Today on the Pelvic Rehab Report, we hear from Dustienne Miller. Dustienne wrote and teaches the Yoga for Pelvic Pain course, which is available in Cleveland, OH on July 18-19, and in Boston, MA on September 12-13.
"It feels like my pelvic floor just sighed."
Grounding in Mountain Pose

As musculoskeletal professionals, we have a sharp eye for postural dysfunction. We explain to our patients that the ribcage is sheared posteriorly to the plumb line and how gravity magnifies forces at specific structures. Some physical therapists perform the Vertical Compression Test (VCT) to allow the patient to feel the difference between their typical habitual posture and a more optimally aligned posture. This works well to “sell” your patients on why their newly aligned posture allows for more efficient weight transfer through the base of support. In addition to the VCT, I utilize Tadasana, or Mountain Pose as an additional kinesthetic approach to postural retraining.
Last week in the clinic, I was teaching my client postural awareness using Tadasana. I asked her to close her eyes, or lower her gaze if she was not comfortable closing her eyes. Working from the ground up, we started bringing awareness to her base of support. She noted that she was standing with her weight mostly in her heels. When I encouraged her to bring her weight forward, hinging from the talocrural joint, she had an “aha moment.” She said, “It feels like my pelvic floor just sighed.” She was unaware that her habitual posture was to stand with her weight mostly posterior to plumb line, thus encouraging her posterior pelvic floor to remain in an overactive state. Once she balanced her body from the ground up, she felt a major release in her holding patterns.
At our follow-up session, the client remarked that her postural awareness increased dramatically. She was surprised at how often her pelvic floor was in a habitual pattern of over-firing. Additionally, she reported increased awareness while practicing standing yoga postures during class. She feels more in control of her body after experiencing embodied optimal alignment and has had success with carrying over postural awareness outside of the clinic setting. Self-awareness and empowerment are two major goals of my physical therapy practice, and using yoga to achieve these goals makes my clinical practice even more enjoyable.
For more info on the Vertical Compression Test, click here. For detailed instruction on Tadasana, click here.
Much has been made of the research indicating that a Caesarean section has a protective effect on the pelvic floor, with some women requesting a CS in order to avoid pelvic floor dysfunction (PFD). This practices raises concern about an elective approach to CS versus natural vaginal birth, as CS are by no means without risk to the mother, the fetus, and to the neuromusculoskeletal system. Recent research contributes to this discussion by assessing several variables including quality of life factors and pelvic dysfunction following either a CS or natural vaginal birth. Twenty one women who had given birth in the prior 36 months were recruited from daycare facilities. Subjects were categorized into normal vaginal delivery (NVD) or Caesarean section (CS). Subjects were only included if they gave birth to singletons, had not previously participated in pelvic rehabilitation, or if they did not had a history of pelvic surgery, neurologic issues or trauma that affected bowel and bladder function. Outcomes tools included the SF-36, and the Pelvic Floor Distress Inventory (PFDI). Within the PFDI, outcomes tools assessed urinary, colorectal, prolapse, and pelvic floor functional impact.

Nearly 70% of the women in the group studied were between the ages of 30 and 39, with ages ranging from 21-45. The number of subjects who had given birth vaginally was 16, by Caesarean section, 5. The authors report that approximately 75% of their subjects were Caucasian, had a household income of 70,000 or more, and nearly 80% had at least a four-year degree. The women in the CS group reported higher rates of urinary incontinence and pelvic pain (90% and 67%, respectively) when compared to the NVD group (50% and 23%). Women who gave birth via CS also had higher mean scores on the Urinary Distress Inventory, Colorectal-Anal Distress Inventory, and the Pelvic Organ Prolapse Distress Inventory. The authors also noted a correlation between pelvic organ prolapse and body mass index (BMI) greater than 25.
