
When I was diagnosed with Thyroid Cancer, I’ll be honest, one of my first thoughts was “Thank goodness this won’t directly affect my pelvic floor.” I think as someone who has experienced pelvic floor problems in the past and worked in the pelvic health field for many years, this is probably a somewhat normal reaction, but it wasn’t the standard from my parents and other loved ones. They wanted answers and information and because Thyroid cancer didn’t fall into my niche knowledge of pelvic health, I had to do some research.
Let’s start by saying that thyroid Cancer is the most pervasive endocrine cancer in the world (Bray, 2018). It is the sixth most common cancer in females in the United States (Siegel, 2019). Thyroid cancer incidence and outcomes depend on where the patient lives with Ethiopia and the Philippines having the highest death rates (Deng, 2020). There has been a rise in the diagnosis of thyroid cancer which studies attribute to access to health care, ultrasound, training of those doing the ultrasound, use of fine needle aspiration biopsy, and changes in monitoring and management guidelines (Megwalu & Moon, 2022). The five-year survival rate for people diagnosed with Thyroid Cancer is around 98.5% (Boucai et al. 2024). There are a few types of Thyroid Cancer and Papillary Thyroid Cancer accounts for 84% of all cases (Boucai et al. 2024). There are also follicular, medullary, and anaplastic forms making up the remaining cases (Boucai et al. 2024).
When I tell people I have Thyroid Cancer one of their first questions is “What were your symptoms, how did you know?!” The short answer is, I didn’t know. My cancer journey started when I found out I had a 3 cm nodule that had grown a “significant” amount since my last ultrasound. My endocrinologist said the growth was enough to warrant a fine needle aspiration biopsy. In reading about this diagnosis, it seems many cases of Thyroid Cancers are asymptomatic and detected during a routine physical examination or found incidentally with diagnostic imaging (Boucai et al. 2024).
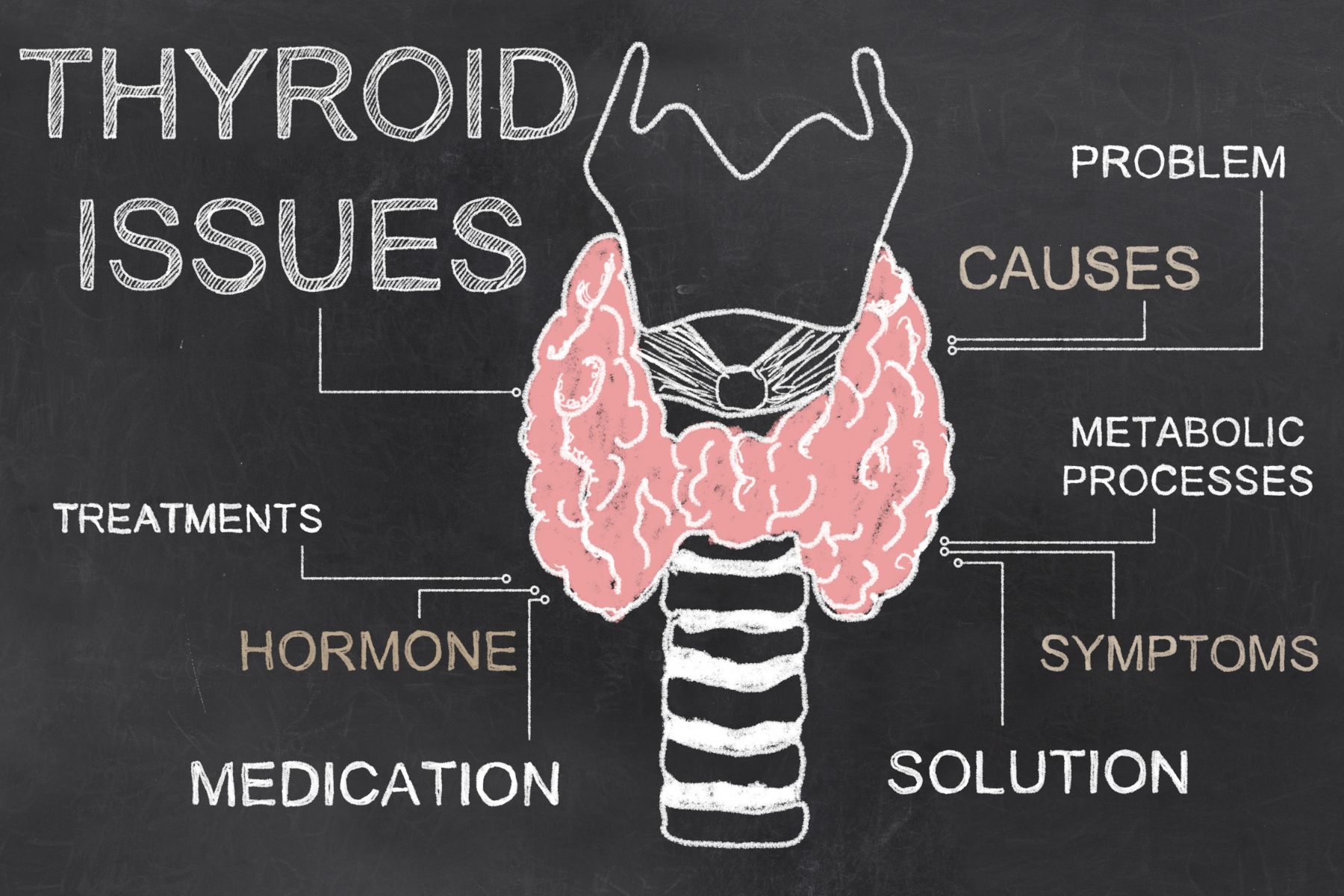 Some other symptoms, mostly related to a growing tumor could include lumps in the throat, a hoarse voice lasting three or more weeks, trouble swallowing or breathing, neck pain/pressure, and swollen cervical lymph nodes. If we had a patient with such complaints, referring them to their primary provider for further diagnostics would be very appropriate. Medullary thyroid cancer does have the ability to increase bowel movements and cause diarrhea and therefore should be on a pelvic health provider’s radar for differential diagnosis. The good news is that the solution to most cases of Thyroid Cancer is surgical removal of the thyroid with the option to perform radioactive iodine ablation treatment. There are other targeted therapies available if the cancer does not respond to radioactive iodine including antiangiogenic multikinase inhibitors and medications for specific genetic mutations (Boucai et al. 2024).
Some other symptoms, mostly related to a growing tumor could include lumps in the throat, a hoarse voice lasting three or more weeks, trouble swallowing or breathing, neck pain/pressure, and swollen cervical lymph nodes. If we had a patient with such complaints, referring them to their primary provider for further diagnostics would be very appropriate. Medullary thyroid cancer does have the ability to increase bowel movements and cause diarrhea and therefore should be on a pelvic health provider’s radar for differential diagnosis. The good news is that the solution to most cases of Thyroid Cancer is surgical removal of the thyroid with the option to perform radioactive iodine ablation treatment. There are other targeted therapies available if the cancer does not respond to radioactive iodine including antiangiogenic multikinase inhibitors and medications for specific genetic mutations (Boucai et al. 2024).
Let’s get to the good part, the therapeutic indications! How can we best support our patients going through Thyroid Cancer or after they have completed treatment?
There are a few things to consider and based on the setting you work on, you may or may not be the one to provide these services.
First, if the patient has a partial or total thyroidectomy, they will have a surgical incision which means a scar to work on and connective tissue restriction. We can help them to mobilize and soften this scar to maintain their cervical range of motion and help the scar to heal better, be less painful, and be more visually appealing. If the therapist has the training, education, and/or application of lymphatic drainage is also very valuable in this healing time.
The patient will have activity restrictions for 1 - 4 weeks depending on the severity of the procedure, including needing rest, eating soft foods, avoiding extremes of ROM of the neck and upper extremities, and regaining vocal control. Working with a patient prior to surgery to review ways to conserve energy and prepare themselves and their home for surgery can be invaluable, especially if the patient doesn’t have a huge support system available post-operatively. Food shopping, meal prepping, and convenience stations set up in the home can make post-operative recovery much smoother.
From personal experience, the throat irritation from the intubation was the most annoying and longest-lasting symptom. My surgeon used electrical stimulation with my intubation to my vocal cords to avoid damage to them. The mucous and hoarseness this created lasted a full 7 days. I still had voice limitations for about a month after and had to work to regain my full voice. Everyone handles pain differently though, and others may feel more pain. My provider, a very seasoned ENT, said they typically found post-thyroid patients had less discomfort than their patients with tonsillectomy or adenoid removal. This can give your patient a benchmark of what to expect if they’ve had one of those surgeries. We can give recommendations to our clients to help with pain management such as using rest, ice, gentle movement, breathing exercises, and meditation to help manage the discomfort, while also taking their pain medication regularly.
As a pelvic floor therapist, as soon as I hear pain medication is involved, I want to make sure that we are keeping the bowels happy. If we have a patient expecting this type of surgery and treatment, we can help guide them to fiber-filled foods and fluid intake to avoid constipation (as long as they don’t have restrictions). If constipation is not something they typically experience, this may be their first introduction to things like osmotic laxatives and a squatty potty and we can be the person who presents them with this education if they need it.
