This post was written by H&W instructor Elizabeth Hampton. Elizabeth will be presenting her Finding the Driver course in Milwaukee in April!
One of the most consistent questions that we hear at the Pelvic Floor 2B course is, “How do you choose between a pelvic floor and a musculoskeletal exam during your first visit with a pelvic pain client?” The answer depends on a number of factors, which include your clinical reasoning, toolbox, the client’s presentation, the clinical specialty, and expectations of the referring provider as well as the expectations of the client. It can be stressful to imagine gathering a detailed history, testing, client education and a home program within the first visit! Now that we have less time and total visits to evaluate and treat these complex issues, it can be overwhelming to know where to start.
Chronic pelvic pain has multifactorial etiology, which may include urogynecologic, colorectal, gastrointestinal, sexual, neuropsychiatric, neurological and musculoskeletal disorders. (Biasi et al 2014) Herman and Wallace faculty member, Elizabeth Hampton PT, WCS, BCB-PMD has developed an evidence based systematic screen for pelvic pain that she presents in her course “Finding the Driver in Pelvic Pain”. “There are a number of extraordinary models that exist for treatment of pelvic pain including Diane Lee’s Integrated System of Function, Postural Restoration Institute, Institute of Physical Art and more,” states Hampton. “However, regardless of the treatment style and expertise of the clinician, each clinician should be able to perform fundamental tissue specific screening. If a client has L45 discogenic LBP with segmental hypermobility into extension, femoral acetabular impingement, urinary frequency > 12/day as well as constipation contributed to by puborectalis functional and structural shortness, all clinicians should be able to arrive at the same fundamental findings during their screening exam. The driver of the PFM overactivity(3) needs to be explored further as local treatment alone (biofeedback and downtraining) will not resolve until the condition causing the hypertonus is found and treated.” Finding the Driver in Pelvic Pain is a course that models a comprehensive intrapelvic and extrapelvic screening exam with evidence based validated testing to rule out red flags, understand key factors in the client’s case as well as develop clinical reasoning for prioritizing treatment and plan of care. The screening exam complements any treatment model as it identifies tissue specific pain generators and structural condition, which will lead the clinician to follow their clinical reasoning and treatment model. Once the fundamentals are established, the clinician can move beyond screening and drill down into treatment of key factors which may include specific muscle gripping patterns, arthokinematic assessment and respiratory evaluation and retraining, among others.
Co-morbidities are common in pelvic pain are well documented (1, 2) and clinically these multiple factors are the reason pelvic pain is complex to evaluate and treat. Intrapelvic (urogynecologic, colorectal, sexual) as well as extrapelvic (orthopedic, neurologic, psychological and biomechanical clinical expertise) are required for skilled evaluation and treatment of this population. It is precisely this complexity, which makes working with pelvic pain clients challenging and extraordinarily rewarding. Physical therapists are uniquely skilled to put all of the puzzle pieces together in these complex clients. Finding the Driver is being offered twice in 2015: April 23-25, 2015 at Marquette University and again in the fall. Check Herman Wallace.com for further details.