This research contributes to the literature about birth mode and pelvic dysfunction, and the study conflicts with other data that describes a protective effect of Caesarean birth mode on the pelvic floor. While avoiding vaginal delivery may indeed help reduce some injury to the pelvic floor, this study, even though the sample size was not large, reminds us that CS delivery can be associated with pelvic dysfunction and symptoms. This study was different from many prior reports in that the subjects were surveyed in the chronic rather than immediate postpartum period. If you are interested in learning more about postpartum rehabilitation, check out the Institute's offerings on this page: http://hermanwallace.com/postpartum.

Bowel dysfunction is a common condition with potential for devastating limitation in a person's quality of life. Constipation, one type of bowel dysfunction, is often associated with an ability to properly coordinate the pelvic floor muscles during an attempt to empty the bowels. Instead of the pelvic floor muscles lengthening to allow the anorectal angle to increase (reducing the "bend" in the distal part of the rectum) the pelvic floor muscles might contract and thereby restrict proper emptying of the bowels. When this "opposite" or "paroxysmal" contraction occurs, a patient may be diagnosed with paroxysmal pelvic muscle function, also called dyssynergic defecation because of the lack of coordination in the muscles.
A recent study demonstrated that biofeedback therapy can be an effective tool in improving pelvic floor function for patients who demonstrate dyssynergic defecation. Magnetic resonance defecography (MR defecography) was measured prior to and after intervention, with variables of anorectal angle and perineal descent among those studied. Standard therapy was administered to 11 patients diagnosed with dyssynergia, and 11 patients received biofeedback therapy. All patients met the Rome diagnostic criteria for functional constipation, and all patients had diagnostic testing with resultant evidence of dyssynergistic muscle patterns. In addition to the MR defecography as a pre- and post-test, patients completed assessments of symptoms, quality of life, and severity of depression.
Standard therapy consisted of instructions in bowel habits, daily exercise such as walking, diaphragmatic breathing, fiber and fluid intake, defecation techniques, and timed toileting (such as attempting bowel movement 30 minutes after eating). Therapy occurred over a period of 3 months with at least once per week phone supervision. The patients in the biofeedback group were instructed in concepts of dyssynergia and in contract-relax training. Rectal sensory training with a rectal balloon was utilized if the patient had poor sensory perception. Patients were trained how to increase intrabdominal pressure while relaxing the pelvic floor muscles. They were also instructed in pelvic floor muscle strengthening, relaxation, and coordination, and were asked to complete home exercises three times per day for 10 minutes. Clinic sessions occurred at twice per week for 12 visits, then once per week for 6 visits, or a total of 18 visits over 3 months.
The authors found that paradoxical contraction and perineal descent with attempt to defecate improved significantly in the treatment group. Constipation symptoms, and depression and several quality of life scales also improved in the treatment group. Interestingly, the sense of incomplete emptying improved in both the treatment and the standard care group. While the results of the intervention are very positive, it would be interesting to include abdominal wall massage, a common technique employed to improve bowel function with constipation. If the patients demonstrated a tight pelvic floor with dyscoordinated patterns of movement, perhaps manual therapy to release tension or any pain that was present may have also been appropriate. As this is the first study to demonstrate through MR defecography an improvement in dyssynergia following biofeedback therapy, the study is very valuable to pelvic rehabilitation therapists. If you are interested in learning more about bowel dysfunction, you can start with the Pelvic Floor 2A course, which instructs bowel dysfunction including dyssynergistic defecation. The pelvic floor series courses sell out quickly, and the next opportunity to take this course is in St. Louis in October. You can also still find seats in the 2A continuing education course in the December courses taking place in Boston and in La Jolla.

The following is a message from Nari Clemons, the instructor of Herman & Wallace's new Meditation for Patients and Providers course. You can join Nari at Touro College in New York this July 19-20 at Meditation for Patients and Practitioners - New York, NY!
What doesn’t meditation do? And why aren’t we meditating, already?
