Many therapists start their career feeling a bit intimidated to work with women who are pregnant. A common and understandable concern is that something the therapist will do during examination or treatment may harm the patient. While there are certainly things to avoid when working with a patient who is pregnant there are also many therapeutic strategies that can help a woman thrive during her pregnancy and beyond. When women have pre-existing issues such as a disease or physical challenge, or when she develops an illness during pregnancy, the therapist needs to rely upon more knowledge- this knowledge is something she rarely learns in school, but more likely in continuing education environments. A recent article asked the question “are women getting sicker, and are there more high-risk pregnancies now than ever before?”
 Researchers studied trends in maternal morbidity and mortality in the United States in order to answer this question, and the answer is a definitive “yes”. Several studies describe increases in the rates of maternal morbidity, with issues such as cardiac and pulmonary complications, and the severe blood pressure fluctuations associated with eclampsia. Gestational diabetes, and postpartum rates for hemorrhage, perineal lacerations, and maternal infections have also risen. Part of the reason for more women carrying pregnancies more successfully or longer when they are ill may be contributed to newer treatments for conditions such as diabetes, yet this does not explain entirely the increase in maternal morbidity. Increased cesarean births, longer labors with epidural anesthesia, pre-pregnancy obesity, rates of multifetal pregnancies, and the rising age of mothers are other factors to be considered.
Researchers studied trends in maternal morbidity and mortality in the United States in order to answer this question, and the answer is a definitive “yes”. Several studies describe increases in the rates of maternal morbidity, with issues such as cardiac and pulmonary complications, and the severe blood pressure fluctuations associated with eclampsia. Gestational diabetes, and postpartum rates for hemorrhage, perineal lacerations, and maternal infections have also risen. Part of the reason for more women carrying pregnancies more successfully or longer when they are ill may be contributed to newer treatments for conditions such as diabetes, yet this does not explain entirely the increase in maternal morbidity. Increased cesarean births, longer labors with epidural anesthesia, pre-pregnancy obesity, rates of multifetal pregnancies, and the rising age of mothers are other factors to be considered.
The more we know as health care providers about how maternal morbidity affects our rehabilitation efforts, the more we can contribute to a woman’s pregnancy and postpartum health. If you would like to learn more about caring for women during pregnancy and during the postpartum period, Herman & Wallace offers the Pregnancy and Postpartum Series. The following courses are available this year:
Care of the Pregnant Patient - Somerset, NJ
Apr 30, 2016 - May 1, 2016
Care of the Pregnant Patient - Akron, OH
Sep 10, 2016 - Sep 11, 2016
Peripartum Special Topics - Seattle, WA
Nov 12, 2016 - Nov 13, 2016
Tillett, J. (2015). Increasing Morbidity in the Pregnant Population in the United States. The Journal of perinatal & neonatal nursing, 29(3), 191-193.
As pelvic rehabilitation providers, it may be safe to assume a lot of us are treating adults with bladder and bowel dysfunction. Often we get questions from these patients about treatment for children with voiding dysfunction. How comfortable are we treating children for these problems and what would we do? Pediatric voiding dysfunction and bowel problems are common and can have significant consequences to quality of life for the child and the family, as well as negative health consequences to the lower urinary tract if left untreated. No clear gold standard of treatment for pediatric voiding dysfunction has been established and treatments range from behavioral therapy to medication and surgery.
 A randomized controlled trial in 2013 that was published in European Journal of Pediatrics, explores treatment options for pediatric voiding dysfunction. Pediatric voiding dysfunction is defined as involuntary and intermittent contraction or failure to relax the urethral striated sphincter during voluntary voiding. The dysfunctional voiding can present with variable symptoms including urinary urgency, urinary frequency, incontinence, urinary tract infections, and abnormal flow of urine from bladder back up the ureters (vesicoureteral reflux).
A randomized controlled trial in 2013 that was published in European Journal of Pediatrics, explores treatment options for pediatric voiding dysfunction. Pediatric voiding dysfunction is defined as involuntary and intermittent contraction or failure to relax the urethral striated sphincter during voluntary voiding. The dysfunctional voiding can present with variable symptoms including urinary urgency, urinary frequency, incontinence, urinary tract infections, and abnormal flow of urine from bladder back up the ureters (vesicoureteral reflux).
The 2013 study compared 60 children over one year who were diagnosed with dysfunctional voiding into two treatment groups. One group received behavioral urotherapy combined with PFM (pelvic floor muscle) exercises while the other group received just behavioral urotherapy. The behavioral urotherapy consisted of hydration, scheduled voiding, toilet training, and high fiber diet. Voiding pattern, EMG (electromyography) activity during voids, urinary urgency, daytime wetting, and PVR (post-void residue) were assessed at the beginning and end of the one year study with parents completing a voiding and bowel habit chart as well as uroflowmetry with pelvic floor muscle sEMG (surface electromyography) was administered to the child for voiding metrics.
