… “times they are a changin”….
So… if you’re a clinician who will diagnosis the SIJ as being “unstable” from movement-based testing, using tests that evaluate the positional movement of the PSIS… then you need to begin to question the approach you’re taking.
There is a contemporary conversation taking place within the field of physical therapy. If you’re like me and learned to evaluate the sacroiliac joint (SIJ) through movement-based testing, you need to be involved in this evolving conversation.
A great place to start is with a “Perspective” article published in Physical Therapy in 2019. It is titled “Changing the Narrative in Diagnosis and Management of Pain in the Sacroiliac Joint Area” written by Thorvaldur Palsson, et.al.1
The narrative dives into several areas pertaining to the treatment of this mysterious region of the body. It gives the reader a thoughtful and contemplative view of the contemporary conversation surrounding the evaluation and treatment of the SIJ.
The target audience should be the clinicians who continue to evaluate the SIJ solely on movement based analysis, attempting to diagnosis the SIJ with terms related to movement dysfunction. We have all heard terms like “upslip, downslip, or sacral torsions”. The narrative addresses why this is not the best approach to diagnosing the SIJ.
The article also touches on the concepts of “pain science” and how assessing how the SIJ “moves” tells the clinician very little about why the tissues about the SIJ might be sensitized. The article scratches the surface about the patient’s pain experience and how harmful terms such as “instability” and how the SIJ “goes out” are ways that can perpetuate and even heighten the pain experience for your patients.
The Perspective article gives the reader a great introduction as to why you might consider altering your approach to the SIJ. I’ll leave you with a quote directly from the article:
“If clinical decisions are based on a construct that lacks plausibility and clinical tests lacking in validity and reliability, the entire management paradigm must be questioned.”
The next question you might be asking yourself… ok, how do I learn a new management paradigm? A great start would be to take the 4-hour introductory webinar, Sacroiliac Joint Current Concepts - Remote Course - June 26, 2021, offered by Herman and Wallace… learn the evidence-based approach to the SIJ with Steve Dischiavi, PT, DPT, MPT, SCS, ATC, COMT who has been working closely on the hip and pelvis for over 20 years!
I hope to see you at the webinar!
1. Palsson TS, Gibson W, Darlow B, et al. Changing the Narrative in Diagnosis and Management of Pain in the Sacroiliac Joint Area. Phys Ther. 2019;99(11):1511-1519.

Dustienne Miller is the creator of the two-day course Yoga for Pelvic Pain. Dustienne passionately believes in the integration of physical therapy and yoga in a holistic model of care, helping individuals navigate through pelvic pain and incontinence to live a healthy and pain-free life.
I’m one of the small business owners who has survived this difficult time. Day after day I would mask up, put on the filtration systems, and be filled with gratitude that I could still safely do my work in the world. Despite being vigilant on sleep, eating lots of veggies from the local farm, exercising, and staying well hydrated I still carry a deep covering of stress and tension.
We have been holding our breath literally and figuratively with collective humanity for the past year. I realized when I had an acute flare of lumbopelvic pain that I had to melt away layer by layer of holding tension in both my back and ribs and go deeper into my breathwork and meditation practice.
I share this to acknowledge that as health care providers we are caring for more than just the physical concerns of our patients. We are honored to witness their grief, which could be from any type of trauma (physical, medical, etc). We are chosen to be their trusted source of advice which often goes beyond the rehab lens. We also need to notice when we as clinicians (and humans experiencing a global pandemic) experience burnout.
We teach our patients how breathing patterns inform our digestion, our spine, our emotional state, our pelvic floor, etc. It’s one of the most powerful tools we have to inform our system that we are safe. Despite this knowledge, we will often find ourselves holding our breath or breathing in non-optimal ways without even realizing it. When we don’t want to feel something we don’t breathe. When we are afraid we hold our breath. We might even find our ribs stay tight even when we feel relaxed.
Let’s pause to notice and soften.
Notice your body without “fixing” your posture. Where is your ribcage in relationship to your pelvic floor? What does it feel like when you breathe in? What does it feel like when you breathe out?