There will be a few things going on hormonally after the surgery. Because the thyroid has been removed, the patient will be hypothyroid unless they take synthetic thyroid hormone or have a partial thyroidectomy where the remaining half has continued to function and adjust. Hypothyroidism can cause many symptoms, but related to our patients in pelvic health, we might see constipation, fatigue, skin changes, menstrual cycle changes, musculoskeletal complaints, and intolerance to temperature changes. If we see our patient experiencing any of these, we can refer them back to their provider to have their levels checked. We can also tailor our plan of care to adjust for some of these things.
 Another more life-threatening complication that can happen is disruption of the parathyroid glands. These produce the calcium needed to regulate muscles and nerves. With calcium levels too low, a person can experience some uncomfortable and possibly dangerous symptoms such as feeling foggy and confused, muscle tremors, heart arrhythmias, and even seizures if the levels get too low. These little guys sit right under the thyroid and can be traumatized or accidentally removed with the thyroid. After surgery, patients will likely be taking a calcium supplement and have instructions to take it if they feel this way, but they may need a reminder from their very caring and observant therapist.
Another more life-threatening complication that can happen is disruption of the parathyroid glands. These produce the calcium needed to regulate muscles and nerves. With calcium levels too low, a person can experience some uncomfortable and possibly dangerous symptoms such as feeling foggy and confused, muscle tremors, heart arrhythmias, and even seizures if the levels get too low. These little guys sit right under the thyroid and can be traumatized or accidentally removed with the thyroid. After surgery, patients will likely be taking a calcium supplement and have instructions to take it if they feel this way, but they may need a reminder from their very caring and observant therapist.
When we think about how else Thyroid Cancer could affect our patients, I think it is important to consider the emotional aspect. Even though it’s a very common, easy-to-treat cancer with a high “cure rate,” it is still cancer. From personal experience, providers are so used to treating more sick people, that they have an almost blase attitude towards the treatment. I’ve spoken to others with endocrine cancer and heard similar stories. We have the “friendly” cancer, why stress or make haste about anything? There is a lack of haste or urgency, which can feel disconcerting when you just want to be cancer-free ASAP.
The incision, if surgery is needed, is directly to the anterior aspect of the neck. It's hard to hide the scar unless you wear a turtleneck. Most surgeons try to make the incision in a fold of the neck, but this may not be possible if lymph nodes also need to be dissected. Scars also take about a year to remodel and “silver.” We can further help our patients feel more confident with their scars by reminding them to avoid sunlight and utilize silicone patches to soften and protect the area to allow the scar to mature into a minimally noticeable line. There is still a reminder every time the patient looks in the mirror and this may affect all aspects of their life including their confidence in areas like sexual intimacy.
The last area to consider would be if a person needs the radioactive iodine treatment. Although this treatment is not “aggressive” like chemo or traditional targeted radiation, it can be a stressor to a patient. Radioactive iodine ablation has an extensive prep, multi-procedure application, and post-treatment quarantine phase that can be very disruptive to a person’s life. Pelvic health providers won’t be actively managing this phase, but being a friendly ear to bounce iodine-free recipe ideas off of and commiserate with the inability to ingest dairy for 3+ weeks can help make your patient feel supported and heard.
I have been fortunate enough to take Herman & Wallace’s Oncology series and so I felt prepared to treat and manage patients with these types of cancer. It was my own Thyroid Cancer journey that gave me hands-on experience with what it is like to be a cancer patient. It's been interesting to have to advocate in a medical system that doesn’t always listen to patients. I’ve also had to re-find who I am after having a pretty significant medical episode. These experiences always help give me perspective to be a better provider to my patients and bring more personalized care to them. I encourage you to take these classes, as cancer really affects so many lives. My most comforting providers during this time have been those who have taken the time to answer my questions, hold space for my worries, and have humor with me during this bizarre time.
The HW Oncology Series includes:
- Oncology of the Pelvic Floor Level 1 - Introduction (*Certified Lymphatic Therapists may skip this course)
- The next scheduled course is on November 2-3
- Oncology of the Pelvic Floor Level 2A - Male Pelvic and Colorectal Cancers
- The next scheduled course is on September 7-8
- Oncology of the Pelvic Floor Level 2B - Urogynecological Cancers
- The next scheduled course is on December 7-8
References:
- Bray, F., Ferlay, J., Soerjomataram, I., Siegel, R. L., Torre, L. A., & Jemal, A. (2018). Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians, 68(6), 394-424.
- Boucai, L., Zafereo, M., & Cabanillas, M. E. (2024). Thyroid cancer: a review. Jama, 331(5), 425-435.
- Deng, Y., Li, H., Wang, M., Li, N., Tian, T., Wu, Y., ... & Dai, Z. (2020). Global burden of thyroid cancer from 1990 to 2017. JAMA network Open, 3(6), e208759-e208759.
- Megwalu, U. C., & Moon, P. K. (2022). Thyroid cancer incidence and mortality trends in the United States: 2000–2018. Thyroid, 32(5), 560-570.
- Siegel RL, Miller KD, Jemal A 2019 Cancer statistics, 2019. CA Cancer J Clin 66:7–30.
AUTHOR BIO:
Mora Pluchino, PT, DPT, PRPC

I am a graduate of Stockton University with my BS in Biology (2007) and Doctorate of Physical Therapy (2009). I have experience in a variety of areas and settings, working with children and adults, including orthopedics, bracing, neuromuscular issues, vestibular issues, and robotics training. I began treating Pelvic Health patients in 2016 and now have experience treating women, men, and children with a variety of Pelvic Health dysfunction. There is not much I have not treated since beginning this journey and I am always happy to further my education to better help my patients meet their goals.
I strive to help all of my patients return to a quality of life and activity that they are happy with for the best bladder, bowel, and sexual functioning they are capable of at the present time. In 2020, I opened my own practice called Practically Perfect Physical Therapy Consulting to help meet the needs of more clients. I have been a guest lecturer for Rutgers University Blackwood Campus and Stockton University for their Pediatric and Pelvic Floor modules since 2016. I have also been a TA with Herman & Wallace since 2020 and have over 150 hours of lab instruction experience.
The diagnosis of chronic constipation may seem like a simple concept; however, bowel patients can be a challenging group within our pelvic health population. The interesting part about treating these patients is that constipation can result in a variety of complaints. Diaz et al confirmed this in their 2023 research. Their article shared that “Constipation encompasses several subtypes, each with its unique characteristics and underlying factors.”(1) Common complaints can include frequency, size, length, and consistency which can become overwhelming for the practitioner to decide which clinical complaints seem the most important to focus on.
Knowing how to effectively treat these patients and ask the right questions is valuable in the scheme of pelvic floor rehab, secondary to overlapping symptoms and etiology of chronic constipation. Consideration needs to be taken into account for any outside factors that can also contribute to patient complaints. For example, taking different prescription medications, supplements, and eating different foods can all influence the patient's stool frequency and formation (2). Realizing where this issue stems from is the deep-dive question to get a handle on their complaints.
Bowel frequency can be one of the biggest clinical challenges for clinicians to educate patients to master – consistency is key! Understanding what their normal frequency should be, or what it should be now, is part of the clinical judgment skill when setting goals. If your patient is only getting a natural bowel movement urge every 10 days, their goal of daily BMs, at first, should be emotionally readjusted so that they don’t feel like they have failed their rehabilitation goals.
Learning colon physiology helps to understand normal vs abnormal motility and can be helpful in treating your patient’s constipation. In my course, Bowel Pathology and Physiology we discuss the physiological reflex that controls the lower motility of the GI tract following a meal (3). When patients present with chronic constipation, they may be experiencing a profound loss of the gastrocolic reflex. The course is filled with clinical pearls and research tidbits that help to improve or slow down colonic motility. Join me in the next course offering on September 14-15, 2024 to learn more.
Resources:
- Diaz S, Bittar K, Hashmi MF, et al. [Updated 2023 Nov 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK513291/
- Araújo MM, Botelho PB. Probiotics, prebiotics, and synbiotics in chronic constipation: Outstanding aspects to be considered for the current evidence. Front Nutr. 2022 Dec 8;9:935830. doi: 10.3389/fnut.2022.935830. PMID: 36570175; PMCID: PMC9773270.
- Mawer S, Alhawaj AF. Physiology, Defecation. 2023 Nov 13. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 30969554.
AUTHOR BIO
Lila Abbate, PT, DPT, MS, OCS, WCS, PRPC
 Lila Abbate is the Director/Owner of New Dimensions Physical Therapy. She graduated from Touro College in Dix Hills, NY with a Bachelor of Science (BS) in Health Sciences and a Master of Arts (MA) in Physical Therapy in 1997. She completed her Advanced Masters in Manual Orthopedic Physical Therapy (MS) at Touro College, Bayshore, NY in 2003 and continued to pursue her Doctor of Physical Therapy (DPT) at Touro in 2005. Dr. Abbate is a Board-Certified Specialist by the American Physical Therapy Association in Orthopedics (OCS) 2004 and Women’s Health (WCS) 2011. She obtained the Certified Pelvic Rehabilitation Practitioner (PRPC) from the Herman & Wallace Institute in 2014. She is a Diane Lee/LJ Lee, Integrated Systems Model (ISM) graduate and completed the New York series in 2012.