All parents and children in both groups received education about urinary and gastrointestinal tract function as well as healthy bladder habits, effects of high fiber diet, scheduled voiding, and normal mechanics of toilet training. For the group that completed PFM exercises and education, they participated in 12 sessions (2x/week for 30 minutes) to learn the PFM exercises under the guidance of a single physical therapist. There was bimonthly follow up for both groups throughout the 12 months to ensure retention and application of the behavioral urotherapy.
The goal of the PFM exercises for the children was too restore the normal function of the PFM’s and their coordination with abdominal muscles. The exercises that the children completed, included exercises with and without a swiss ball. The exercises without a swiss ball included breathing with the diaphragm, Transversus Abdominus muscle isolation, hip adductor squeeze (isolation), bridging with PFM relaxation, and cat/camel to improve lumbopelvic coordination. Swiss ball exercises included seated PFM contraction and relaxation exercise with a seated lift and relax, supine bridge with roll out on the ball with PFM contraction, and supine swiss ball lift with the legs and pelvic contraction. (Pictures and more details about how the exercises were carried out in the article itself.)
The conclusion of the study was that the functional PFM exercises with swiss ball combined with behavioral urotherapy reduced the frequency of urinary incontinence, PVR (post void residue), and the severity of constipation in children with voiding dysfunction. The children in the combined group showed improvements with voiding pattern, reduced EMG activity during voids, reduced urgency, reduced daytime wetting, and improvements with more complete emptying with voids (reduced PVR).
The Functional PFM exercises are easy to teach and easy for children to complete. They are a safe, inexpensive, and effective treatment option for children with dysfunctional voiding. PFM exercises combined with behavioral urotherapy seems to be a logical treatment option for treating pediatric voiding dysfunction.
To learn more about pediatric bowel and bladder dysfunction and treatment for it consider attending Dawn Sandalcidi's Pediatric and Pelvic Floor Dysfunction course. The three opportunities in 2016 are Pediatric Incontinence - Augusta, GA April 16-18, Pediatric Incontinence - Torrance, CA June 11-12, and Pediatric Incontinence - Waterford, CT on September 17-18.
Seyedian, S. S. L., Sharifi-Rad, L., Ebadi, M., & Kajbafzadeh, A. M. (2014). Combined functional pelvic floor muscle exercises with Swiss ball and urotherapy for management of dysfunctional voiding in children: a randomized clinical trial. European Journal of Pediatrics, 173(10), 1347-1353.
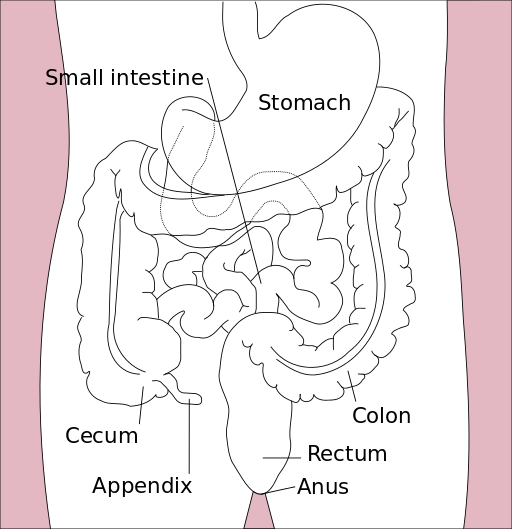
As a child, I remember my grandmother rubbing my lower back to help me pass my stubborn stool, a problem which landed me in the hospital twice before I turned 10. Decades later, after the birth of my first baby, I had a grade III perineal tear that made me afraid I would never be able to control my stool from passing. At the time of each situation, I had no idea how many people of all ages experience the two extremes of bowel dysfunction. Thankfully, for patients struggling with either issue, whether it is chronic constipation or fecal incontinence, healthcare practitioners are becoming knowledgeable in how to treat both effectively through classes such as the Herman & Wallace course, “Bowel Pathology, Function, Dysfunction & the Pelvic Floor.”
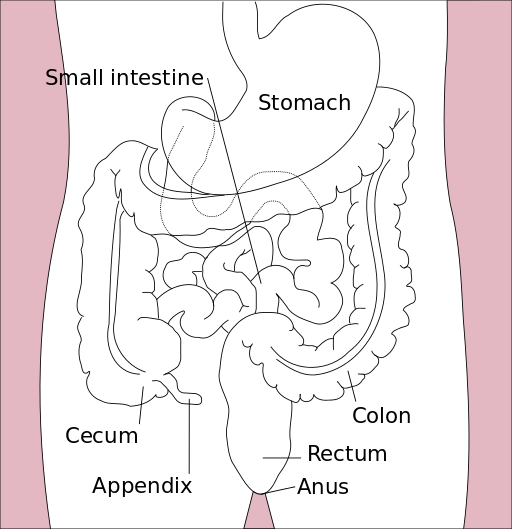 In 2014, Kelly Scott, MD, authored an article entitled, “Pelvic Floor Rehabilitation in the Treatment of Fecal Incontinence.” She reviews the current literature and notes this area of study lacks high quality randomized controlled trials, and further research is needed to provide evidence on the efficacy of different treatment protocols. Up to 24% of the adult population has been shown to experience fecal incontinence. Under the umbrella of pelvic floor rehabilitation lies pelvic floor muscle training, biofeedback, rectal balloon catheters for volumetric training, external electrical stimulation, and behavioral bowel retraining. The goals of various biofeedback methods include the following: provide endurance training specifically for the anal sphincter and pelvic floor; improve rectal sensitivity and compliance; and, increase coordination and sensory discrimination of the anal sphincter. Overall, the success rate of pelvic floor rehabilitation for fecal incontinence in most of the studies is 50% to 80%, and it is considered safe as well as effective.