1. Chronic pelvic pain: comorbidity between chronic musculoskeletal pain and vulvodynia. Reumatismo: 2014 6;66(1):87-91. Epub 2014 Jun 6. G Biasi, V Di Sabatino, A Ghizzani, M Galeazzi
2. http://www.jhasim.net/files/articlefiles/pdf/XASIM_Master_5_6_p306_315.pdf
3. IUGA/ICS Terminology for Female Pelvic Floor Dysfunction. http://c.ymcdn.com/sites/www.iuga.org/resource/resmgr/iuga_documents/iugaics_termdysfunction.pdf
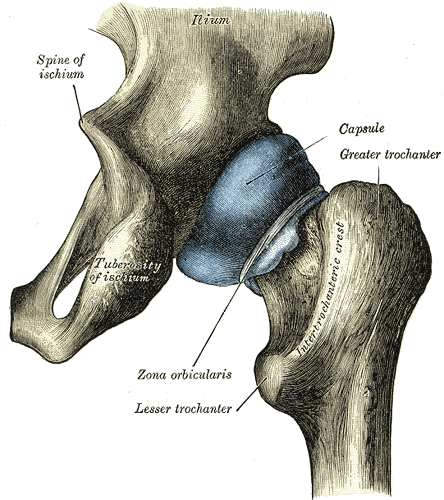
An article appearing this year in Arthroscopy details a systematic review completed to determine if asymptomatic individuals show evidence on imaging of femoroacetabular impingement, or FAI. Cam, pincer, and combined lesions were included in the results. To read some basics about femoroacetabular injury, click here. Over 2100 hips (57% men, 43% women) with a mean age of 25 were studied. (Only seven of the 26 studies reported on labral tears.) The researchers found the following prevalence in this asymptomatic population:
Cam lesion: 37% (55% in athletes versus 23% in general population)
Pincer lesion: 67%
Labral tears: 68%
Mean lateral and anterior center edge angles: 30-31 degrees
The authors conclude that femoroacetabular impingement tissue changes and hip labral injury are common findings in asymptomatic patients, therefore, clinicians must determine the relevance of the findings in relation to patient history and physical examination. Because hip pain is a common comorbidity of pelvic pain, knowing how to screen the hip joint for FAI or labral tears, rehabilitate hips with joint dysfunction, and help someone return to activity following a hip repair is valuable to the pelvic rehabilitation therapist.
As the athletic population may have increased risk of hip injuries due to overuse, traumatic injury, or vigorous activity, being able to address dysfunction in both high level and less active patients is necessary. Herman & Wallace faculty member Steve Dischiavi has developed a course rich in athletic examples and including education about activating fascial systems in various planes. If you are ready to step up your game related to Biomechanical Assessment of the Hip & Pelvis, check out this continuing education course taking place next in Durham, North Carolina in May.
In our weekly feature section, Pelvic Rehab Report is proud to present this interview with newly certified practitioner Reeba Varghese, DPT. PRPC.

How did you get involved in the pelvic rehabilitation field?
I was asked to attend a course by my director back in 2008 because they wanted to expand pelvic rehabilitation services to a few of our company's locations. I told my director I did not think this specialty was for me but I would be willing to attend one course and see how I felt. When I attended PF1 I was immediately drawn in by the wealth of knowledge I gained. Learning the intricacies of the human anatomy, specifically the female anatomy just completely opened my eyes to one of Gods most amazing creations. Also, the passion in the instructors was contagious. When I returned to work and started to see patients with incontinence and listened to their stories my passion for supporting these individuals in their rehabilitation journey began to grow. As I continued to expand my knowledge base by attending more courses through Herman and Wallace I realized I had found my niche in the world of physical therapy.
What patient population do you find most rewarding in treating and why?
I feel honored every time a patient walks into my clinic and begins to open up and share about their pelvic health issues. There is so much stigma associated with discussing these issues so when someone is willing to receive help I want to support them however I can. Also, it seems like more and more women I see have been through some kind of traumatic experience in their life and they find their way to you in an emotionally unstable state. What a great opportunity to be a part of their healing journey.
What motivated you to earn PRPC?
After practicing as a physical therapist for 10 years I was re-evaluating my life as a whole and was praying about what direction to go next in my life/career. I felt like the next step for me was to pursue a specialty area that I wanted to invest more time and energy into, as well as seek opportunities for professional growth. Shortly after I made this decision I received an email from Herman and Wallace regarding the fall 2014 PRPC exam. The lightbulb went off and I decided to apply to sit for the exam.
What is in store for you in the future?
One of my biggest dreams is to be a mother one day. I will be getting married this fall and hopefully starting a family. I plan to work part-time once kids come along. I am considering maybe working in a clinic which solely provides pelvic rehabilitation services. I also have a passion for taking my skills and knowledge and serving women in areas that do not have healthcare. I have done medical mission trips to Oaxaca, Mexico and served in an orphanage in Brasov, Romania. I absolutely plan to continue doing medical missions. I think it would be an honor to serve the women and children in the red light districts of India.