Lila Abbate is the Director/Owner of New Dimensions Physical Therapy. She graduated from Touro College in Dix Hills, NY with a Bachelor of Science (BS) in Health Sciences and a Master of Arts (MA) in Physical Therapy in 1997. She completed her Advanced Masters in Manual Orthopedic Physical Therapy (MS) at Touro College, Bayshore, NY in 2003 and continued to pursue her Doctor of Physical Therapy (DPT) at Touro in 2005. Dr. Abbate is a Board-Certified Specialist by the American Physical Therapy Association in Orthopedics (OCS) 2004 and Women’s Health (WCS) 2011. She obtained the Certified Pelvic Rehabilitation Practitioner (PRPC) from the Herman & Wallace Institute in 2014. She is a Diane Lee/LJ Lee, Integrated Systems Model (ISM) graduate and completed the New York series in 2012.
Dr. Abbate has been an educator for most of her physical therapy career. She has experience as a full-time faculty at Touro College, Manhattan Campus from 2002 to 2006 teaching the biomechanical approach to orthopedic dysfunction and therapeutic exercise as well as massage/soft tissue work that highlighted trigger point work, scar management, and myofascial release. She is currently on faculty as a Lecturer at Columbia University teaching the private practice section Business & Management course (since 2016) along with the Pelvic Health elective (since 2012). She teaches nationally and internationally with the Herman & Wallace Pelvic Rehabilitation Institute teaching advanced courses of her own intellectual property: Orthopedic Assessment for the Pelvic Health Therapist, Bowel Pathology Function, Dysfunction and the Pelvic Floor, Coccydynia & Painful Sitting: Orthopedic Implications. She was a co-writer for the Pudendal Neuralgia course and teaches the Pelvic Function Series, and Pregnancy/Postpartum Series. She has written two book chapters in 2016: Pelvic Pain Management by Valvoska and Healing in Urology: Clinical Guidebook to Herbal and Alternative Therapies by Chughtai.
Lila is a member of the American Physical Therapy Association, the National Vulvodynia Association, the American Urogynecology Association, the International Pelvic Pain Society, and is also a Senior Physical Therapy consultant for SI Bone, a sacroiliac joint instrumentation company.
Dawn is debuting a new course, Pediatric Postural Development, with Herman & Wallace on September 29, 2024.
Most physical and occupational therapists learn about one diaphragm in school: the respiratory diaphragm. But did you know that Osteopathic Manipulative Medicine recognizes 5 different diaphragms within the body? They include tentorium cerebelli, tongue, thoracic outlet, respiratory diaphragm, and pelvic floor. (1)
The intricate myofascial connections between all these diaphragms are fascinating! But as a pediatric pelvic floor therapist, what’s the significance of these connections when you look at kids’ functional mobility and strength?
The pelvic floor and respiratory diaphragm are the two main structures that we’ll be discussing today. You’ll learn how they develop during infancy and childhood and how their functional relationship affects your assessment and treatment for kids with bowel and bladder dysfunction.
Development Of The Pelvis, Spine, And Diaphragm During Infancy
Pelvic Structure At Birth
 Pelvic structure and spinal curvatures develop based on the activities of infants and young children. The educational role that you have as a pediatric therapist is significant during a child’s first years of life, especially for children with congenital or developmental delays. Doing your best to help them achieve these developmental goals will greatly affect their life in later years.
Pelvic structure and spinal curvatures develop based on the activities of infants and young children. The educational role that you have as a pediatric therapist is significant during a child’s first years of life, especially for children with congenital or developmental delays. Doing your best to help them achieve these developmental goals will greatly affect their life in later years.
At birth, the pelvis of the baby is funnel shaped and the respiratory diaphragm is oblique. You can observe a neonate with a wide rib cage, which only allows for a short descent of the ribs. You can hear evidence of this as a newborn’s cry is very short. At this time, their pelvic floor has no posture.
Cervical Lordosis
The first curve to develop in an infant is cervical lordosis. Neck control improves as the head is challenged against gravity. In an upright position, the neck is challenged to maintain a neutral position. In prone, the neck is challenged to extend and re-enforces a lordotic curve.
Tummy time is important to begin at a young age. Not only do kids develop neck and core strength, but extending the neck in a prone establishes proper cervical lordosis for later in life.
Thoracic Kyphosis And Ribcage
Thoracic kyphosis develops when a child begins sitting. Again, thinking about sitting from a trunk control perspective is important, but establishing proper kyphotic alignment should not be overlooked. A mild degree of kyphosis is normal, but congenital deformities can exaggerate children’s kyphosis and increase the difficulty of achieving good sitting posture.
Independent sitting is an important milestone itself and further affects: (2)
- object perception
- language development
- spatial memory
- visual processing
- overall cognition
When treating infants, let’s remember to teach how important the skill of independent sitting is. We will discuss this further in the last section and how it relates to pelvic floor function.
As an infant increases their activity in the quadruped position, the diaphragm angle gets steeper inside the ribcage. This angle also increases through weight-bearing positions and with the development of the scapular stabilizers around the ribcage.
Lumbar Lordosis And Sacrum
Standing influences lumbar lordosis. Once again, standing challenges core stability and develops strength. But also recognize how standing helps the child establish proper lordotic lumbar posture.
Furthermore, in standing, the diaphragm orientation changes. The diaphragm becomes more parallel to the pelvic floor. As the diaphragm establishes a more horizontal orientation with standing and walking, the muscular tone increases as it responds to the vertical pressure and pull of the viscera.
This upright position also develops the pelvic floor to counteract the pressure of the viscera being pulled down by gravity. Counternutation of the sacrum protects the pelvic floor from full visceral pressures.
Let’s take a look at the functional relationship as the diaphragm and pelvic floor develop.
Functional Relationship Of Diaphragm And Pelvic Floor During Childhood
 When the diaphragm and pelvic floor are developed in their horizontal orientations, they begin moving together during breathing. When inhaling, the diaphragm and pelvic floor descend as the ribcage and abdominal cavity expand. When exhaling, the diaphragm and pelvic floor ascend. The continued alternating movement mobilizes the viscera and creates a lymphatic pump.
When the diaphragm and pelvic floor are developed in their horizontal orientations, they begin moving together during breathing. When inhaling, the diaphragm and pelvic floor descend as the ribcage and abdominal cavity expand. When exhaling, the diaphragm and pelvic floor ascend. The continued alternating movement mobilizes the viscera and creates a lymphatic pump.
This relationship between the diaphragm and pelvic floor is why it’s so important to look at breathing mechanics in kids. Ribcage mechanics and good diaphragm strength and tone affect the mobilization of the viscera, including the stomach and intestines. This is especially relevant when treating kids with constipation.
If you watch constipated children breathe, you will notice that they often breathe more anteriorly through their bellies instead of up and down. You will also notice minimal or no expansion of the ribcages.
Additionally, when the viscera descend, this cues the pelvic floor to activate and continue developing. Around ages 2-3, the pelvic floor develops enough stretch to react to bowel and bladder function. This is the age when children typically develop urinary continence.
Although therapists usually use the term pelvic “floor”, it’s important for you to consider this as a “diaphragm”. The pelvic “diaphragm” is a dynamic partition that serves to adjust pressures and pump fluids within the body.
Lymphatics throughout the trunk, head, and limbs are all regulated by the pumping of the body’s five diaphragms. The diaphragms work together to regulate pressures, pulling fluids and toxins into the lymph system to detoxify the body. The colon has a great lymphatic network, so this is especially important in kids with bowel issues.
Now you understand how the respiratory diaphragm and pelvic floor influence function in typically developing children. What about kids with impaired functional mobility or impaired gross motor delays? Let’s dive into these considerations.
Pediatric Postural Impairments And Gross Motor Developmental Delays
 Children with physical developmental delays will have delayed pelvic floor control as well. As you learned earlier in this blog, establishing control in positions including prone, sitting, quadruped, and standing, develops a baby’s spinal curvatures.
Children with physical developmental delays will have delayed pelvic floor control as well. As you learned earlier in this blog, establishing control in positions including prone, sitting, quadruped, and standing, develops a baby’s spinal curvatures.
If children have conditions such as spina bifida or cerebral palsy, those developmental positions may be delayed or sometimes never reached.
Improper spinal curvature early in life will affect a child’s ability to attain or maintain postural positions required for voiding and defecation. This will also delay the development of the relationship between the diaphragm and pelvic floor control.
Start looking at these milestones not only from your perspective of postural control and gross motor function but also to help improve their bowel and bladder function:
- holding head up in prone
- sitting independently
- quadruped reaching and crawling
- standing independently
- walking
If a child never stands or walks, they will struggle to develop diaphragm and pelvic floor control because gravity will not challenge this system. Spending time in upright positions by using assistive devices such as standers or walkers will help develop respiratory capacity and pelvic floor control.
When you have this treatment outlook, you can help parents shift their perspectives too. Parents of children with disabilities are often overwhelmed and tired. Help them to understand the benefits of continued work in practicing and attaining developmental postural and motor skills.
 The new course, Pediatric Postural Development debuts on September 29, 2024 and focuses on the role of the pelvic floor, diaphragm, and core. This one-day course is designed to help therapists understand the development of the diaphragm and pelvic floor muscles (PFM) as they relate to core function and continence in children. Learn how to connect the ribcage, the diaphragm, and the pelvic floor for proper core activation, as well as receive instruction in anatomy and development of the diaphragm and its relationship to the pelvic floor/core. The information presented in the course applies to children who have been diagnosed with Cerebral Palsy, Down syndrome, ASD, Hypotonia, and more.