In 2014, Kelly Scott, MD, authored an article entitled, “Pelvic Floor Rehabilitation in the Treatment of Fecal Incontinence.” She reviews the current literature and notes this area of study lacks high quality randomized controlled trials, and further research is needed to provide evidence on the efficacy of different treatment protocols. Up to 24% of the adult population has been shown to experience fecal incontinence. Under the umbrella of pelvic floor rehabilitation lies pelvic floor muscle training, biofeedback, rectal balloon catheters for volumetric training, external electrical stimulation, and behavioral bowel retraining. The goals of various biofeedback methods include the following: provide endurance training specifically for the anal sphincter and pelvic floor; improve rectal sensitivity and compliance; and, increase coordination and sensory discrimination of the anal sphincter. Overall, the success rate of pelvic floor rehabilitation for fecal incontinence in most of the studies is 50% to 80%, and it is considered safe as well as effective.
On the other end of the spectrum, Vazquez Roque and Bouras (2015) published an article regarding management of chronic constipation. Chronic constipation (CC) in the general population has a prevalence of 20%, and the elderly population has a higher rate than the younger population. Chronic constipation is commonly treated with stool softeners, fiber supplements, laxatives, and secretagogues. However, as in all areas of healthcare, a thorough examination needs to be performed to assess the source of the problem. Determining whether a patient exhibits slow transit constipation or a true pelvic floor dysfunction (PFD) via blood work, rectal exam, and appropriate PFD tests is essential to provide the appropriate treatment. When the CC culprit is dysfunction of the pelvic floor, clinical trials have proven the efficacy of pelvic floor rehabilitation and biofeedback, making them optimal treatments.
When research indicates a particular type of rehabilitation is effective for treating a wide scope of issues in an area of the body, learning how and when to implement the techniques is paramount for a well-rounded practitioner. Most of us do not dream of treating chronic constipation or fecal incontinence; but, as we mature in our clinical practice, the spectrum of dysfunctions we discover through diagnostic testing and experience grows. Continuing education in previously unexplored territories can only expand the population to whom we provide relief.
Scott, K. M. (2014). Pelvic Floor Rehabilitation in the Treatment of Fecal Incontinence. Clinics in Colon and Rectal Surgery, 27(3), 99–105.
Vazquez Roque, M., & Bouras, E. P. (2015). Epidemiology and management of chronic constipation in elderly patients. Clinical Interventions in Aging, 10, 919–930.
The following comes to us from Felicia Mohr, DPT, a guest contributor to the Pelvic Rehab Report.
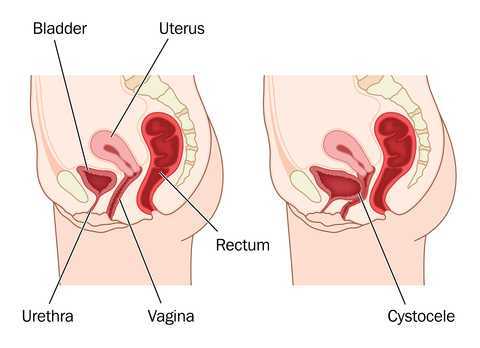
Vaginal mesh kits were used frequently early in the millennium as they led to high initial anatomic success rates with peak use between 2008 and 2010. Objectively they seemed to help elevate women’s pelvic organs to appropriate anatomical locations. Unfortunately there has been a high rate (10% according to a review of current literature on PubMedBarski 2015) of mesh erosion causing recurrent prolapse and/or stress urinary incontinence. Also there are cases when the mesh product perforates surrounding organs causing numerous dangerous complications. The rate of mesh-related complications according to current research is 15-25%. As a result, the FDA has reclassified the risk of synthetic mesh into a higher risk category so that the public has an increased awareness of the risk involved in these types of surgeries.