Learn more about Reeba Varghese, DPT. PRPC at her Certified Pelvic Rehabilitation Practitioner bio page. You can also learn more about the Pelvic Rehabilitation Practitioner Certification at www.hermanwallace.com/certification.

The merriam-webster online dictionary defines reflex as "an action or movement of the body that happens automatically as a reaction to something" or as "something that you do without thinking as a reaction to something." This reflexive action ideally describes what the pelvic floor does when we perform an activity that increases intra-abdominal pressure- and that can help us tighten the pelvic floor protectively so that urine is not expelled from the bladder and out the urethra. A research article by Dietz, Bond, & Shek asked if childbirth interrupted the body's natural reflex of contracting the pelvic floor muscles during a cough.
84 women completed the study, which utilized ultrasound measurements to assess reflex contraction of the pelvic floor during a cough. The women were pregnant with their first child (a singleton) and were between 33-37 weeks gestation. Prior to childbirth, 98% of the subjects demonstrated a reflex contraction of the pelvic floor muscles. At a postpartum visit at least 3 months postpartum, the number of women completing a reflex contraction was reduced to 75%. In addition to fewer women demonstrating a shortening contraction during a cough in the postpartum women, the intensity of the contraction was also reduced.
To collect the data, the researchers prospectively completed 4D (4-dimensional) ultrasound (US) volume measurement of the pelvic floor during a cough. They used levator hiatus diameter changes to quantify reflex action of the pelvic floor muscles. From prenatal to postnatal visit, the magnitude of the reflex contraction decreased from 4.8 mm to 2.0 mm (the number represents the mean difference in midsaggital diameter between rest and maximal contraction.) In the antenatal visit, 26 of the 84 women complained of stress urinary incontinence, at the postpartum visit, 20 reported stress incontinence. An association was noted between a lower magnitude of reflex contraction and stress urinary incontinence.
The authors conclude that pelvic floor reflexes are altered by childbirth. The study offers theories as to why the reflexive contraction is interrupted, such as nerve injury or muscle damage, but did not make concrete conclusions about the causes of reflex interruption. Regardless of the mechanism that interrupts a reflexive contraction, this study highlights the value and importance of teaching women to retrain this importance reflexive contraction, and not only for a cough, but for any activity that may create a significant change in intra-abdominal pressure. If you are interested in learning more about postpartum rehabilitation, check out the Care of the Postpartum Patient, which will be offered next in Boston in May!
In our weekly feature section, Pelvic Rehab Report is proud to present this interview with Herman & Wallace instructor Tina Allen, PT, BCB-PMD, PRPC

How did you get started in pelvic rehab?
I was about 5 years into my career as a PT when for some reason I had patients who where comfortable with me enough to ask questions like, "I'm leaking. Is that normal after giving birth?", "Since my total hip replacement I've been leaking urine" and "I have pain sometimes when I'm have sex...is that normal?". I was working in Outpatient Orthopaedics and I had no idea if it was normal. I searched and found out that it wasn't. After whispering to my patients that it wasn't normal, that I read that there where things they could do about it and then slipping them pieces of paper with instructions on how to maybe make it better; I decided I should learn if there was something a PT could do to help. I spent time with Ob/Gyn's and Urologists learning from them and applying my musculoskelatal knowledge to what they taught me. I was still in denial that I could help folks but then I started getting patients specifically referred to me for these conditions. I finally found that there where classes I could take! Imagine! That was 20 years ago now!
Who or what inspired you?
My patients have always been who inspires me! The questions they ask and how they face what they are going through has always pushed me to figure out ways to help them along their paths to healing and improved function!
I must also include all the PT's whom take our courses. Watching everyone lean into the uncomfortableness of what we teach and the questions everyone asks all in the hopes of helping that client whom walks into the clinic on Monday is inspiring.
What have you found most rewarding in treating this patient population?