The new course, Pediatric Postural Development debuts on September 29, 2024 and focuses on the role of the pelvic floor, diaphragm, and core. This one-day course is designed to help therapists understand the development of the diaphragm and pelvic floor muscles (PFM) as they relate to core function and continence in children. Learn how to connect the ribcage, the diaphragm, and the pelvic floor for proper core activation, as well as receive instruction in anatomy and development of the diaphragm and its relationship to the pelvic floor/core. The information presented in the course applies to children who have been diagnosed with Cerebral Palsy, Down syndrome, ASD, Hypotonia, and more.
References:
- Bordoni B. The Five Diaphragms in Osteopathic Manipulative Medicine: Myofascial Relationships, Part 1. Cureus. 2020 Apr 23;12(4):e7794. doi: 10.7759/cureus.7794. PMID: 32461863; PMCID: PMC7243635.
- Kretch, K. S., Marcinowski, E. C., Hsu, Y., Koziol, N. A., Harbourne, R. T., Lobo, M. A., & Dusing, S. C. (2023). Opportunities for learning and social interaction in infant sitting: Effects of sitting support, sitting skill, and gross motor delay. Developmental Science, 26(3), e13318. https://doi.org/10.1111/desc.13318
Special thanks to Dawn for allowing The Pelvic Rehab Report to reprint her article, originally published on her website at kidsbowelbladder.com.
AUTHOR BIO:
Dawn Sandalcidi PT, RCMT, BCB-PMD
 Dawn Sandalcidi is a trailblazer and leading expert in the field of pediatric pelvic floor disorders. She graduated from SUNY Upstate Medical Center in 1982 and is actively seeing patients in her clinic Physical Therapy Specialists, Centennial CO.
Dawn Sandalcidi is a trailblazer and leading expert in the field of pediatric pelvic floor disorders. She graduated from SUNY Upstate Medical Center in 1982 and is actively seeing patients in her clinic Physical Therapy Specialists, Centennial CO.
Dawn is a national and international speaker in the field, and she has gained so much from sharing experiences with her colleagues around the globe. In addition to lecturing internationally on pediatric bowel and bladder disorders, Dawn is also a faculty instructor at the Herman & Wallace Pelvic Rehab Institute. Additionally, she runs an online teaching and mentoring platform for parents and professionals.
In 2017, Dawn was invited to speak at the World Physical Therapy Conference in South Africa about pediatric pelvic floor dysfunction and incontinence. Dawn is also Board-Certified Biofeedback in Pelvic Muscle Dysfunction (BCB-PMD). She has also been published in the Journals of Urologic Nursing and Section of Women’s Health.
In 2018, Dawn was awarded the Elizabeth Noble Award by the American Physical Therapy Association Section on Women's Health for providing Extraordinary and Exemplary Service to the Field of Physical Therapy for Children.

Ask yourself these 5 questions:
- Do you understand the importance of conducting medication reviews with all your patients?
- Can you confidently discuss the medications used in the treatment of pelvic floor, gastrointestinal (GI), and genitourinary conditions?
- Are you able to describe the common side effects of medications routinely used in pelvic health?
- Can you analyze the impact medications may have on a patient’s complaints and their treatment plan and outcomes?
- Are you able to effectively communicate with patients and other healthcare providers about medications?
If you answered "no" to any of these questions or are preparing for an upcoming PRPC or WCS exam, the Pharmacologic Considerations for the Pelvic Health Provider course is designed for you!
The Role of Medication Review in Rehabilitation Therapy
While managing medications is not within the scope of practice for rehabilitation therapists, it is crucial to review patient medications during the initial evaluation and on an ongoing basis. Therapists must assess the impact of medications on treatment and patient outcomes to ensure patient safety.
Why Pharmacology Knowledge Matters!
Aging Population: With an aging population, many patients over the age of 65 are on more than five medications, increasing the risk of side effects, adverse drug reactions, and drug interactions.
Informed Discussions: A solid grasp of pharmacology allows therapists to engage in informed discussions with patients and collaborate effectively with other healthcare providers.
Alternative Approaches: Understanding pharmacology enables therapists to explore recent medications, supplements, or alternative approaches that may minimize side effects, mitigate impacts on quality of life, and enhance function.
Evidence-Based Practices: Keeping current on advancements in pharmacology is essential for delivering effective, evidence-based physical therapy interventions.
Benefits of Pharmacology Understanding in Rehabilitation
Safe and Effective Treatment: A thorough understanding of pharmacology helps provide safe and effective treatment.
Optimized Rehab Strategies: Knowledge of pharmacology allows therapists to optimize rehabilitation strategies.
Patient Empowerment: Educating patients about their medications empowers them to make informed decisions.
Recognizing Red Flags: Identifying potential red flags related to medication use.
Improved Collaboration: Pharmacology knowledge improves collaboration with other healthcare providers.
Course Offering
Join Kristina Koch for the virtual course Pharmacologic Considerations for the Pelvic Health Provider on August 17th to deepen your understanding and stay up-to-date on the medications used in treating pelvic floor and women's and men's health dysfunctions. This course will provide you with the essential knowledge to confidently manage medication-related aspects of patient care, ensuring better outcomes and enhanced patient safety.
AUTHOR BIO
Kristina Koch, PT, DPT, MS, Board Certified Specialist in Women's Health PT (2013-2023), CLT

Kristina received her Master of Science in Physical Therapy in 1996 from Springfield College in Massachusetts. In 2001, while living in the Los Angeles area, Kristina started specializing in the treatment of pelvic floor dysfunction including bowel/bladder issues and pelvic pain, and in 2021, she went on to earn her doctorate of physical therapy from The College of St. Scholastica. During her time in Los Angeles, she was fortunate to work with and, be mentored by fellow Herman and Wallace faculty member, Jenni Gabelsburg, DPT, WCS, MSc, MTC. Kristina is a Board Certified Specialist in Women's Health Physical Therapist (2013-2023) by the American Board of Physical Therapy Specialties. She then received her lymphatic therapist certification (CLT) in 2015.
Kristina has successfully helped establish women’s health and pelvic floor physical therapy programs in San Diego, California, and Colorado Springs, CO where she currently works in private practice. Kristina treats men, women, children, trans and gender non-binary individuals in her practice. In addition, Kristina serves as a guest lecturer for graduate physical therapy students at Regis University in Denver, CO, and provides educational lectures to medical providers and local community groups. Outside of work, Kristina enjoys spending time with her husband and two children, skiing, running, and hiking.

Sacroiliac joint pain can be a challenging condition to treat. One of the clinical pearls that I feel changed my practice for the better is the palpation and direct treatment of the dorsal sacral ligament. At a course many years ago, I listened to Diane Lee describing Andry Vleeming's work addressing the potential role of the long dorsal sacral ligament (LDL) in pelvic pain. His valuable research was conducted on women who had complaints of peripartum pain, and it has been my experience that the information is easily extrapolated to other patient populations.
Vleeming and colleagues describe the long dorsal sacroiliac ligament anatomy as attaching to the lateral crest of the 3rd and 4th sacral segments (and sometimes to the 5th segment), and as having connections to the aponeurosis of the erector spine group, the thoracolumbar fascia, and the sacrotuberous ligament. Functionally, nutation in the sacroiliac joint will slacken the ligamentous tension in the LDL and counternutation will tension the ligament. This structure can be palpated directly caudal to the posterior superior iliac spine (PSIS).
The referenced study examined women who had tenderness in the LDL and were also diagnosed with peripartum pelvic pain. Patients included in the study had pain in the lumbopelvic region, pain beginning with pregnancy or within 3 weeks of childbirth, were not pregnant at the time of the study, and were between the ages of 20-40. In patients with peripartum pelvic pain, 76% of the women reported tenderness in the LDL- this number increased to 86% when only patients scoring positively on the active straight leg raise test and posterior pelvic pain provocation (PPPP) test were included.
The study proposes that strain in the LDL may occur from a counter-stated sacrum and/or an anterior pelvic tilt position. In my clinical experience and as instructed to many pelvic health therapists by expert clinicians such as Diane Lee, balancing the pelvic structures, activating stabilizing muscles of the inner core (pelvic floor, multifidi, transverses abdominis), and addressing soft tissue dysfunction in the ligament frequently resolve long-standing localized pain in the sacroiliac joint area. The authors of the study conclude that "…knowledge of the anatomy and function of the LDL and the simple use of a pain provocation test…could help gain a better understanding of peripartum pelvic pain." They also reported that combining tests such as the ASLR, the PPPP test, and the long dorsal sacral ligament palpation test "seems promising" in the differentiation of patients categorized as having pelvic pain versus lumbar pain.
To learn more about sacroiliac joint anatomy and function, diagnosis, and treatment then sign up for Steve DIschiavi's upcoming remote course Sacroiliac Joint Current Concepts scheduled for August 4, 2024.
Reference:
1. Vleeming A, de Vries HJ, Mens JM, van Wingerden JP. Possible role of the long dorsal sacroiliac ligament in women with peripartum pelvic pain. Acta Obstet Gynecol Scand. 2002 May;81(5):430-6. doi: 10.1034/j.1600-0412.2002.810510.x. PMID: 12027817.