If you are sitting, slouch down. How does breathing feel in this position? Now imagine your head is getting magnetically pulled up towards the ceiling and sit in a more lengthened position. Take a breath with a taller spine. Does it feel different?
Now try this with your eyes closed: imagine the intercostal space widens with each inhale - then softens during each exhale. Do you have a habit of holding your ribs open with tension? Picture your shoulders softening, as if the tension from the upper traps was melting away. The jaw softens, the tongue softens, the center of the forehead softens.
Now take another long, conscious breath. What do you notice?
As practitioners, we give so much to our patients. It serves us to stay grounded in our bodies and as relaxed as we can be while we work. It’s a tall order and hard to remember but it might help decrease fatigue, exhaustion, physical pain, and burnout. Let’s all try and keep our breaths long, jaws soft, and pelvic floors pliable. I hope this pause was useful for you!
Dustienne Miller can be found teaching her course Yoga for Pelvic Pain online for 2021 on the following dates:
May 15-16, July 31-Aug 1, and Sept 25-26

;Aparna Rajagopal, PT, MHS is the lead therapist at Henry Ford Macomb Hospital's pelvic dysfunction program, where she treats pelvic rehab patients and consults with the sports therapy team. Her interests in treating peripartum patients and athletes allowed her to recognize the role that breathing plays in pelvic dysfunction. She has co-authored the course, "Breathing and the Diaphragm: Pelvic and Orthopedic Therapists", which helps clinicians understand breathing mechanics and their relationship to the pelvic floor.
A few months ago a young woman with a diagnosis of dyspareunia was referred to me. She had been a gymnast through her teens and now worked out regularly. She reported being unable to use tampons throughout her life, experiencing difficulty with undergoing pelvic examinations, and inability to have intercourse with her partner all through her married years. She also had a history of long-standing constipation and urinary symptoms including increased voiding frequency and the feeling of incomplete emptying.
Her examination included significant overactivity of her abdominals. A very chest dominant pattern of breathing with very limited lower lateral costal expansion, limitations in thoracic mobility, a fairly rigid rib cage with a very narrow infra sternal angle, connective tissue restrictions of the abdominal, pelvic areas, decreased flexibility of her hamstrings, and weakness of her Glut Max muscles. There was significant guarding and an internal assessment of pelvic floor muscles was not performed initially due to associated discomfort.
Throughout the first few sessions, we worked on releasing her first rib, the scalenes, latissimus dorsi, and quadratus lumborum muscles, and worked on reducing the connective tissue restrictions in the abdominal and pelvic regions. We also spent time improving rib cage and thoracic spine mobility and reducing the chest dominant pattern of breathing; while trying to establish improved abdominal compliance and lateral costal expansion with inhalation. All this, along with techniques aimed at improving neuromuscular control of her Gluteus Maximus without excess compensatory pelvic floor muscular assistance led to enough improvement in a few sessions to allow for an internal pelvic floor muscle assessment to be performed.
The patient's job activities required constant vocalization and I found that she contracted her neck, her abdominal, and pelvic floor muscles very strongly with any vocalization and did not relax the muscles after she finished vocalization. The patient was educated on softening her vocalization, and on a more controlled release of air through the glottis with more gradual abdominal and pelvic floor contractions while performing glottal/vocalization exercises. The patient was very keen on continuing her fitness-related activities through all of her therapy. Manual internal pelvic floor muscle assessment performed with standing activities revealed that although she did not particularly find her workout routine very taxing she tended to exhale extremely forcefully with each repetition of the exercise. This forceful exhale was naturally accompanied by very strong recruitment of her abdominals and her pelvic floor muscles, and once again there was decreased relaxation after cessation of her exercises. The treatment process involved making the patient aware of breath patterns and her gripping, nonrelaxing quality of the contractions of the pelvic floor and the abdomen and how she could gain some relaxation by utilizing her breath.