It has to be that first session with a patient whom when you educate them on anatomy and function of the urogynecolgical system including fascia and what is needed for function (intimacy, continence etc) and I can see the light bulb go off for them on how everything is connected and everything has to be treated as a whole.
What do you find more rewarding about teaching?
This has to be the inspiration I get a thrill from being with a room of Pelvic Rehab therapists. We all work behind closed doors all day and getting to be in a room with such amazing like-minded therapists gives me a shot in the arm. To watch us all click in and problem solve how to serve our population of clients is inspiring for me.
How did you get started teaching pelvic rehab?
I was lab assisting courses for Kathe and Holly for years. Then one year Holly Herman just kept saying to me, "Why aren't you teaching?" "You could teach this?" "Tina, why don't you take this lecture?" "Tina, how many patients do you see like this in a day? What would you do?" I almost starting avoiding her Then I talked to Kathe about teaching and she said she was just waiting for me to say I was ready to start. That's our founders; always encouraging us to do more and contribute more!
What was it like the first time you taught a course to a group of therapists?
The first time I taught was terrifying! I'm a bonafide introvert (have multiple personalty tests to prove it) and standing in front of 40+ folks talking was not my idea of a fun way to spend a weekend. After the first lecture or two I found a rhythm and relaxed into it. By the afternoon or maybe the next day I was very excited to be around so many clinicians interested in learning and treating Pelvic Rehab.
What have you learned over the years that has been most valuable to you?
That my clients journey is their journey and I get to be a part of it. It's a privilege but it is still their journey. My hope is that where ever they meet me along their path I can assist them to their next step. As long as I get out the way that can happen.
What is your favorite topic about which you teach?
My favorite part of every course are the lab sessions. Getting to teach at each table in small groups and helping clinicians refine their observation and palpation skills is what makes me happy!

A US study published in the International Society for Sexual Medicine last year reports on the available evidence linking cycling to female sexual dysfunction. In the article, some of the study results are summarized in the left column of the chart below. On the right side of the column, we can consider ideas about how to potentially address these issues.
| Examples of Research Cited |
Ideas for Addressing Potential for Harm |
| dropped handlebar position increases pressure on the perineum and can decrease genital sensation | encourage cyclists to take breaks from dropped position, either by standing up or by moving out of drops temporarily |
| chronic trauma can cause clitoral injury | encourage cyclists to wear appropriately padded clothing, to apply cooling to decrease inflammation, and to use quality shocks or move out of the saddle when going over rough roads/terrain when able |
| saddle loading differs between men and women | women should consider specific fit for bike saddles |
| women have greater anterior pelvic tilt motion | is pelvic motion on bike demonstrating adequate stability of pelvis or is there a lot of extra motion and rocking occurring? |
| lymphatics can be harmed from frequent infections and from groin compression | patients should be instructed in positions of relief from compression and in self-lymphatic drainage |
| pressure in the perineal area is affected by saddle design, shape | female cyclists with concerns about perineal health should work with a therapist or bike expert who is knowledgeable about a variety of products and fit issues |
| unilateral vulvar enlargement can occur from biomechanics factors | therapists should evaluate vulvar area for size, swelling, and evidence of imbalances in the tissues from side to side, and evaluate bike fit and mechanics, encouraging women to create more symmetry of limb use |
| genital sensation is frequently affected in cyclists, indicating dysfunction in pudendal nerve | therapists should evaluate female cyclists for sensory or motor loss, establishing a baseline for re-evaluation |
Because women tend to be more comfortable in an upright position, the authors recommend that a recreational (more upright) versus a competitive (more aerodynamic and forward leaning) position may be helpful for women when appropriate. Although saddles with nose cut-outs and other adaptations such as gel padding in seats are discussed in the article, the authors caution against making any distinct recommendations due to the paucity of literature that is available. The paper concludes that more research is needed, and particularly for considering the varied populations of riders ranging from recreational to racing.