The HW admin team has been hard at work filling speaker spots, building breakout sessions, and creating fun new experience ideas for the upcoming 2025 conference.
If you're into pelvic health then this is the conference for you. HWConnect was created to provide a top-tier networking event for pelvic rehabilitation practitioners that focuses on providing a safe environment for professional development, exposure to new products, and sharing inspiration for all things pelvic health.
HWConnect features keynote speakers, breakouts, labs, and educational sessions. Topics range from pediatrics with Dawn Sandalcidi to gender-affirming care with Ken McGee. HWConnect is all about connection - the name says it all. Network. Learn. Grow. Repeat. 
Registering is as easy as 1, 2, 3!
- Complete online registration.
- Book travel and lodging. HWConnect will be held at the Hilton Seattle Airport & Conference Center and HW has special pricing set up for attendees.
- Show up, and don't forget to stop by and say hello to all of your favorite HW team members!
Need More Information?
- Keynote Speakers are the indomitable Dawn Sandalcidi, PT, RCMT, BCB-PMD (she/her), Nancy Norton, RN (she/her), and Leticia Nieto, PsyD, LMFT, TEP (she/her).
- Speakers include Ken McGee, PT, DPT (they/he), Dr. Cindy Mosbrucker (she/her), Meryl Alappattu, PT, PhD (she/her), and Carole High Gross, PT, DPT, PRPC (she/her).
- Breakout sessions, workshops, and labs include yoga, meditation, rehabilitative ultrasound imaging, squat analysis, and MORE - all led by your favorite HW faculty including Dustienne Miller, Nari Clemons, and Allison Ariail.
- HW proudly welcomes second-time conference sponsor CMT.
- Vendor Hall featuring exhibitors including Intimate Rose, Slippery Stuff, and Raise the Pelvic Floor.
- Non-profit booths feature the Kenya Scholarship Foundation and Open Arms Perinatal Services. Read this past blog to learn more about the Kenya Scholarship Foundation.
- Special Podcast Guests feature Callie and Rachel from Pelvic Service Announcement (PSA) and Courtney from Raise the Pelvic Floor.
For more information and a full lineup check out the HWConnect 2025 page!
Already Coming to HWConnect?
That's amazing!
Herman & Wallace would love your help spreading the word about HWConnect 2025 and the chance to connect with the amazing people in our community. Check out this page where you can review and share all the programming we’ve booked thus far. https://hermanwallace.com/connect-2025
We look forward to seeing you at HWConnect 2025!

Anyone working in pelvic health knows all too well that the symptoms of female pelvic floor dysfunction (PFD) — from bladder leaks and pain with vaginal penetration to anal pain and fecal incontinence — are vastly underreported. Most providers do not screen for pelvic health symptoms and patients are either reluctant to bring them up or assume that they’re ‘just the way it is’ if you own a uterus (and especially if you’ve had kids).
Just how underreported are pelvic health symptoms? That’s one of the questions that the 2024 Origin Pelvic Health Study sought to answer. The consumer-facing study consisted of a 10-minute, double-blinded, online, quantitative survey conducted by the market research firm Ipsos, with a base sample of 612 U.S. women, ages 18-59.
Study participants were asked whether they had experienced bladder, bowel, and sexual symptoms in the past year, how those symptoms had impacted their lives, and whether they had gotten care for their symptoms. Additional questions were asked of those who had given birth within the past five years or who were in peri/menopause to both explore how these major life events impact pelvic health symptoms and reveal gaps in related care and education.
As a clinical reviewer of the study and an APTA Pelvic Health grant recipient working on my own research, I’m excited that companies like Origin are collecting this valuable data, which not only garners media attention that can be hard for pelvic health researchers to attain (the Origin study was written up in Vogue), it can help inspire and steer our research in important new directions.
The study includes too many eye-opening statistics to list here, but below are 3 high-level takeaways:
- The majority of U.S. women ages 18-59 are dealing with multiple pelvic health symptoms.
PFD has most recently been found to impact 1 in 3 women, based on a 2022 study that examined the medical records of 25,425 women seeking primary care. ICD-10 codes were used to determine presence of PFD, including urinary incontinence, pelvic organ prolapse, bowel, dysfunction, and difficult defecation. Other pelvic floor-related conditions like vulvovaginal pain or orgasm difficulty were not included.
In contrast, the Origin study included a long list of pelvic health symptoms described in terms women often use themselves, with the goal to expose just how common these symptoms really are. What they found was that most women had one or more symptoms, and only a tiny minority had received care for them.
75% of U.S. women between the ages of 19 and 58 have dealt with two or more pelvic health symptoms within the past year. The average number of pelvic symptoms reported was 5.
Some of the symptoms experienced most often in the past year by U.S. women ages 18-59:
Bladder sypmtoms:
- 48% report bladder leaks when they cough, sneeze or exercise
- 38% report peeing more than once every 2 hours
- 37% report feeling like they had to pee again right after going
- 33% report feeling like they could barely hold their pee
- 27% report feeling like they couldn’t fully empty their bladder
Bowel symptoms:
- 52% report straining to have a bowel movement
- 48% report feeling like they can’t fully empty their bowels
- 29% report pain with having a bowel movement
- 21% resort leaking gas or poop
Sexual symptoms:
- 33% report inability to orgasm
- 25% report unsatisfying orgasm
- 22% report pain with sex
- 18% report delayed orgasm
Interestingly, the study also found that Millennial women were more likely to report a host of symptoms in the past year, compared to Gen X.
- Pregnant and postpartum patients are left in the dark when it comes to preparing for and recovering from the immense physical strain of childbirth.
As major health organizations seek to improve the current dire state of postpartum care, mentions of pelvic health and pelvic floor physical therapy are often limited to recommendations that postpartum patients be evaluated for urinary and fecal incontinence and referred to pelvic floor PT as needed.
Those of you who are women’s health specialists who focus on prenatal and postpartum PT, know that we have so much more to offer. The Origin Study highlighted the need for the exact guidance and expertise that pelvic floor PTs can provide.
Among women who had given birth with in the past 5 years:
- 85% report receiving no guidance on reducing their risk of tearing during childbirth.
- 65% report receiving no guidance on how to effectively push out a baby.
- 50% report receiving no guidance on how to manage pregnancy pain.
- 86% report receiving no guidance on how to heal their pelvic floor after childbirth.
- 83% report receiving no guidance on how to heal their abdominals after pregnancy and childbirth.
- 71% said they received no guidance on how to exercise safely before or after childbirth.
In addition, 44% of women who had a baby in the past 5 years say providers did not help them understand what is or isn’t normal in terms of their pelvic health systems. And 23% said they felt “not at all supported” by their medical providers during their postpartum recovery.
- Pelvic floor PT continues to be underutilized, resulting in unnecessary pain and suffering for women of all ages.
It’s unlikely to surprise you that, of the Origin study participants who reported pelvic health symptoms within the past year, 96% had not received medical care for their symptoms. Of study respondents who had given birth within the past 5 years, 92% said they had not seen a pelvic floor PT to support their recovery after their most recent delivery.
Without proper screening by providers and referrals to pelvic floor PT, women will continue to suffer in silence, confused about what is and isn’t normal when it comes to their pelvic health.
The Origin study reiterates what pelvic health specialists and their patients already know — pelvic health symptoms significantly disrupt women’s lives. 64% of study respondents who report pelvic health symptoms in the past year say that these symptoms negatively impact their lives. And that number is even higher among women who have given birth within the past 5 years, at 79%.
Despite how discouraging it can be to read through these statistics, it’s important to get loud about them and continue to demand better. I’m grateful to my colleagues at Origin for making research part of their mission and am excited to see this data is used to fuel more research, draw more attention to pelvic health, and drive positive change in our healthcare system.
AUTHOR BIO:
Jessica Swartz, PT, DPT, CCI
 Jessica Swartz, PT, DPT, CCI, is a physical therapist at Origin, a leading provider of pelvic floor and whole-body physical therapy with a special focus on pregnancy and postpartum. She is also working on her PhD in Public Health with an emphasis on Health Behavior in the Joint Doctoral Program of Public Health at UC San Diego/San Diego State University, where the focus of her research is developing ways to use physical therapy as a tool to improve women’s and maternal health outcomes and address health disparities.
Jessica Swartz, PT, DPT, CCI, is a physical therapist at Origin, a leading provider of pelvic floor and whole-body physical therapy with a special focus on pregnancy and postpartum. She is also working on her PhD in Public Health with an emphasis on Health Behavior in the Joint Doctoral Program of Public Health at UC San Diego/San Diego State University, where the focus of her research is developing ways to use physical therapy as a tool to improve women’s and maternal health outcomes and address health disparities.