I’ve heard it said that if all the benefits of exercise could be placed in a pill, it would be the most powerful prescription. I’m thinking that the same could be said for meditation. We hear little snippets of it as we scroll through the news: meditation for heart disease, meditation for blood pressure, meditation for decreased anxiety. Well, here is yet another study:
Researchers used fMRI technology to examine the brain in 50 people who had been meditating for an average of 20 years and 50 non- meditators. Both groups had the same number of men and women, with ages ranging from 24 to 77. The participants’ brains were scanned, and while age did related to gray matter loss, it was better preserved in those who meditate. **
Americans are living longer, but rates of Alzheimers and Neurodegenerative disease rates are going up. Well, meditation is something you can do to keep on top of your cognitive game. So, why aren’t people meditating? When I ask patients this, I often hear, “I don’t know how” or “I tried it once and I didn’t like it”. I think there is a misconception that mediation should be valued if someone had an experience of bliss or if they are “good at it”.
In fact, meditation is like exercise; it is a benefit that grows as you use it more. It can be hard at first when the mind is not used to being calm or more still. It is not a one-time-use kind of fix. Like exercise, as you do it more, you see more benefits, and you come to like it more. Not everyone who is starting an exercise program will want to train for marathons or be a ballerina or try cross fit. Just as there are different personalities and starting points with exercise, the same can apply to meditation.
In the MPP Herman Wallace course, Meditation for Patients and Practitioners, we break down a lot of the mystery behind learning and teaching meditation. We use techniques of different lengths of time and different aims. We discuss how to pick which technique for which patient or even how to choose a technique for the same patient in a different situation. Going further, we discuss ways to use meditation as a health care provider, so you can share in the benefits of a practice and keep yourself refreshed about your practice. Participants in the course get lots of lab time to develop comfort level deciphering which technique to use and be comfortable teaching and using meditation in their own lives. We also provide a CD with many of the techniques that you will be able to use to refresh course material or to recommend to participants for use in their own homes.
As providers we know that “carrying our patients home” by thinking of them when we leave work or staying sad or anxious about something that happened that day at work is not actually helpful to our patients. Or we may realize we are tired or worn out from the stress of our jobs. Yet, we really don’t know what to do about it. In the MPP course, we discuss ways to keep your job in the space it belongs in your life. This can help practitioners to live a more balanced life, as well as being more present at work.

The Pelvic Rehab Report recently caught up with Katie Woolf, DPT, in order to hear a bit about her recent experience at H&W's Pudendal Neuralgia course in Salt Lake City. The Pudendal Neuralgia course was developed and is instructed by faculty members Loretta Robertson and Tracy Sher. Katie had this to say about her experience in the course:
I recently attended the Pudendal Neuralgia course in Salt Lake City, Ut. It was a fabulous experience! The instructors were Tracy and Lorretta. They are such darling ladies. They have a contagious passion and endless knowledge of pelvic rehabilitation. This was my second Herman and Wallace course and I have never been disappointed. The facilities for the course were perfect as well.
This course opened my eyes to pelvic pain, pudendal neuralgia (PN), pelvic dysfunction, and how to recognize and manage it. The instructors gave an evidence based practice review and personal testimony of PN and how they treat patients with PN. The instructors were knowledgeable about anatomy, treatment interventions, and surgical interventions for to PN. Most of all they made it a fun course.
The course was well organized and gave great examples of how to interact with your patients about their pain and recovery. The course allowed for us professionals to network and learn from each other. It was interactive and thorough. I felt like every detail of PN was covered.
I have often been intimidated to treat pelvic dysfunction but after this course I discovered it’s just like treating any other diagnosis, “just down stairs.” The course was taught at a level I understood and could apply. I feel empowered to take my knowledge and become a better physical therapist. Tracy and Loretta instilled confidence in me that I can treat patients with PN and pelvic pain. It’s only been a few days but, I have already changed the way I interact with patients because of this course (although I haven't seen a patient with PN yet). I would highly recommend any of the Herman and Wallace courses to anyone who would like to learn about pelvic rehabilitation. The Herman and Wallace educational materials and booklet are a great resources and very helpful to review time and time again. We need more professionals who can help with the pelvic recovery and I feel like I can start to be a resource in my community. I cannot wait for the next course!