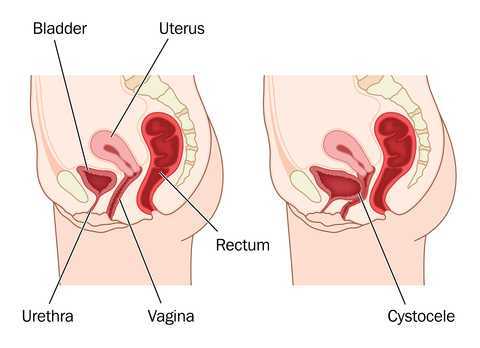 A systematic review and meta-analysis, published in 2015, reviewed the risk factors for mesh erosion following female pelvic floor reconstructive surgery (Deng, et al). They concluded the following factors increase risk of mesh erosion: younger age, more childbirths, premenopausal states, diabetes, smoking, concomitant hysterectomy, and surgery performed by a junior surgeon. Moreover, concomitant POP surgery and preservation of the uterus may be the potential protective factors for mesh erosion.
A systematic review and meta-analysis, published in 2015, reviewed the risk factors for mesh erosion following female pelvic floor reconstructive surgery (Deng, et al). They concluded the following factors increase risk of mesh erosion: younger age, more childbirths, premenopausal states, diabetes, smoking, concomitant hysterectomy, and surgery performed by a junior surgeon. Moreover, concomitant POP surgery and preservation of the uterus may be the potential protective factors for mesh erosion.
It is a common practice to perform a hysterectomy with a POP surgery. Reason being that the oversized uterus from childbearing adds extra weight on pelvic organs. However, the latter study as well as two other recent studies published in 2015 (Huang, Farthmann) also provide evidence that there is no benefit to a concomitant hysterectomy at the 2.5 year follow up and can lead to less satisfaction with surgery according to patient surveys respectively.
Keep in mind that all pelvic floor surgeries do not use the same amount of mesh material and different procedures have different risks associated with them. One retrospective study (Cohen, 2015) addressing incidence of mesh extrusion categorized 576 subjects into three categories: pubo-vaginal sling (PVS) (a small string of mesh around the urethra specifically addressing stress urinary incontinence only); PVS and anterior repair (also referred to as cystocele or bladder prolapse); and PVS with anterior and/or posterior repairs (also referred to as rectocele or rectal prolapse). Mesh extrusion for these types of procedures occurred at the follow rates: approximately 6% for PVS subjects, 15% for PVS + anterior repair, and 11% for PVS + anterior and/or posterior repair. This study did not account for any other types of mesh-related complications.
Pelvic organ prolapse and stress urinary incontinence make up some of the most common conditions for which patients seek Pelvic Floor physical therapy and perhaps this will allow us to better speak to current research on surgical options.
1. Barski D, Deng EY. Management of Mesh Complications after stress urinary incontinence and pelvic organ prolaps repair: review and analysis of the current literature. Biomed Research International; 2015Article ID 831285.
2. Deng T. et al. Risk factor for mesh erosion after female pelvic floor reconstructive surgery: a systematic review and meta-analysis. BJU International. Doi:10.1111/bju.13158.
3. Huang LY, et al. Medium-term comparison of uterus preservation versus hysterectomy in pelvic organ prolapse treatment with prolift mesh. International Urogynecology Journal. 2015;26(7):1013-20.
4. Farthmann J, et al. Functional outcome after pelvic floor reconstructive surgery with or without concomitant hysterectomy. Archives of Gynec and Obstet. 2015; 291(3):573-7.
5. Cohen S, Kaveler E. The incidence of mesh extrusion after vaginal incontinence and pelvic floor prolapse surgery. J of Hospital Admin. 2014; 3(4): www.sciedu.ca/jha.
After menopause, more than half of women may have vulvovaginal symptoms that can impact their lifestyle, emotional well-being and sexual health. What's more, the symptoms tend to co-exist with issues such as prolapse, urinary and/or bowel problems. But unfortunately many women aren't getting the help they need, despite a growing body of evidence that skilled pelvic rehab interventions are effective in the management of bladder/bowel dysfunctions, POP, sexual health issues and pelvic pain.
 Vaginal dryness, hot flashes, night sweats, disrupted sleep, and weight gain have been listed as the top five symptoms experienced by postmenopausal women in North America and Europe, according to a study by Minkin et al 2015, and they also concluded ‘The impact of postmenopausal symptoms on relationships is greater in women from countries where symptoms are more prevalent.’
Vaginal dryness, hot flashes, night sweats, disrupted sleep, and weight gain have been listed as the top five symptoms experienced by postmenopausal women in North America and Europe, according to a study by Minkin et al 2015, and they also concluded ‘The impact of postmenopausal symptoms on relationships is greater in women from countries where symptoms are more prevalent.’
Between 17% and 45% of postmenopausal women say they find sex painful, a condition referred to medically as dyspareunia. Vaginal thinning and dryness are the most common cause of dyspareunia in women over age 50. However pain during sex can also result from vulvodynia (chronic pain in the vulva, or external genitals) and a number of other causes not specifically associated with menopause or aging, particularly orthopaedic dysfunction, which the pelvic physical therapist is in an ideal position to screen for.