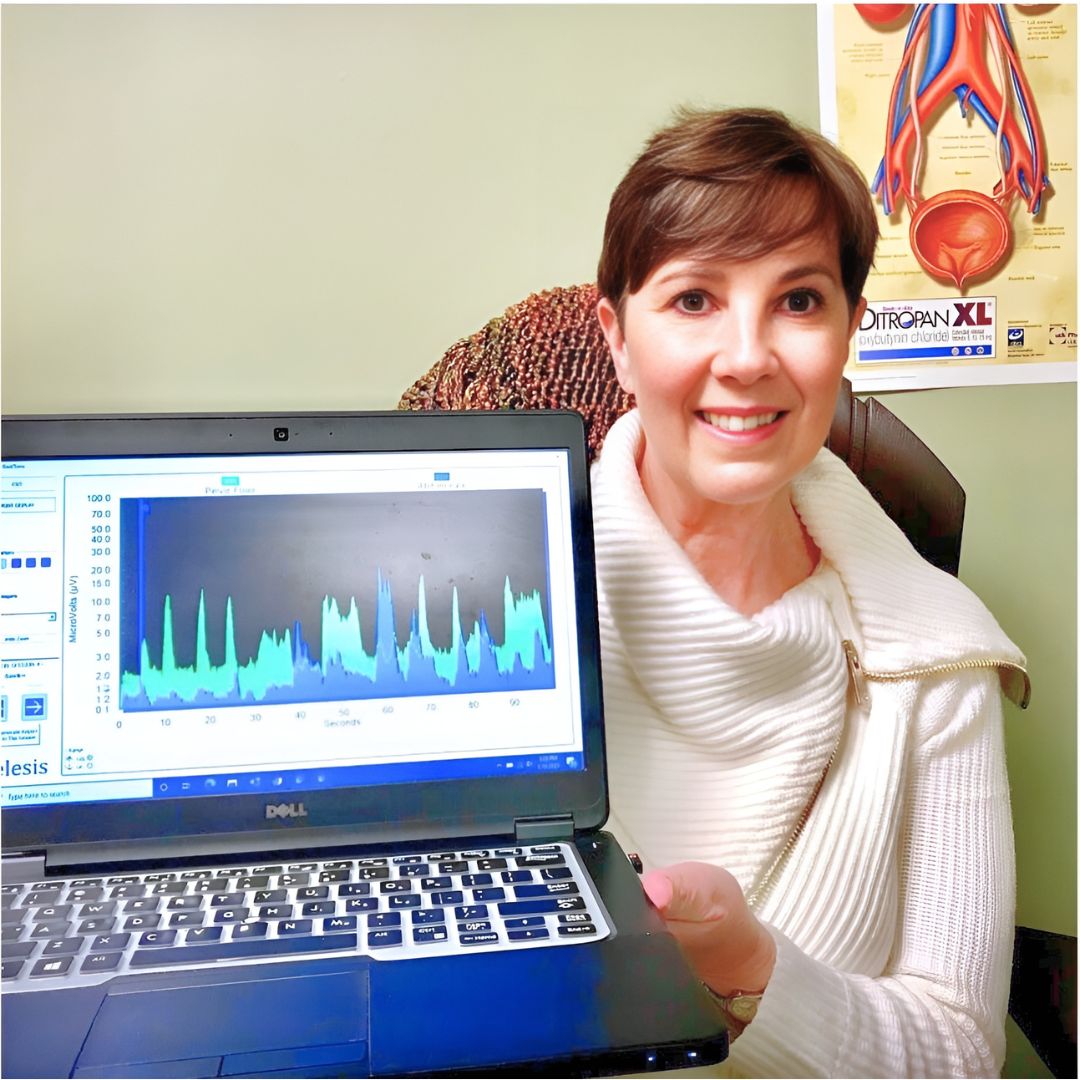
Surface EMG is the only modality that can isolate the active component of tone and is, therefore, a very valuable tool in the assessment of patients with altered tone conditions. However, it is the most misunderstood modality in pelvic health therapy. Rarely do practitioners see a topic so argued in pelvic rehabilitation as surface EMG biofeedback. Some practitioners boldly state they are for or against it on their social media accounts and clinic pages. Therapists are not questioning the use of biofeedback with neurologic or orthopedic applications, so why is it such a polarizing topic in pelvic health? The Pelvic Rehab Report sits down with faculty members Tiffany Lee and Jane Kaufman to discuss the tool they love. These two instructors have over 50 years of combined experience using biofeedback and have been teaching biofeedback board certification courses together for the past 16 years.
Biofeedback provides visual and auditory feedback of muscle activity and is a non-invasive technique that allows patients to adjust muscle function, strength, and behaviors to improve pelvic floor function. The small electrical signal (EMG) provides information about an unconscious process and is presented visually on a computer screen, giving the patient immediate knowledge of muscle function and enabling the patient to learn how to alter the physiological process through verbal and visual cues. Jane Kaufman explains “Many patients gain knowledge and awareness of the pelvic floor muscle through tactile feedback, but the visual representation helps patients hone in on body awareness and connect all the dots." Muscle evaluation through digital exam offers strength but does not appropriately address electrical activity such as resting tone and the ability to recruit or release tone in the muscle. The use of biofeedback addresses the specificity of muscle contraction and release, offering an additional view of muscle function.
In a 2020 research study by Pilkar et al., clinicians reported sEMG barriers of use, which included limited time and resources, clinically inapplicable sEMG system features, and the majority of clinicians' lack of training and/or confidence in the utilization of sEMG technology. This research also noted technical challenges, including the limited transfer of ever-evolving sEMG research into off-the-shelf EMG systems, nonuser-friendly intuitive interfaces, and the need for a multidisciplinary approach to accurately handling and interpreting data.
One barrier may be the price of a biofeedback unit. Tiffany Lee recommends using a 2-channel sEMG biofeedback hand-held unit with the software on a laptop or computer. In fact, to become board-certified in pelvic floor biofeedback, the Biofeedback Certification International Alliance (BCIA) requires a 2-channel EMG system with software. If you use a hand-held one-channel unit, the patient will have difficulty seeing the muscle activity and the coordination between the abdominals and pelvic floor. This prevents meaningful treatment as the patient cannot understand or interpret the LED bars on the machine (and often, the therapist cannot understand either). In truth, the benefits outweigh the cost of the equipment. You can cover the unit's cost and software to visualize muscle function and tone within a few treatments. Training is another issue; you need proper training in the modality to start utilizing biofeedback in your clinical setting. Most therapists have never been adequately trained. If they take a course where the instructor doesn’t believe in the benefits of biofeedback, they feel negatively toward a modality they have never personally explored. Biofeedback relies on a skilled clinician to interact with the patient, give verbal cues, ensure that the proper muscles are contracting and relaxing, and must be used in conjunction with their other skills and knowledge.
Think of sEMG biofeedback as one tool in your toolbox. Tiffany shares, "In a study by Aysun Ozlu MD et al., the authors conclude that biofeedback-assisted pelvic floor muscle training, in addition to a home exercise program, improves stress urinary incontinence rates more than a home exercise program alone." She continues, "Biofeedback is a powerful tool that can benefit your patient population and add to your skill set.
The acceptance of sEMG biofeedback in rehabilitation requires a unit (with software and sensors), training, and a multidisciplinary approach. Used correctly, it can positively impact patient performance and care in the clinic. Keep in mind that sEMG is a non-invasive technique. It has already shown great promise in neurorehabilitation and has been a widely utilized tool to assess neuromuscular outcomes in research. Jane Kaufman concludes, "Biofeedback treatment/training using the proper instrumentation provides the precise information necessary to change behaviors." This allows the patient to recognize that ‘yes, they are in charge of this muscle and that they can achieve success in overpowering the symptoms.’ Biofeedback routinely allows patients to understand that they are empowered to heal themselves with the tools you offer. They are in charge of their bodies and the outcome of treatment. It is also an important tool to use with patients who have experienced trauma and who are not ready to participate in manual therapy, and it is valuable for the pediatric population as well. Tiffany adds, “This modality can bring new business to your clinic. My local GI and colorectal providers often refer up to 5 new patients a week to my practice.
There is a long history of scientific evidence supporting the use of sEMG biofeedback in managing incontinence or pain symptoms. As a noninvasive, cost-effective, and powerful treatment modality, healthcare providers should consider this tool when managing pelvic floor dysfunction patients. Providers should be educated in the proper use of this valuable modality to gain the most out of the skills and knowledge that can be achieved through this intervention. For more information regarding courses and certification, please visit www.pelvicfloorbiofeedback.com.
Tiffany asked several PTs and OTs who have been to the board certification courses what they love about biofeedback. Here are a few answers
- “Biofeedback empowers my patients and gives them the confidence that they are actually doing their exercises and relaxing correctly! I’ve had nothing but positive feedback from patients, and it’s such a great tool to have as a pelvic floor therapist.”
- “My patients really love it, and they ask for it. I especially see the value for dyssynergia work on bearing down and learning eccentric abdominals and relaxed pelvic floor muscles. For men, I work on relaxing in standing and toileting postures if they can’t empty their bladder.”
- “Ultimately, the treatment needs to be meaningful to the patient. Biofeedback can complement other treatments. Their needs come before ours. We should offer all of our patients the ability to control their own muscles and SEE how to do it.”
- “After ONE session with a 5-year-old with constipation, mom called me in sheer excitement, screaming over the phone that he pooped on the potty!!! Something he has NEVER done before. Biofeedback helped him find and coordinate the potty muscles and tummy muscles, and this made a huge difference for him!”
- “Becoming certified in biofeedback has only been positive for me. My patients feel that the initial sEMG evaluation sets the stage for my care plan, and my discharge reassessment is a tangible reflection of their progress. Not to mention its strength as a marketing tool.”