Within a pelvic rehabilitation setting, applying all orthopedic and specific pelvic rehabilitation skills is necessary for women cyclists who present with pelvic dysfunction. Because injury to the perineal area including the pudendal nerve can have negative impact on function such as bowel, bladder, or sexual health, skills in helping a patient heal from compressive or traumatic cycling injuries is very valuable. To learn more about pudendal nerve health and dysfunction, the Institute offers a 2-day course titled Pudendal Neuralgia Assessment, Treatment and Differentials: A Brain/Pain Approach. This course is offered next in Salt Lake City in April, so sign up soon!

A US study published in the International Society for Sexual Medicine last year reports on the available evidence linking cycling to female sexual dysfunction. In the article, some of the study results are summarized in the left column of the chart below. On the right side of the column, we can consider ideas about how to potentially address these issues.
| Examples of Research Cited
|
Ideas for Addressing Potential for Harm |
| dropped handlebar position increases pressure on the perineum and can decrease genital sensation | encourage cyclists to take breaks from dropped position, either by standing up or by moving out of drops temporarily |
| chronic trauma can cause clitoral injury | encourage cyclists to wear appropriately padded clothing, to apply cooling to decrease inflammation, and to use quality shocks or move out of the saddle when going over rough roads/terrain when able |
| saddle loading differs between men and women | women should consider specific fit for bike saddles |
| women have greater anterior pelvic tilt motion | is pelvic motion on bike demonstrating adequate stability of pelvis or is there a lot of extra motion and rocking occurring? |
| lymphatics can be harmed from frequent infections and from groin compression | patients should be instructed in positions of relief from compression and in self-lymphatic drainage |
| pressure in the perineal area is affected by saddle design, shape | female cyclists with concerns about perineal health should work with a therapist or bike expert who is knowledgeable about a variety of products and fit issues |
| unilateral vulvar enlargement can occur from biomechanics factors | therapists should evaluate vulvar area for size, swelling, and evidence of imbalances in the tissues from side to side, and evaluate bike fit and mechanics, encouraging women to create more symmetry of limb use |
| genital sensation is frequently affected in cyclists, indicating dysfunction in pudendal nerve | therapists should evaluate female cyclists for sensory or motor loss, establishing a baseline for re-evaluation |
Because women tend to be more comfortable in an upright position, the authors recommend that a recreational (more upright) versus a competitive (more aerodynamic and forward leaning) position may be helpful for women when appropriate. Although saddles with nose cut-outs and other adaptations such as gel padding in seats are discussed in the article, the authors caution against making any distinct recommendations due to the paucity of literature that is available. The paper concludes that more research is needed, and particularly for considering the varied populations of riders ranging from recreational to racing.
Within a pelvic rehabilitation setting, applying all orthopedic and specific pelvic rehabilitation skills is necessary for women cyclists who present with pelvic dysfunction. Because injury to the perineal area including the pudendal nerve can have negative impact on function such as bowel, bladder, or sexual health, skills in helping a patient heal from compressive or traumatic cycling injuries is very valuable. To learn more about pudendal nerve health and dysfunction, the Institute offers a 2-day course titled Pudendal Neuralgia Assessment, Treatment and Differentials: A Brain/Pain Approach. This course is offered next in Salt Lake City in April, so sign up soon!
This post was written by H&W instructor Ginger Garner. Ginger will be presenting her Hip Labrum Injuries course in Houston in March!

Lots of you have reached out with questions about “best care” practices after hip surgery. There isn’t a whole lot in scientific literature written about rehab, and over many months of fielding questions on my closed HIP LABRAL PHYSIOTHERAPY FB page, I am finally ready to share what Best Care Practices after Hip Labral Surgery may look like.
Today is Post 1 of this series, which will follow me day-by-day, week-by-week, through the highs and lows of my recovery and rehabilitation. Here we go!
First, “What IS Hip Labral Surgery?”
A relatively new term, the surgery is presently called “Hip Preservation.” However I like to call a spade a spade – this surgery is a bona fide hip reconstruction.