In our weekly feature section, Pelvic Rehab Report is proud to present this interview with Herman & Wallace instructor Ginger Garner, PT, MPT, ATC.
How did you get started in pelvic rehab?
My entry point into pelvic rehab was a bit unorthodox and as a result, my colleagues at the time (back in the 90’s), considered my practice quite eccentric and frankly, a bit strange.
In fact, although I can see lots of humor in it now, I was actually pushed out of a practice because what I was doing was “too individualized” and patient specific. Of course, that “eccentric” entry point into pelvic rehab was integrative medicine, using a yoga-based biopsychosocial model of practice.
Who or what inspired you?
To answer that question I think you first have to be able to recognize and appreciate times when you have not been well supported or inspired, kind of like having to know adversity before you can recognize and value success.
Here’s my short story:
Early on in my education (in sports medicine, athletic training, physical therapy, yoga, and pilates) I realized that the biomedical model, although stellar at handling life-threatening emergencies, was not always so great at addressing chronic conditions and preventing disease processes and injury. So the answer to what inspires me – is the privilege of being able to be on the prevention end of injury and disease.
Back in the 90’s, I had a faculty instructor who encouraged me to keep pursuing my passion – in spite of the pushback I got from many directions, including within the department at the university. She found a way for me to pursue lateral work in the School of Public Health, which I felt was necessary in order for me to become a successful patient advocate. It was a great experience where I was able to work with the Governor’s Council on Physical Fitness and Health and conduct a pilot study. Her encouragement inspired me to keep following my dream, which is why I strongly believe in this quote by Mark Twain,
“Keep away from people who try to belittle your ambitions. Small people always do that, but the really great make you feel that you, too, can become great.”
Fast forward almost 20 years, and my most influential mentors, sources of my biggest inspiration, have been 1) Dr. Riane Eisler, holocaust survivor, attorney, social scientist, and founder of the not-for-profit organization, Caring Economics, which works to end violence against women and raise the status of caregiving; and 2) my three children. Experiencing pregnancy three times was an enormous gift, which allowed me the privilege giving birth not just to my three boys, but also to the framework for using yoga in prenatal, childbirth, and postpartum to prevent and manage injury and pain. The mothers I work with also inspire me. The work I do is for them and their future children.
What have you found most rewarding in treating this patient population?
There is go greater reward than empowering women, especially mothers and mother-to-be.
Women are too frequently disempowered by our current medical model. Their concerns are often marginalized and the care they get can be dehumanizing and humiliating, especially during maternal and childbirth care. I believe that above being a physical therapist, an athletic trainer, and an integrative clinician, I am first and foremost a patient advocate. Each woman I work with is a personal investment of my time, energy, and dedication. The reward of seeing a woman be able to pursue the compassionate birth she wants and deserves, to find relief from pelvic pain, and to know what questions to ask to get the best care from her health care providers, all because of the time I have spent with her – is worth more than gold.
What do you find more rewarding about teaching? (this could be one story or something you always find magical about the experience)
The two most rewarding aspects of teaching are 1) changing the course and paradigm of practice in rehab and medicine by fostering creativity and a shift toward person-centered, integrative practice, and 2) getting to be constantly immersed in research.
I love learning and am the perpetual student. I’m currently working toward my doctorate at UNC Chapel Hill, and love the interchange and partnership that is nurtured by being in education.
What trends/changes are you finding in the field of pelvic rehab?
The full circle return to seeing the person as whole, and not broken or as a part, is incredibly encouraging.
I am seeing this through the integrative courses that H&W is embracing, including my own courses in yoga, but also and perhaps more importantly, through the ground swell of individual health care consumer action. Folks realize “health care” doesn’t just consist of drugs and surgery, and they are seeking out integrated care now more than ever. Still yet, access to pelvic rehab can be vastly improved, which is a great segue into the next question.