Jane Kaufman adds “Biofeedback in treatment has been a game changer. Using this tool as a foundation for treatment in my clinic allowed my practice to grow, thrive, and achieve great acclaim in our region and beyond. It is not unusual for patients to travel several hours to seek treatment because of the empowering effect the biofeedback visual had on their understanding of their dysfunction.”
Biofeedback for Pelvic Floor Muscle Dysfunction is scheduled for July 28th and December 7th, 2024, and provides a safe space for clinicians to learn and practice this valuable tool. Registrants will need equipment to participate in this online course and will learn about the benefits of using this modality in their clinical practice.
In this course, Tiffany and Jane guide participants through learning to administer biofeedback assessments, analyze and interpret sEMG signals, conduct treatment sessions, and role-play patient instruction/education for each diagnosis presented during the many hands-on lab experiences.
References:
- Use of Surface EMG in Clinical Rehabilitation of Individuals With SCI: Barriers and Future Considerations Rakesh Pilkar, Kamyar Momeni, Arvind Ramanujam, Manikandan Ravi, Erica Garbarini, Gail F. Forrest. Front Neurol. 2020; 11: 578559. Published online 2020 Dec 18. doi: 10.3389/fneur.2020.578559 PMCID: PMC7780850
- Comparison of the efficacy of perineal and intravaginal biofeedback-assisted pelvic floor muscle exercises in women with urodynamic stress urinary incontinence. Aysun Ozlu MD, Neemettin Yildiz MD, Ozer Oztekin MD. Neurourol Urodyn. 2017 Nov;36(8):2132-2141. Epub 2017 Mar 27. doi: 10.1002/nau.23257 PMID: 28345778.
- Cram, J. R., & Kasman, G. S. (2011). The basics of surface electromyography. In E. Criswell (Ed.). Cram’s introduction to surface electromyography (2nd ed., pp. 3–7.) Jones and Bartlett.
- Kaufman, J., Stanton, K., & Lee, T. E. (2021). Pelvic Floor Biofeedback for the Treatment of Urinary Incontinence and Fecal Incontinence. Biofeedback, 49(3), 71-76.
- Shelly, Beth & Kaufman, Jane (2023). Foundations of Pelvic Floor Muscle Assessment Using Surface Electromyography. APTA Academy of Pelvic Health Physical Therapy.
AUTHOR BIOS
Tiffany Lee, OTR, OTD, MA, BCB-PMD, PRPC

Tiffany Lee holds a BS in OT from UTMB Galveston (1996), an MA in Health Services Management, and a post-professional OTD from Texas Tech University Health Sciences Center. In 2004, she received her board certification in Pelvic Muscle Dysfunction from the Biofeedback Certification International Alliance. She is a Herman & Wallace Pelvic Rehab Institute faculty member and teaches biofeedback courses. She has been treating pelvic health patients for 25 out of her 30-year career. Her private practice in San Marcos, Texas, is exclusively dedicated to treating urinary and fecal incontinence and pelvic floor disorders. Her continuing education company, Biofeedback Training & Incontinence Solutions, offers clinical consultation and training workshops. She also enjoys mentoring healthcare professionals working toward their BCIA certification.
Jane Kaufman, PT, M.Ed, BCB-PMD
Jane has been practicing PT for more than fifty years. She is a graduate of the Ithaca College Physical Therapy program and earned her master’s degree at the University of Vermont. In her early career, she practiced in outpatient settings, skilled nursing, and acute rehabilitation. Jane’s career began at Columbia Presbyterian Medical Center and progressed to the University of Vermont Health Network where she supervised the Department of Physical Therapy’s outpatient services. In the late 1990s, Jane became intrigued with pelvic floor muscle dysfunction, evolving to a quarter-century career in this highly specialized field.
In 2001 she began her career as a sole practitioner in pelvic floor muscle dysfunction and in 2003 established Phoenix Physical Therapy, PLC with a staff of clinicians specializing in the treatment of pelvic floor dysfunction, incontinence, and pelvic pain for all genders and all ages. In 2005, Jane became certified in the use of surface EMG biofeedback for pelvic floor muscle dysfunction (BCB-PMD ) from the Biofeedback Certification International Alliance. She sold her practice in 2022, having established a renowned reputation in Vermont, upstate New York, regionally, nationally, and internationally. Post Phoenix, Jane continues to offer workshops for other healthcare providers in the use of biofeedback for pelvic muscle dysfunction, and mentors healthcare professionals around the world toward certification in this field through the Biofeedback Certification International Alliance. Jane teams with Tiffany Lee, OTR, OTD through Biofeedback Training and Incontinence Solutions (www.pelvicfloorbiofeedback.com).
Jane has recently begun a consulting practice helping adults with pelvic floor muscle dysfunction issues and has continued helping children/teens through her new practice, PottyTime Physical Therapy (www.pottytimephysicaltherapy.com). In addition to her practice and teaching, Jane has participated in research through the University of Vermont Health Network on pelvic organ prolapse, incontinence, and sexual dysfunction. She has authored an article published in the online international journal Biofeedback and was a co-author in the APTA self-study manual for Foundations in Pelvic Floor Muscle Assessment using Surface Electromyography with Dr. Beth Shelley, PT, DPT, WCS, BCB-PMD. She is a Herman & Wallace Pelvic Rehabilitation Institute faculty member and teaches biofeedback courses through this company. Jane may be reached by email at: jkaufmanpt@comcast.net

Did you know that chronic pain affects an estimated 51.6 million adults in the United States alone? That's almost 21% of the population (1). It's a debilitating condition that can disrupt daily life and limit one's ability to function. But what about those with hypermobility? Often individuals with hypermobility are even more susceptible to chronic pain and their treatment may require a unique approach.
There are many variables that make a person more susceptible to developing chronic pain. Some of these include genetics, prior trauma, culture, and health history. Patients with hypermobility are more likely to develop chronic pain and may also need to be treated with a different lens than the rest of the population.
What is Hypermobility
Hypermobility spectrum disorder (HSD) includes joint hypermobility syndrome (JHS) as one of its conditions and is a connective tissue disorder characterized by chronic musculoskeletal pain due to joint hyperextensibility and is a common cause of chronic pain, fatigue, headaches, anxiety, orthostasis, and abdominal pain. Hypermobility spectrum disorder (HSD) is sometimes considered a milder variant of hypermobile EDS (hEDS) and is seen in up to 3% of the general population, with a prevalence rivaling fibromyalgia, gout, and rheumatoid arthritis (2).
Joint hypermobility implies a range of motion of a joint that exceeds the documented “norm.” Norms for each joint are determined by the specific joint anatomy, the person’s age, sex, and ethnicity. Hypermobility is typically scored using the Beighton scale requiring at least a 5 to be classified as systemically hypermobile. The Beighton score is determined by 9 points awarded for each described condition met. The conditions include (3,4):
- Elbow hyperextension of at least 10 degrees (one for each elbow)
- Knee hyperextension of at least 10 degrees (one for each knee)
- Ability to passively extend the pinky finger to 90 degrees or more (one for each hand)
- Ability to touch the thumb to the forearm with wrist flexion (one for each hand)
- Ability to forward flex the trunk at the hips and place both palms on the floor with knees extended.

Hypermobility as a problematic condition occurs on a spectrum and ranges from Hypermobility Spectrum Disorder (HSD) to genetic connective tissue disorders such as hypermobile EDS (hEDS). Patients with connective tissue disorders often have other symptoms associated with the syndrome such as fragile blood vessels or cardiac arrhythmias (3). Those with generalized joint hypermobility are less likely to have other associated comorbidities.
Hypermobility and Rehab
A patient with hypermobility must have their hypermobility considered in their treatment plan as their tissues, and force tolerance of tissues, differ from the rest of the population. Patients with hypermobility may present with decreased strength overall and require more strength than typical to perform activities. This is likely due to the extensibility of the tendons and ligaments, changing the force a muscle can produce. Patients with hypermobility also often have decreased proprioception, as their tissue laxity cannot provide as much awareness to the brain. These variables can lead to a higher incidence of injury, with dislocation common for those with hEDS (4).
Hypermobility is also correlated with pelvic pain and dysfunction, especially in female patients. They are more prone to pelvic organ prolapse but also may present with pelvic floor muscle overactivity (3) creating a difficult case to treat, especially if they have chronic pain in addition. This patient will often benefit from rehabilitation to address the prolapse, muscle overactivity, and then coordination of core and pelvic stabilizers. Knowing that the patient has hypermobility can be vital to the successful treatment plan for this presentation. When treating patients with hypermobility, they often have decreased functional tolerances for loading, not only at the joints but also systemically. hEDS especially, is highly associated with autonomic dysfunction such as postural orthostatic tachycardia syndrome (POTS), which may affect your treatment plan as well. A portable pulse oximeter and slow positional changes may be helpful in decreasing and monitoring symptoms (3,4).
 Pain Patterns and Hypermobility (3)
Pain Patterns and Hypermobility (3)
Pain patterns for the hypermobile patient include all 3 subtypes of pain.
- Nociceptive Acute Pain
- Neuropathic Pain
- Nociplastic Pain
Nociceptive acute pain will occur at localized injury sites with frequent dislocations, strains, and sprains. These recurrent injuries can then lead to chronic musculoskeletal changes of the joint that affect function and gait.