According to the North America Menopause Society, ‘…beyond the immediate effects of the pain itself, pain during sex (or simply fear or anticipation of pain during sex) can trigger performance anxiety or future arousal problems in some women. Worry over whether pain will come back can diminish lubrication or cause involuntary—and painful—tightening of the vaginal muscles, called vaginismus. The result can be a vicious circle, again highlighting how intertwined sexual problems can become.’
The research has demonstrated that the optimal strategy for post-menopausal stress incontinence is a combination of local hormonal treatment and pelvic floor muscle training – the strategy of combining the two approaches has been shown to be superior to either approach used individually (Castellani et al 2015, Capobianco et al 2012) and similar conclusions can be drawn for promoting sexual health peri- and post-menopausally.
The pelvic rehab specialist may be called upon to screen for orthopaedic dysfunction in the spine, hips or pelvis, to discuss sexual ergonomics such as positioning or the use of lubricant as well as providing information and education about sexual health before, during and after menopause.
To learn more about sexual health and pelvic floor function/dysfunction at menopause, join me in Atlanta in March for Menopause: A Rehab Approach!
Prevalence of postmenopausal symptoms in North America and Europe, Minkin, Mary Jane MD, NCMP1; Reiter, Suzanne RNC, NP, MM, MSN2; Maamari, Ricardo MD, NCMP3, Menopause:November 2015 - Volume 22 - Issue 11 - p 1231–1238
Low-Dose Intravaginal Estriol and Pelvic Floor Rehabilitation in Post-Menopausal Stress Urinary Incontinence, Castellani D. · Saldutto P. · Galica V. · Pace G. · Biferi D. · Paradiso Galatioto G. · Vicentini C., Urol Int 2015;95:417-421
Unfortunately one of the most common things we hear in pelvic rehab is “I hope you can help me, you’re my last hope.” In severe cases, this translates to the patient having little hope of surviving their life with pelvic pain. In severe but not necessarily life-threatening cases, being a patient’s last hope can also mean “please help me have sex in my relationship or my partner is going to leave me.” This situation places a lot of pressure on the patient and also on the therapist. How long did it take this patient to find her way to pelvic rehab? Research tells us that most women have been through multiple physicians, under- or misdiagnosed, and that many have failed attempts at intervention with medications or procedures.
 It’s clear to women that they are being judged when they go to medical appointments complaining of pelvic pain or pain with intercourse. Although it seems really old school to hear that a provider said “It’s all in your head.” or “How much do you like your partner?” or “Well, you’re getting older, sex isn’t that important.” these dismissive phrases are still used. A study by Nguyen et al., 2013 reported that women who reported chronic pain were more likely to perceive being stereotyped by doctors and others. Interestingly, among the group of women who had chronic vulvar pain, the women who sought care for their condition reported feeling more stigmatized. Because the support a woman perceives may influence her willingness to seek out help for chronic vulvar pain, we need to keep educating our peers, the public, and the providers about the real challenges women face, and the power of rehabilitation in overcoming those challenges.
It’s clear to women that they are being judged when they go to medical appointments complaining of pelvic pain or pain with intercourse. Although it seems really old school to hear that a provider said “It’s all in your head.” or “How much do you like your partner?” or “Well, you’re getting older, sex isn’t that important.” these dismissive phrases are still used. A study by Nguyen et al., 2013 reported that women who reported chronic pain were more likely to perceive being stereotyped by doctors and others. Interestingly, among the group of women who had chronic vulvar pain, the women who sought care for their condition reported feeling more stigmatized. Because the support a woman perceives may influence her willingness to seek out help for chronic vulvar pain, we need to keep educating our peers, the public, and the providers about the real challenges women face, and the power of rehabilitation in overcoming those challenges.
Vulvodynia is a common pelvic pain condition, and one that typically is associated with painful intercourse, or dyspareunia. (Arnold et al., 2006) It's estimated that by the age of 40, as many as 8% of women will have or have had a diagnosis of vulvodynia (Harlow et al., 2014), and this is clearly a significant quality of life issue.
Physical therapy has been shown to be successful in treating vulvar pain and pain with intercourse, including as part of a multidisciplinary approach. (Brotto et al., 2015) That's why Herman & Wallace is so eager to help empower more therapists to help patients live a life free of vulvar pain and dyspareunia. You can learn more about our courses and other resources at https://www.hermanwallace.com/continuing-education-courses.
Arnold, L. D., Bachmann, G. A., Kelly, S., Rosen, R., & Rhoads, G. G. (2006). Vulvodynia: characteristics and associations with co-morbidities and quality of life. Obstetrics and gynecology, 107(3), 617.
Brotto, L. A., Yong, P., Smith, K. B., & Sadownik, L. A. (2015). Impact of a multidisciplinary vulvodynia program on sexual functioning and dyspareunia. The journal of sexual medicine, 12(1), 238-247.
Harlow, B. L., Kunitz, C. G., Nguyen, R. H., Rydell, S. A., Turner, R. M., & MacLehose, R. F. (2014). Prevalence of symptoms consistent with a diagnosis of vulvodynia: population-based estimates from 2 geographic regions. American journal of obstetrics and gynecology, 210(1), 40-e1.