In addition to continuing to receive pelvic therapy from me, the patient consulted with Leeann, a sports-trained therapist, for 2 sessions to set up a fitness program. Leeann set up a program for the patient to strengthen her core and gluteal muscles while monitoring the pelvic floor externally. The fitness program progressed with challenging exercises in non-weight bearing and quadruped positions which were then progressed to kneeling and then standing. An important focus during the development of this program was on monitoring the patient's strength of exhaling and ensuring pelvic floor relaxation with breathwork between repetitions ensuring that there was no reverting to the old habit of gripping.
The patient's complaints for which she initially sought pelvic therapy were completely resolved. The patient's pelvic pain symptoms were resolved with treatment directed at the thorax, the breath, vocalization and the glottis, and lower extremity muscle strength. Very little time was spent on conventional manual techniques applied directly to the pelvic floor musculature.
In the Herman and Wallace course, you will learn skills to effectively assess the thorax, the diaphragm, breathing patterns, thoracic mobility inclusive of joint mobility, and myofascial connections. Come and learn how postural changes can affect the biomechanics of how the body performs and in turn affect intra-abdominal pressure. Learn easy effective strategies that will help you in your care of patients with low back pain and pelvic floor dysfunction the very next day. Hope to see you in class!
;Aparna Rajagopal will be co-teaching Breathing and the Diaphragm: Pelvic and Orthopedic Therapists on May 15-16, 20201 with her colleague Leeann Taptich. This course instructs practitioners on breathing mechanics and their relationship to the pelvic floor.
This is Part 2 of Tuesday's, April 27, 2021, blog Misbehaving Bladders and Cluster Drinking - A Novel Approach, Part 1.
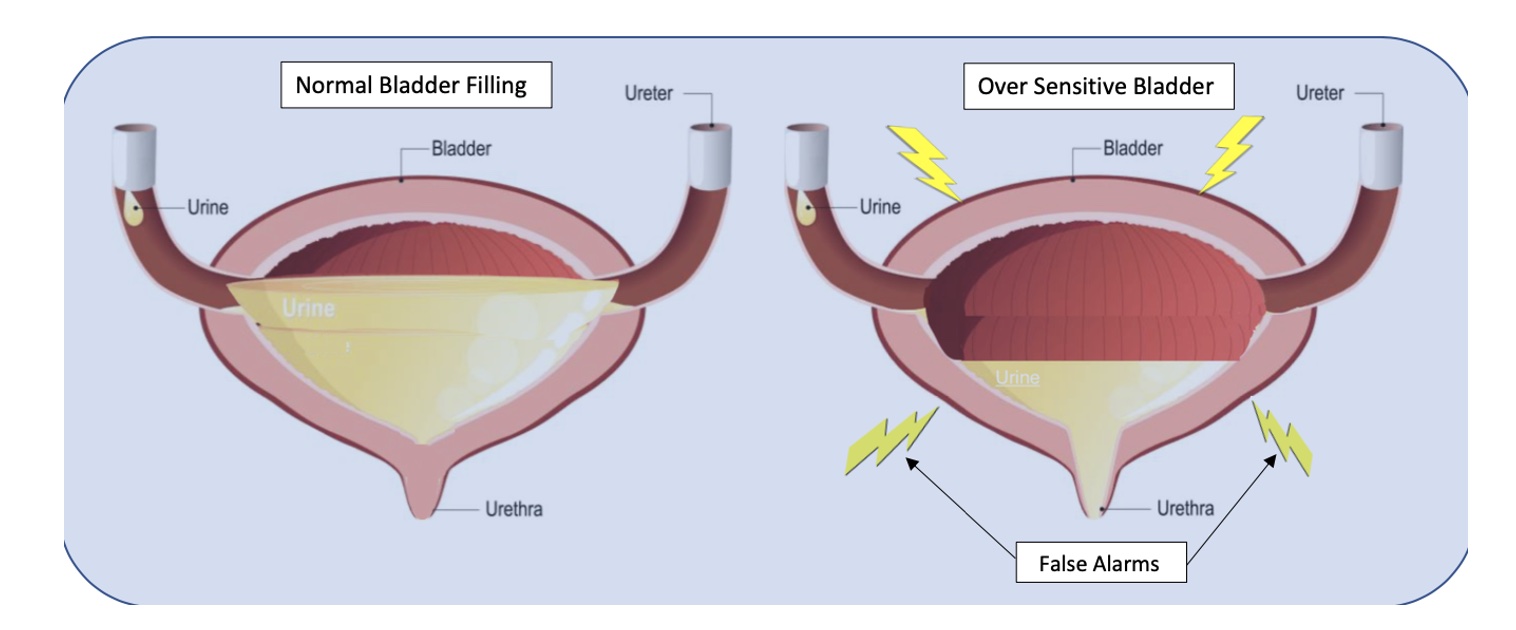
Bladder capacity ranges from around 400-500ml (13-16 oz). The use of a measuring cup or water bottle can be very helpful to teach this concept. We certainly don’t have to strive for a full bladder volume, but it is important to illustrate that 2-3 ounces are in fact “just in case” voids. I explain to patients that in situations of overactive or irritated bladders, the receptors in their bladder walls are hypersensitive and sending “false alarm” messages when only a small amount of urine is present. The kidneys are always active and refilling the bladder, so it will never be totally empty per se, therefore it must be desensitized and retrained to be a viable, reliable, and reasonably comfortable storage vessel.