If you could make a significant change to the field of pelvic rehab or the field of PT, what would it be?
As a patient advocate, I believe our biggest responsibility as clinicians is to improve access to pelvic rehab and integrated care.
Integrated care I define as “integrative medicine + rehab.” PT’s are not yet the practitioner of choice in many areas, including back and pelvic pain and orthopaedic injury. So we have our work cut out for us – to improve public health education and health literacy about physical therapy and specifically, pelvic PT.
If I had the chance, I would absolutely become involved in evolving the scope of practice and increasing the reach and influence of PT on a legislative and policy level.
What have you learned over the years that has been most valuable to you?
Relationship is more important than anything else.
You can be the most skilled clinician on the planet, and plan the best integrated, “wholistic” biopsychosocial plan of care the world has ever seen – and yet, if you haven’t connected with the patient and nurtured a therapeutic landscape that fosters compassionate care and a safe environment, then patient outcomes will falter. What’s more is, patient frustration and clinician burnout will be high.
When in doubt about what you are doing, return to nurturing relationship.
What is your favorite topic about which you teach?
My courses are like my children. I can’t choose a favorite. I love teaching integrated hip labral care, because it’s difficult and complex subject matter and urgently needed in this rapidly developing new field of hip rehab. But I equally love helping women toward the pregnancy and birth they desire and deserve.
Overall, no matter what the course is, yoga is the entry point for the zen I experience when teaching, practicing integrated physical therapy, and in my personal life. Ultimately, guiding my students and patients toward their own version of that mountain-top experience of personal and professional transformation – that is the real deal.
Ginger Garner, PT, MPT, ATCOther Credentials: PYT, ERYT500, CPI
GingerGarner.com
H&W Courses: HLI, YPREG, YPOST
Update: Please note that this course is now only offered online through the instructor's website. For more information visit https://pelvicpainrelief.com/laser/
Herman & Wallace is announcing a new course on laser therapy for pelvic pain! The Pelvic Rehab Report caught up with the instructor, Isa Herrera.
Laser Therapy For Female Pelvic Pain was developed by Isa Herrera MSPT, CSCS for Herman and Wallace specifically for women’s health clinicians. Ms. Herrera is the author of 4 books, including the breakthrough book, Ending Female Pain, A Woman’s Manual, now in its 2nd Edition. Ms. Herrera has appeared on several national TV and radios shows including on MTV True Life, The Regis and Kelly Show and NBC’s Today Show. She lectures nationally on the topic of women’s health and has been a passionate advocate about pelvic health for over 10 years.
Can you describe the clinical/treatment approach/techniques covered in this continuing education course?
Laser Therapy For Female Pelvic Pain Conditions (LTFPP) is a two-day intensive course that provides the clinician with hands-on experience and treatment protocols using low level laser for the relief female chronic pain conditions that include vestibulodynia, vaginismus, bladder, coccyx and scar pain.
“This class is one in which pelvic floor therapists bring their foundational knowledge of anatomy, neurology and previous training and learn to apply it to laser therapy. “ says Ms. Herrera. “In this class I will share with you my treatment protocols that I have used at my healing center for the last ten years. These treatment protocols are safe and help provide pain relief, reducing injury damage and loss of function. Your patients will oftentimes see immediate results,” she continued.
What inspired you to create this course?
“Clinicians deal with female chronic pain on a daily basis that can be problematic to treat and manage. There is an arsenal of tools, exercises and techniques at their disposal, but many times using a proven modality can help to accelerate the pain-relieving process for the patient. I created this course not only to help the women out there who suffer everyday with debilitating pain, but also to help clinicians achieve even more success with their treatments.”
What resources and research were used when writing this course?