Nguyen, R. H., Turner, R. M., Rydell, S. A., MacLehose, R. F., & Harlow, B. L. (2013). Perceived stereotyping and seeking care for chronic vulvar pain. Pain Medicine, 14(10), 1461-1467.
Since the passing of Title IX in 1972, which protects people from sex discrimination in education or activity programs receiving federal funding, the number of females participating in sports has greatly increased. The National Federation of State High School Associations states that in 2011 nearly 3.2 million girls are participating in high school sports.
Unfortunately, a consequence of this increased participation in sports is a higher prevalence in urinary incontinence (UI) and stress urinary incontinence (SUI) in female athletes. Borin et al looked at the ability of nulliparous female athletes to generate intracavity perineal pressure in comparison to nonathletic women. The study demonstrated that higher mean pressures were generated by nonathletic women in comparison to the athletic women group and that lower perineal pressures in the athletic women were also related to number of games per year and time spent on sport specific workouts and strength training workouts.
UI and SUI are underreported in the general population and also in the athletic population. As health care professionals it is important to screen for UI and SUI in our clients. Physical therapy interventions using pelvic floor muscle rehabilitation have shown to decrease the severity of UI and SUI (Rivalta et al, Hulme). Rivalta used internal methods to improve the function of the pelvic floor muscle. Hulme’s success was achieved through activation of the pelvic floor muscles’ extrinsic synergists.
 |
 |
Pilates is often used in physical therapy as a therapeutic tool to improve lumbar stability with studies showing increases in abdominal strength (Sekendiz), trunk extensor endurance (Sekendiz) and to improve posture (Kloubec). Pilates is often also used in pelvic floor muscle rehabilitation and can easily be modified for low level clients. For example the use of resistance can assist supporting the weight of the leg. Practical proof, while lying supine in neutral lumbar spine position, stretch an arm and a leg away from center, notice the difficulty to maintain neutral spine. Now hold a resistance strap, which is also attached to the foot, and notice how maintaining neutral lumbar spine is easier to maintain (pictured above).
Pilates can also be modified for the higher level client or more athletic client. The use of arc barrels, BOSUs or the Hooked on Pilates MINIMAX (pictured belowy) allow the athletic client to achieve an inverted position, unloading the pelvic floor muscles. In the inverted position, pelvic floor muscles may be activated as intrinsic and/or extrinsic synergists of the pelvic floor muscles are also activated. These types of exercises may be more appealing to the athletic client ensuring continuation of the exercise post discharge from physical therapy.
 |
 |
Borin LC, Nunes FR, Guirro EC. Assessment of pelvic floor muscle pressure in female athletes. PMR. 2013; 5(3):189-193.
Hulme, Janet. Beyond Kegels 3rd edition, 2012 Phoenix Publishing Co. Missoula, Montana
Kloubec JA. Pilates for improvement of muscle endurance, flexibility, balance and posture. J Strength Cond Res. 2010;24:661-667.
Rivalta M, Sughunolfi MC, Micali S, De Stafani S, Torcasio F, Bianchi G, Urinary incontinence and sport. First and preliminary experience with a combined pelvic floor rehabilitation program in three female athletes. Health Care Women Int. 2010;31(5);330-334.
Sekendiz B, Altun O, Korkusuv F, Akin S, Effects of pilates exercise on trunk strength, endurance and flexibility in sedentary adult females. J Bodyw Mov Ther. 2005;9:52-57.
One of the dilemmas for many clinicians new to pelvic rehab is trying to figure out which equipment to purchase, and how to convince their employer (or themselves) to purchase the equipment. A common question in relation to equipment for pelvic rehabilitation is “what do I really need?” In a perfect world, and based on both existing and emerging research as well as clinical practice recommendations, we would all have access to pressure biofeedback and real-time ultrasound to help us document and train our patients in best strategies. The truth, however, lies in the fact that when those devices are not available, clinical practice can gain meaningful information from our best tools: our eyes and our hands. Certainly when completing research about pelvic floor generated pressures we might choose pressure biofeedback, and when looking for muscle activation patterns, needle EMG is the right choice, but no one should deny patients the opportunity to learn how to increase or decrease muscle activity, focus on movement retraining, and learn strategies to decrease improve quality of life and function because the latest technology is unavailable.
 Recent research published in the Brazilian Journal of Physical Therapy helps affirm the value of vaginal palpation in an article that assessed the relationship between vaginal palpation, vaginal squeeze pressure, electromyography and ultrasound. Eighty women between the ages of 18 and 35 years old, who had never given birth, and who had no known pelvic floor dysfunction were given a thorough evaluation using a multitude of evaluative methods. These methods included vaginal digital palpation (using Modified Oxford scale), vaginal squeeze pressure, electromyographic activity, diameter of the bulbocavernosus muscles as well as bladder neck movement using transperineal ultrasound. The muscles were assessed in a supine, hooklying position. A strong and positive correlation was found between pelvic floor muscle function and pelvic floor muscle contraction pressure. A less strong correlation was found between pelvic muscle function and pressure and electromyography and ultrasound.