With the Cluster Drinking Approach, it is important to try and drink the fluid in a short enough period of time to ensure an increased rate of bladder filling for this to be effective, but you must be careful to monitor the bladder irritability with the training. A fuller bladder will experience more pressure, but this also helps with urine flow during voids. We then embark on this process of retraining and using their bladder diaries to help us with detective work to determine optimal amounts of fluid intake in each cluster and the optimal timing of fluid intake, number of clusters, etc. for their daily schedules. It may take some time to get used to the new habits. It can be hard for some patients who are used to sipping on their water bottle all day long, and they can feel dehydrated. This is a habit and learned response and can be retrained with some gradual investment in the process. Once patients experience the rewarding outcomes, they are usually willing to make the changes.
Based on diary findings, we modify types of fluids as necessary, my motto being: minimal disruption to achieve desired results. Why give up coffee and all favorite beverages if not necessary? Sometimes making modifications on timing and amount of intake works just fine, other times we tweak the beverage types. I also teach and integrate urge suppression strategies (USS) as well, to help with the process of retraining; and of course, address breathing, pelvic floor dysfunctions, connective tissue restrictions, and chronic constipation, but the variable which sets this approach apart is the cluster drinking.
According to Washington state urogynecologist Elizabeth A. Miller, MD FPMRS, a practitioner at Overlake and Swedish Medical Centers, the Cluster Drinking Approach works similarly to some OAB medications in training your bladder to hold more urine. She endorses the Cluster Drinking Approach as a viable first-line treatment option since it works naturally without harmful side effects. Results are often profound and rapid even for folks who have been struggling with these bladder issues for years. Likewise, leaking issues tend to diminish as the bladder training is mastered. Patients can structure riskier activities around this cluster program, i.e. plan their Zumba after cluster intake and output. The same goes for major outings where one will not be near a bathroom. Even my constipation patients have benefitted due to a more reliable intake of adequate fluid.
Nocturia is a bit of a different situation because of the role of kidney hormones, but I have found this approach to be quite effective for many patients whose lives and sleep are impacted by this problem. The Cluster Drinking Approach helps these patients to structure their fluid intake during daytime hours, and I teach them to heed the 1st overnight urge if it is within 2-3 hours after going to sleep. Then if they awaken again, I coach them to use the mantra “the bladder is a storage vessel”, analyze their last intake and output, and permit themselves to use the Urge Suppression Strategies, and go back to sleep without worrying that their bladder will explode. The other good news is after their bladders (and brains) are “retrained”, and you have done your PT magic, they can often return to more natural drinking patterns without negative consequences.
Fun Fact: Even Did you know that under anesthesia the amazing expandable bladder can hold over 1 liter?!
Kathy E. Golic, PT is a physical therapist at Overlake Hospital Medical Center in Bellevue, Washington.