- Atlas Of Clinical Anatomy-Frank Netters
- Grays Anatomy
- Ending Female Pain, 2nd edition, Isa Herrera
- Herman and Wallace PF 1, PF2, PF3
- V Book by Elizabeth G. Stewart and Paula Spencer
- Travell and Simmons Volume 2. Myofascial Pain and Dysfunction: The Trigger Point Manual. The Lower Extremities
- Current Research Articles on Low Level Laser Therapy
Why should a therapist take this course? How can these skill sets benefit his/ her practice?
“This class is for the clinician that is working in the field of women’s health and who typically treats female chronic pain conditions. Clinicians looking for a non-invasive modality, one that is easy to operate and provides reliable and effective treatment options, will see great value in this course. This course provides the clinician with protocols and applicable information on the safe usage of low level laser therapy for female pelvic pain,” says Herrera.

With words like jumping, diving, spiking, hitting, and blocking making up the game's activities, volleyball is clearly a sport that requires a healthy pelvic floor. We know that athletes are at risk for pelvic dysfunction, with symptoms ranging from tension to leakage, but what happens when the pelvic floor is reeducated? In a study addressing volleyball players, researchers assess the effectiveness of a pelvic muscle rehabilitation program on symptoms of urinary incontinence. 32 female athletes were divided evenly between a control group and an experimental group. Inclusions criteria for the sample was nulliparity, symptoms of stress urinary incontinence, age between 13 and 30, and leakage amount more than 1 gram on the pad weight test. Exclusion criteria is as follows: treatment time of less than six months, sport practice for less than two years, urinary tract infections (either current or repeated prior infections), intervention adherence less than 50%, or body mass index outside of the range of 18-25.
Before and after intervention, the athletes were given a baseline questionnaire, a pad test (in the first 15 minutes of volleyball practice), and they completed seven days of a bladder diary to track leakage. The treatment group were instructed in anatomy and physiology of the lower urinary tract, about urinary incontinence (UI) and UI in athletes, and in leakage prevention strategies. A 3-day bladder diary was completed to improve awareness of fluid intake and bladder habits. Pelvic muscle awareness and correct contractions, doing protective pre-contractions of the pelvic floor, and a home exercise program of quick and endurance pelvic muscle contractions in different positions were also instructed.
The results of the intervention include a significant decrease in urinary leakage in the treatment group. The education provided also allowed for prevention of negative coping strategies that were reported in the subjects: the athletes would conceal leakage by wearing a menstrual pad, decreased their fluid intake, or empty their bladder more frequently. This study contributes to the growing body of evidence linking sport to pelvic dysfunction, and more importantly, rehabilitation efforts to improvement. If you want to learn more about pelvic dysfunction in athletes, come to The Athlete and the Pelvic Floor with Michelle Lyons. This 2-day continuing education course took place recently in New York City and your next opportunity to take the class is in Denver in October!
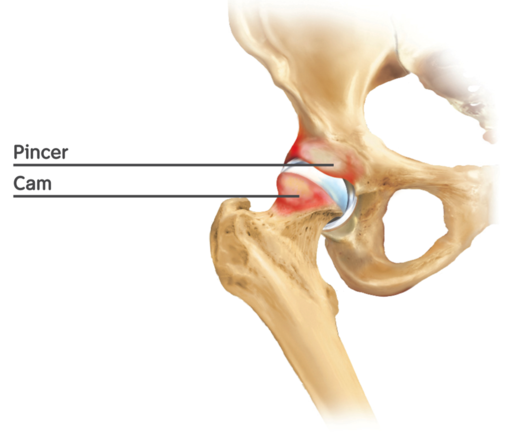
In the treatment of pelvic dysfunction, collaboration among physicians and pelvic rehabilitation providers creates an optimal care situation for the patient. In a research article that will be published in the July issue of Journal of Lower Genital Tract Disease, physical therapist and Herman & Wallace Institute faculty member Stacey Futterman demonstrates how a partnership between disciplines provides information valuable to the field of pelvic rehabilitation. Stacey and physicians Deborah Coady, Dena Harris, and Straun Coleman hypothesized that persistent vulvar pain may be generated by femoroactebular impingement (FIA) and the resultant effects on pelvic floor muscles. Through the research, the authors attempted to determine if hip arthroscopy was a beneficial intervention for vulvar pain, and if so, which patient characteristics influenced improvements.