Recent research published in the Brazilian Journal of Physical Therapy helps affirm the value of vaginal palpation in an article that assessed the relationship between vaginal palpation, vaginal squeeze pressure, electromyography and ultrasound. Eighty women between the ages of 18 and 35 years old, who had never given birth, and who had no known pelvic floor dysfunction were given a thorough evaluation using a multitude of evaluative methods. These methods included vaginal digital palpation (using Modified Oxford scale), vaginal squeeze pressure, electromyographic activity, diameter of the bulbocavernosus muscles as well as bladder neck movement using transperineal ultrasound. The muscles were assessed in a supine, hooklying position. A strong and positive correlation was found between pelvic floor muscle function and pelvic floor muscle contraction pressure. A less strong correlation was found between pelvic muscle function and pressure and electromyography and ultrasound.
Vaginal pelvic muscle assessment via palpation has been shown to be more accurate when assessed by more experienced therapists, and use of multiple methods may be most valuable in gaining the most accurate data. In addition to validating the usefulness of pelvic muscle palpation as an evaluative tool, the authors point out that transperineal ultrasound may also be the most appropriate tool for pediatric patients or patients who are otherwise not appropriate for internal pelvic muscle assessment.
Pereira, V. S., Hirakawa, H. S., Oliveira, A. B., & Driusso, P. (2014). Relationship among vaginal palpation, vaginal squeeze pressure, electromyographic and ultrasonographic variables of female pelvic floor muscles. Brazilian journal of physical therapy, 18(5), 428-434.
Rarely does a patient with sacroiliac joint dysfunction come to see us with a goal of having surgery. Sometimes surgery winds up being the last resort for relief if our efforts and the patient’s commitment to physical therapy and prescribed exercises fail. Some of the most recent research shows positive results from minimally invasive surgery; however, the bottom line is to make sure the most educated, clinically accurate diagnosis has been made in implicating the SI joint as the source of pain.
Capobianco et al (2015) performed a prospective multi-center trial regarding SI joint fusion using a minimally invasive technique in women with post-partum pain in the pelvic girdle. Eligibility for the study required subjects to have 3 out of 5 positive SI joint stress tests and at least 50% relief with image-guided intra-articular SI joint block with a local anesthetic. Of the 172 subjects in the study, 20 of the 100 females had post-partum pelvic girdle pain, and 52 subjects were male. Significant improvements in pain, quality of life, and function were found for not only the post-partum group but all groups 12 months after surgery. Worth noting is one to three weeks after surgery, the subjects engaged in physical therapy, two times per week for six weeks.
Whang et al (2015) assessed the 6-month outcomes of SI joint fusion using triangular titanium implants versus non-surgical management in a prospective randomized controlled trial. Of the 148 subjects chosen based on similar diagnostic criteria as the study mentioned above, 102 underwent surgery, and 46 had non-surgical management. Non-surgical management involved appropriate pain medication administration, physical therapy, intra-articular SI joint steroid injections, and radiofrequency ablation of sacral nerve roots, all based on individual needs. The surgical group subjects in this study were also asked to have physical therapy two times per week for six weeks anywhere from one to three weeks post-op. The results in a six month follow up showed “clinical success” of >80% in the surgical group and <25% in the non-surgical management group.
The Journal of Neurosurgery: Spine presented an article in July 2015 by Zaidi et al with results of a systematic review of literature regarding the surgical and clinical effectiveness of SI joint fusion. The studies included open as well as minimally invasive surgery, and the causes of surgery included SI joint degeneration and arthritis, SIJ dysfunction, postpartum instability, posttraumatic, idiopathic, pathological fractures, and HLA-B27+/rheumatoid arthritis. A mean rate of satisfaction with open surgery was 54%; whereas, the mean was 84% with minimally invasive surgery. Ultimately, the authors concluded, “serious consideration of the cause of pain” is necessary before embarking on SI joint fusion as the evidence for the surgery’s efficacy is lacking.
So, who is responsible for making the definite diagnosis for SI joint dysfunction? As many patients get minimal time in doctor offices, we have a professional responsibility to competently perform a thorough evaluation for our patients. When the diagnosis is “SI joint dysfunction,” rule out the lumbar spine and hip; and, of course, when “low back pain” or “hip pain” fills the diagnosis line, rule out/in the SI joint. If you are confused about how, it is time to consider taking the Sacroiliac Joint Evaluation and Treatment course!