This surgery is a major undertaking for surgeon and patient and is constantly charting new territory in surgical techniques and discoveries. A brilliant way to preserve the hip joint, a surgeon is charged with essentially piecing the hip back together and reshaping it to work better than before surgery. It comes with risks AND benefits, many of which I will address in posts to come. It requires serious dedication and a wicked good physical therapist to get you back to fighting shape after surgery. But success begins with choosing a good surgeon who is a specialist in this type of surgery (more on that later).
Not a hip replacement, hip labral surgery rarely ONLY consists of repair of the labrum. Most of the time, a torn hip labrum is an issue secondary to a whole slew of hip disorders that make up a quagmire of highly technical and complex systems that converge during hip reconstruction. Whew, that was a mouthful.
A few of those technical things include hip dysplasia, impingement syndromes (and oh are there lots of different kinds we will be discussing), tendinosis, bursitis, pelvic pain, sexual dysfunction, snapping hip phenomenon (internal and external), anteversion, retroversion, and well, that’s enough to get us started.
Passion for Hip Labral Rehab
Let me tell you that this surgery was everything I thought it was going to be, and a hell (there’s just no other way to put it) of a lot more. I would have LOVED to avoid surgery, and heck, to avoid the injury that led to surgery – because I don’t know a single person who would prefer to gain clinical expertise by actually suffering through the injury or surgery. But alas, adversity is often what makes us better.
As you may guess, I did experience a single traumatic injury – which then proceeded to give birth to a perpetually poorly behaved, havoc-wreaking monster of a chronic condition. The funny thing was before the injury, my area of clinical expertise was ALREADY orthopaedics and women’s health. You can see I was kind of in for a colossal butt-kicking lesson from the universe. Oh the irony…
I did try to prepare myself for the road to recovery though. Read my post on Shutting Down to Move Forward: The Therapist Becomes the Patient.
But trust me, I would rather NOT have gleaned clinical expertise on hip labral and pelvic injury through personal tragedy.
Nonetheless, I knew that my journey from hip reconstructive surgery back to health, was going to help more than just me. I could use it to help so many others who wrestle with that same monster.
But yea, there are a few challenges to recovery:
- I am mother. Of three boys. Ranging in age from 3-9.
- I was/still am trying to finish my doctorate.
- I completed a book chapter for a colleague’s new text on Fostering Creativity in Rehabilitation and a research manuscript during early post-op.
- I had to maintain a full teaching schedule that required walking and stair climbing (which I couldn’t do) and lots of standing (which I also could not do).
- The final straw was, midway through rehab, my oldest son received a special needs diagnosis.
Nevermind having clean laundry and healthy meals to foster healing (and maintain sanity). I mean, a human can only do so much. The point is – I didn’t live tweet or post about my recovery in real time.
The Bright Side
The good side though – is my delay in posting has given me much needed time to reflect on what variables are most critical to the recovery process.
If you are considering hip labral surgery, please read Top Five Must Have Hip Labral Surgery Tips to help you prepare.
Other colleagues I know have released blog series in real time, a chronicle to their injury and recovery. Shelly Prosko and her traumatic Achilles Tendon rupture, is one of those colleagues. Also a physioyogi, I highly recommend Shelly’s series on her recovery. Read here or cut and paste: http://www.gingergarner.com/2014/10/28/medical-therapeutic-yoga-achilles-tendon-rupture-missing-link-rehabilitation/
Now onward and forward, I am (finally) sitting down to write, 5 and a half months AFTER my surgery.
I hope you’ll join me on my journey through Hip Preservation, er, Reconstruction Surgery and that, most of all, you’ll find something that will inspire you to more complete healing and recovery.

An important survey completed in Australia asked if prenatal pelvic floor function and dysfunction relates to postnatal pelvic floor dysfunction (PFD). Interestingly, the authors propose that "…damage to the pelvic floor is probably made before first pregnancy due to congenital intrinsic weakness of pelvic floor structures." Many of the patients involved in the study had dysfunction in more than one domain of pelvic health, with the authors recommending a comprehensive approach to the evaluation of pelvic floor dysfunction.