Twenty six patients diagnosed with generalized, unprovoked vulvodynia or clitorodynia underwent arthroscopy for femoroacetabular impingement. For 3-6 months following hip repair, patients were treated with physical therapy that included surgical postoperative rehabilitation combined with rehabilitation for vulvodynia. Time period for follow-up data collection ranged from 36-58 months. Six patients reported improvements in vulvar pain following surgery and did not require further treatment, and it is noted that these patients were all in the youngest age bracket (22-29). Among the patients who did not report sustained relief, relatively older ages (33-74) were noted, along with a tendency to have vulvar pain for 5 years or longer.
The relationship between hip and pelvic pain may come from the bony structures, hip muscles including but not limited to the obturator internus, and nerves such as the pudendal. The authors conclude that "All women with vulvodynia need to be routinely assessed for pelvic floor and hip disorders…" and if needed, treatment should be implemented to address the appropriate tissue dysfunctions. If you are interested in learning more about hip dysfunction so you can better screen for dysfunction such as femoroacetabular impingement, check out faculty member Steve Dischiavi's continuing education course. Biomechanical Assessment of the Hip & Pelvis: Manual Movement Therapy and the Myofascial Sling System takes place next in Durham, North Carolina in May.
Patients diagnosed with colorectal cancer may undergo a procedure called mesorectal excision as part of their oncology management. In this procedure, a significant portion of the bowel is removed along with the tumor. Total mesorectal excision refers to the entire rectum and mesorectum (peritoneum that connects the upper rectum.) The rectum is removed up to the level of the levator muscles, and this procedure is indicated for tumors of the middle and lower rectum. In a study published in the World Journal of Oncology, the authors report on female urogenital dysfunction following total mesorectal excision (TME).
Questionnaires were returned by 18 women (age range 34-86) who had undergone TME for rectal cancer. Results of the study are summarized in the chart below. (All patients had reported vaginal childbirth, and five had undergone total abdominal hysterectomy and oophrectomy.)
| Presurgical
|
Postsurgical
|
Sexual function
| 5/18 (28%) were sexually active (with no complaints of dyspareunia) | Sexually active patients remained active but all reported discomfort with penetration 2 patients reported decreased libido due to stoma |
Urinary function
| 3/18 (17%) reported urinary urgency and frequency | Of patients with urinary symptoms, 80% persisted longer than 3 months post-surgery |
| 7/18 (39%) reported stress urinary incontinence | |
| New onset symptoms: 61% developed nocturia, 20% developed stress urinary incontinence, 1 patient required permanent catheter |
The authors conclude that rectal cancer treatment can worsen urinary symptoms of nocturia and stress incontinence. Patients who had also been treated with a hysterectomy were found to have more significant symptoms. A proposed mechanism of this increase in symptoms in women who had undergone a hysterectomy is the prior nerve dissection which, when added to the nerve dissection of the inferior hypogastric plexus and the hyogastric nerves for the total mesorectal excision, may have an additive effect. This study which is available full-text, free access, describes further the relationship between the autonomic nervous system in the female pelvis, pelvic function, and the surgery for rectal cancer. Data such as the information provided in this study allow medical providers and their patients to make well-informed decisions about surgeries and quality of life risk factors that may guide medical management of colorectal cancer.
If you would like to feel better prepared to manage post-surgical issues that arise following treatments for colorectal cancer in women, check out the Institute’s Oncology and the Female Pelvic Floor course taught by faculty member Michelle Lyons. This continuing education course happens next in May in Torrance, California.
By accepting you will be accessing a service provided by a third-party external to https://www.hermanwallace.com/










