Neuropathic pain can also become problematic for this population. Due to the increased laxity of their vertebrae, they may suffer from higher incidences of spinal cord compression and peripheral nerve compression. It is also becoming more common to evaluate this population with a dermal biopsy for small fiber neuropathy. As the patient experiences continued nociceptive and neuropathic pain inputs over and over, their nervous system may also sensitize causing both peripheral and central sensitization with nociplastic pain.
Nociplastic pain may then transform into widespread generalized pain. As their pain patterns progress, they may start to experience more fear avoidance behaviors and may become deconditioned. Deconditioning in turn can lead to more injuries and continues a recurrent cycle for these patients.
Conclusion
Knowing that patients with hypermobility are more susceptible to chronic pain allows us to treat this population more effectively. As rehab practitioners, we can educate the patient, improve strength, improve stability, improve proprioception, and work to desensitize the nervous system. A sensitive nervous system may be the initial hurdle with the hypermobile patient.
Pain neuroscience education is the first step to educate the patient on how their nervous system functions and to decrease fear they may have around pain. After education, there are several physical interventions we can use for the nervous system including dry needling, spinal mobilization, manual therapy, and exercise.
Ready to Learn More?
Expand your knowledge, experience, and treatment in understanding and applying pain science to the chronic pelvic pain population with Alyson Lowrey and Tara Sullivan in their upcoming course Pain Science for the Chronic Pelvic Pain Population on August 17-18, 2024.
This course is not specific to the patient who is hypermobile. However, there are portions of the course that address this population. This course provides a thorough introduction to pain science concepts including classifications of pain mechanisms, peripheral pain generators, peripheral sensitization, and central sensitization in listed chronic pelvic pain conditions; as well as treatment strategies including therapeutic pain neuroscience education, therapeutic alliance, and the current rehab interventions' influence on central sensitization.
Pain Science for the Chronic Pelvic Pain Population is a remote course that will provide you with the understanding and tools needed to identify and treat patients with chronic pelvic pain from a pain science perspective. Lecture topics include the history of pain, pain physiology, central and peripheral sensitization, sensitization in chronic pelvic pain conditions, therapeutic alliance, pain science and trauma-informed care, therapeutic pain neuroscience education, the influence of rehab interventions on the CNS, and specific case examples for sensitization in CPP.
References:
- Rikard, S. Michaela, et al. “Chronic pain among adults — United States, 2019–2021.” Morbidity and Mortality Weekly Report, vol. 72, no. 15, 14 Apr. 2023, pp. 379–385, DOI: https://doi.org/10.15585/mmwr.mm7215a1.
- Kumar, Bharat, and Petar Lenert. “Joint hypermobility syndrome: Recognizing a commonly overlooked cause of chronic pain.” The American Journal of Medicine, vol. 130, no. 6, June 2017, pp. 640–647, DOI: https://doi.org/10.1016/j.amjmed.2017.02.013.
- Syx D, De Wandele I, Rombaut L, Malfait F. Hypermobility, the Ehlers-Danlos syndromes and chronic pain. PubMed. 2017;35 Suppl 107(5):116-122.
- Scheper M, De Vries JE, Verbunt J, Engelbert RHH. Chronic pain in hypermobility syndrome and Ehlers-Danlos syndrome (hypermobility type): it is a challenge. Journal of Pain Research. August 1, 2015:591-601
AUTHOR BIO
Alyson Lowrey, PT, DPT, OCS
Dr. Lowrey attended the University of New Mexico where she received a BA degree in Psychology in 2011. She then attended the University of New Mexico School of Medicine to earn her Doctor of Physical Therapy degree in 2014. Following graduation from UNM, Alyson completed the HonorHealth Orthopaedic Residency program in 2015 and became a board-certified orthopedic specialist (OCS) in 2016. She is now the director of that residency program and lectures about pain and pelvic dysfunction in the curriculum. Alyson treats the pelvic floor patient population through an orthopedic approach, working closely with pelvic floor specialists. This allows for a wholistic style addressing the entire patient from a functional perspective. Alyson’s clinical interests include the evaluation and treatment of chronic pain, lumbar and cervical spine disorders, foot and ankle disorders, pelvic pain, and clinical instruction. She is certified in dry needling and an APTA-certified clinical instructor, regularly taking students from several PT schools. She participates in Creighton’s and Midwestern University’s Doctor of Physical Therapy programs as adjunct faculty assisting in lab and lecturing in Biomechanics, Kinesiology, and Musculoskeletal courses. Outside of the clinic, she enjoys being active, doing yoga, crafting, and spending time with her husband and cats.

Most of us spend our day sitting and do not think about the position of our ilia, sacrum, or coccyx during the change from standing to sitting. Weight-bearing through a tripod of bilateral ischial tuberosities and a sacrum that should have normalized form closure should be easy and pain-free.
The coccyx typically has minimal weight bearing in sitting, about 10%, just like the fibula, however, it can be a major pain generator, if the biomechanics of the ilia, sacrum, and femoral head positions are not quite right. A lot of patients will state “My pain is worse with sitting” which can mean thoracic pain, low back/sacral pain, and even lower extremity radicular pain.
Scanning the literature for coccyx treatment does not always yield the best results for physical or occupational therapists. Most literature states what the medical interventions can be, and physical therapy is never at the forefront. However, as we are musculoskeletal and neuromuscular specialists, this is no different in our thinking patterns relating to coccyx pain or painful sitting.
During sitting, the coccyx has normal flexion and extension moments that will change or become dysfunctional once mechanics above and below that joint change. A simple ankle sprain from 2 years ago can result in chronic knee and sacroiliac pain that can lead to coccyx pain over time. Even the patient who has long-standing TMJ (temporomandibular joint) and cervical dysfunction, now has a thoracic rotation and your correction of their coccyx deviation cannot maintain correction.
Coccydynia and Painful Sitting is a course that provides a spark for your orthopedic mindset and encourages clinicians to evaluate the coccyx more holistically.
- What are the joints doing?
- How does it change from sitting to standing?
- Standing to sitting?
- What is the difference from sitting upright to slump activities?
Working through the basics and the obvious with failed results takes you to the next step of critical thinking within this course. How does the patient present? What seems to be lacking and how to correct them biomechanically to achieve pain-free sitting? Related coccyx musculature and nerve dysfunction can seem like the easiest to treat, but what happens when those techniques fail?
In Coccydynia and Painful Sitting, we look at the entire body, from the cranium to the feet, to determine the driver of coccyx pain and dysfunction. A better understanding of ilial motion, with accompanied spring tests (Hesch Method) normalizing spinal mechanics and lower extremity function is highlighted in this course. Internal vaginal and rectal release of pelvic floor muscles can lead to normalized coccyx muscle tension that is supported via coccyx taping.
To learn more, join Lila Abatte in her next Coccydynia remote course scheduled for July 13, 2024.
AUTHOR BIO
Lila Abbate, PT, DPT, OCS, WCS, PRPC

Lila Abbate, PT, DPT, MS, OCS, WCS, PRPC is the Director/Owner of New Dimensions Physical Therapy with locations in Roslyn, Long Island, and the Noho Section of New York City. Dr. Abbate graduated from Touro College in Dix Hills, NY with a Bachelor of Science (BS) in Health Sciences and a Master of Arts (MA) in Physical Therapy in 1997. She completed her Advanced Masters in Manual Orthopedic Physical Therapy (MS) at Touro College, Bayshore, NY in 2003 and continued to pursue her Doctor of Physical Therapy (DPT) at Touro in 2005. Dr. Abbate is a Board-Certified Specialist by the American Physical Therapy Association in Orthopedics (OCS) 2004 and Women’s Health (WCS) 2011. She obtained the Certified Pelvic Rehabilitation Practitioner (PRPC) from the Herman & Wallace Institute in 2014. She is a Diane Lee/LJ Lee, Integrated Systems Model (ISM) graduate and completed the New York series in 2012.
Dr. Abbate has been an educator for most of her physical therapy career. She has experience as a full-time faculty at Touro College, Manhattan Campus from 2002 to 2006 teaching the biomechanical approach to orthopedic dysfunction and therapeutic exercise as well as massage/soft tissue work that highlighted trigger point work, scar management, and myofascial release.
She is currently on faculty as a Lecturer at Columbia University teaching the private practice section Business & Management course (since 2016) along with the Pelvic Health elective (since 2012). She teaches nationally and internationally with the Herman & Wallace Pelvic Rehabilitation Institute teaching advanced courses of her own intellectual property: Orthopedic Assessment for the Pelvic Health Therapist, Bowel Pathology Function, Dysfunction and the Pelvic Floor, Coccydynia & Painful Sitting: Orthopedic Implications. She was a co-writer for the Pudendal Neuralgia course and teaches the Pelvic Function Series and the Pregnancy and Postpartum Rehabilitation courses. She has written two book chapters in 2016: Pelvic Pain Management by Valvoska and Healing in Urology: Clinical Guidebook to Herbal and Alternative Therapies by Chughtai.
She is a member of the American Physical Therapy Association, the National Vulvodynia Association, the American Urogynecology Association, and the International Pelvic Pain Society. Dr. Abbate is also a Senior Physical Therapy consultant for SI Bone, a sacroiliac joint instrumentation company.
By accepting you will be accessing a service provided by a third-party external to https://www.hermanwallace.com/









