As part of the large study called the Screening for Pregnancy Endpoints study, or SCOPE, a prospective cohort study called Prevalence and Predictors of Pelvic floor dysfunction in Prenips, or 4P, was also completed. The 4P research (n = 858) contained 2 different studies including a questionnaire-based survey and a detailed clinical assessment. The survey utilized the Australian pelvic floor questionnaire which was administered at 15 weeks gestation and at 1 year postpartum. The Australian questionnaire scores items on domains of urinary dysfunction, fecal dysfunction, pelvic organ prolapse, and sexual dysfunction. When the participants answered the questionnaire the first time, all answers were directed to be answered for symptoms they experienced prior to being pregnant.
The results indicated that at 1 year postpartum, 90% of the women in this study reported pelvic floor dysfunction. Regarding the domains of bladder, bowel, prolapse and sexual symptoms, 71% of the participants reported symptoms from more than 1 of these domains, 31% from 2 domains, 24% from 3 sections of the survey, and 8% from all four sections. Other interesting statistics are as follows:
-of the 73% of participants reporting urinary dysfunction, 67% had these symptoms persisting from the prenatal period
-pre-pregnancy urinary dysfunction symptoms persisted in postpartum in 61% of participants
-for new onset bowel symptoms in the postpartum period, fecal incontinence or obstructed defecation were more likely to occur, while incontinence of gas (flatus) was more likely to occur as persisting symptoms
-prolapse symptoms were reported by 14% of women, with 20% of participants describing symptoms as severe and most common symptoms being vaginal pressure, heaviness, or a sensation of a lump being present
-symptoms of sexual dysfunction such as dyspareunia persisted postnatally in 59% and worsened in 12% compared to prenatal period
In women who delivered vaginally, the risk of pelvic floor dysfunction was increased, yet the authors caution against stating that c-sections are protective against pelvic floor dysfunction. They do theorize based on survey results that c-section may reduce the persisting PFD. Ideally, research such as this can help can assist in creating predictions for postpartum pelvic floor symptoms based on prenatal symptom history. Certainly it may be helpful to be aware of a patient's prenatal symptoms and include any new onset or persisting postpartum symptoms in her rehabilitation. If you are interested in learning more about pelvic floor dysfunction in pregnancy or postpartum, these topics are included in our Pregnancy and Postpartum course series that you can find on our main course page. The Care of the Pregnant Patient is happening in mid-March in Seattle, with a few seats still available! Care of the Postpartum Patient happens next in May in Boston. If you are interested in hosting Peripartum Special Topics, send us an email or give us a call!
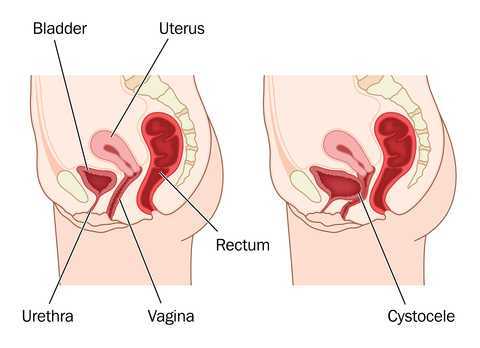
When considering rehabilitation of prolapse symptoms, therapists often implement an approach that addresses multiple factors related to pelvic health and function. Rehabilitation of prolapse symptoms may include bladder re-training, pelvic muscle strengthening, bowel health management, trunk and pelvic control strategies, avoidance of potential aggravating maneuvers such as bearing down, and education in management tools such as pessaries. As we have established in earlier posts in this 3-part series, each patient must be evaluated and treated with respect to her complaints and clinical findings. This post highlights a few of the many clinical research studies aimed at determining effectiveness of pelvic rehabilitation for prolapse symptoms.