References:
Capobianco, R., Cher, D., & for the SIFI Study Group. (2015). Safety and effectiveness of minimally invasive sacroiliac joint fusion in women with persistent post-partum posterior pelvic girdle pain: 12-month outcomes from a prospective, multi-center trial. SpringerPlus, 4, 570. http://doi.org/10.1186/s40064-015-1359-y
Zaidi, Hasan A., Montoure, Andrew J., and Dickman, Curits A. (2015). Surgical and clinical efficacy of sacroiliac joint fusion: a systematic review of the literature. Journal of Neurosurgery: Spine. (23)1:59-66. DOI: 10.3171/2014.10.SPINE14516
Whang, P., Cher, D., Polly, D., Frank, C., Lockstadt, H., Glaser, J., … Sembrano, J. (2015). Sacroiliac Joint Fusion Using Triangular Titanium Implants vs. Non-Surgical Management: Six-Month Outcomes from a Prospective Randomized Controlled Trial. International Journal of Spine Surgery, 9, 6. http://doi.org/10.14444/2006
Exercise in pregnancy is a loaded topic. We commonly see images of women doing vigorous exercise in late pregnancy accompanied by judgmental statements about the safety of such activity not only for the woman, but also for the baby. Many myths persist about exercise in pregnancy, and it’s our role as health care specialists to educate women about what is known about exercising. Holly Herman, co-founder of the Herman & Wallace Pelvic Rehabilitation Institute, has been educating providers about this topic for most of her career. Anyone lucky enough to take a course on pregnancy and postpartum issues from Holly Herman knows that her style of teaching is effective and her passion is contagious. From Holly’s use of patient stories to wonderful humor, you can really “get it” when it comes to clinical concepts and strategies. One of Holly’s clinical pearls that really stuck with me after learning about exercise and pregnancy is the research completed by James Clapp in his book “Exercise in Pregnancy”. In short, the book dispels the myth that women shouldn’t exercise in pregnancy and in fact reports on the benefits of exercise to both Mom and baby for labor, delivery, and beyond. In signature style, Holly held this book up in front of the class and to great laughter said, “And this is the book you should buy for your mother-in-law.”
 Another myth that has been perpetuated in relation to pregnancy, labor and delivery is the notion that exercising can make the pelvic floor muscles short, tight, and more narrow, making delivery more difficult. In an article we reported on previously about women being “too tight to give birth” the authors concluded that strong pelvic floor muscles do not lead to challenges with birthing. (Bo et al., 2013) In a more recent article that addressed this issue, Kari Bo and colleagues studied 274 women for levator hiatus (LH) width to see if exercising in late pregnancy did in fact narrow this space. At week 37 of gestation, the exercisers were measured to have a significantly larger LH than the non-exercisers. (Exercisers were defined as women who exercised 30 minutes or more 3 times per week versus the non-exercisers.) The authors conclude that there were not any significant differences in labor outcomes or in delivery outcomes between the groups. (Bo et al., 2015)
Another myth that has been perpetuated in relation to pregnancy, labor and delivery is the notion that exercising can make the pelvic floor muscles short, tight, and more narrow, making delivery more difficult. In an article we reported on previously about women being “too tight to give birth” the authors concluded that strong pelvic floor muscles do not lead to challenges with birthing. (Bo et al., 2013) In a more recent article that addressed this issue, Kari Bo and colleagues studied 274 women for levator hiatus (LH) width to see if exercising in late pregnancy did in fact narrow this space. At week 37 of gestation, the exercisers were measured to have a significantly larger LH than the non-exercisers. (Exercisers were defined as women who exercised 30 minutes or more 3 times per week versus the non-exercisers.) The authors conclude that there were not any significant differences in labor outcomes or in delivery outcomes between the groups. (Bo et al., 2015)
Without a doubt, the patient’s obstetrician gives primary direction to the patient when any high-risk issues are present. Most women however, are basing their exercise choices on experience, on misinformation, myths, or popular opinion. It is our responsibility to engage women in conversations about her health, wellness, and fitness, and to appropriately counsel on exercise during pregnancy and the postpartum period. Most of us lacked proper education about this important population in our primary graduate training, and therefore must seek out information to fill in the gaps. If you are interested in filling in any gaps, join us at one of our peripartum courses around the country. Your next opportunities to take these courses are:
Care of the Postpartum Patient - Seattle, WA
Mar 12, 2016 - Mar 13, 2016
Care of the Pregnant Patient - Somerset, NJ
Apr 30, 2016 - May 1, 2016
Care of the Pregnant Patient - Akron, OH
Sep 10, 2016 - Sep 11, 2016
Bø, K., Hilde, G., Jensen, J. S., Siafarikas, F., & Engh, M. E. (2013). Too tight to give birth? Assessment of pelvic floor muscle function in 277 nulliparous pregnant women. International urogynecology journal, 24(12), 2065-2070.
Bø, K., Hilde, G., Stær-Jensen, J., Siafarikas, F., Tennfjord, M. K., & Engh, M. E. (2015). Does general exercise training before and during pregnancy influence the pelvic floor “opening” and delivery outcome? A 3D/4D ultrasound study following nulliparous pregnant women from mid-pregnancy to childbirth. British journal of sports medicine, 49(3), 196-199.
Clapp, J. F., Cram, C. (2012) Exercising Through Your Pregnancy. Addicts Books