In recent research, Hagen and colleagues completed a multi-center, randomized trial using parallel treatment groups to assess recovery from prolapse. Women with a stage I-III prolapse of any type confirmed by a physician using the POP-Q system and complaints of prolapse symptoms were the primary inclusion criteria. Women who had previously been treated by surgery for prolapse were excluded. The control group (n = 222) were given a prolapse lifestyle advice leaflet and no pelvic floor muscle training. The lifestyle advice included information about weight loss, constipation, avoidance of heavy lifting, coughing, and high-impact exercise. No information about pelvic floor muscle exercise was included.
The physiotherapy treatment group (n = 2250 received up to 5 individualized sessions of pelvic floor muscle training over 16 weeks. The first appointments were scheduled closer together to allow for proper training in muscle education, with the latter appointments being spread further apart. Rehabilitation began with instruction in pelvic muscle anatomy and function. Exercises were instructed based on results of a pelvic muscle assessment, and exercises were progressed with a goal of up to 10, 10-second holds, and up to 50 quick contractions completed three times per day. Women were also instructed in a pre-contraction of the pelvic floor muscles prior to increases in intra-abdominal pressure. (Electromyography, electrical stimulation, or pressure biofeedback were not allowed among the interventions.)
Outcomes tools included the pelvic organ prolapse symptom score (POP-SS) and several other tools to measure quality of life, level of bother from bowel and bladder symptoms, and a general health survey. Women in the physiotherapy treatment group reported more improvements in prolapse symptoms (POPP-SS). While degree of prolapse was also improved in the intervention group, the authors state that the differences were not significant when compared to the control group. Following are highlights from other research completed in prior years.
In this review of 5 randomized, controlled trials, Kari Bo describes the potential benefits demonstrated in the literature including improved pelvic organ prolapse (POP) stage, symptoms, and pelvic floor muscle morphology. The author summarizes that supervised and more intensive training is more effective than unsupervised training.
In this study the authors conducted 14 weeks of treatment with 7 clinic visits that included pelvic muscle awareness and proprioceptive training, education in home exercise program of strengthening.) Positive outcomes included improved anatomic measurements via POP-Q in anterior and posterior vaginal wall, and decreased prolapse symptoms. The intervention group demonstrated improved muscle strength, endurance, and surface EMG parameters. The study concluded that pelvic floor muscle training is effective in treating prolapse.
Compared with women in the control group, women in the pelvic floor muscle training group in this study demonstrated increased muscle thickness, decreased hiatal area, shortened muscle length, and elevated position of the bladder and rectum. Subjects also demonstrated decreased muscle length at maximum Valsalva, which the researchers indicated as a sign of increased muscle stiffness.
Following a 16 week physiotherapy program, women with stage I or II prolapse demonstrated significant improvement in stage of prolapse in this research. Women in the treatment group were more likely to report subjective improvement when compared to the control group.
The research indicates, although not consistently, that pelvic floor muscle training can improve the level of prolapse or descent in women with various types of prolapse. Many of the studies include not only pelvic muscle strengthening, but pelvic muscle awareness, protection, and training in functional activation to reduce the impact of straining when it does occur. Regardless of improvement in structural measures, women participating in pelvic muscle training consistently report decreased symptoms such as sense of heaviness when standing. In rehabilitation we are always concerned about function, level of bother, and quality of life of our patients. The bottom line appears to be that symptoms rule the day. We can tap into this fact by taking careful histories, by using outcomes tools, and by teaching our patients that over time they may benefit from continued rehabilitation efforts based on their home program. As with any home program, patients may benefit from a reevaluation and modification of a home program.
Although the research addressing perioperative pelvic rehabilitation is emerging, therapy in combination with surgical approaches may also help prepare women for successful management of prolapse symptoms. Evaluation and treatment of prolapse is instructed in the Institute's pelvic floor series, both in the Level 1 and in the Level 2B course. If you are interested in any series courses, please remember to plan ahead, as these courses fill up several months ahead of time! You can find all of our continuing education courses on the website by clicking here.
By accepting you will be accessing a service provided by a third-party external to https://www.hermanwallace.com/









































