Herman & Wallace are pleased to announce a new course! Pudendal Neuralgia and Nerve Entrapment will be presented by Michelle Lyons in Freehold, NJ on June 17/18, 2017. We chatted with Michelle about this new course to hear her thoughts and get an overview of the contents
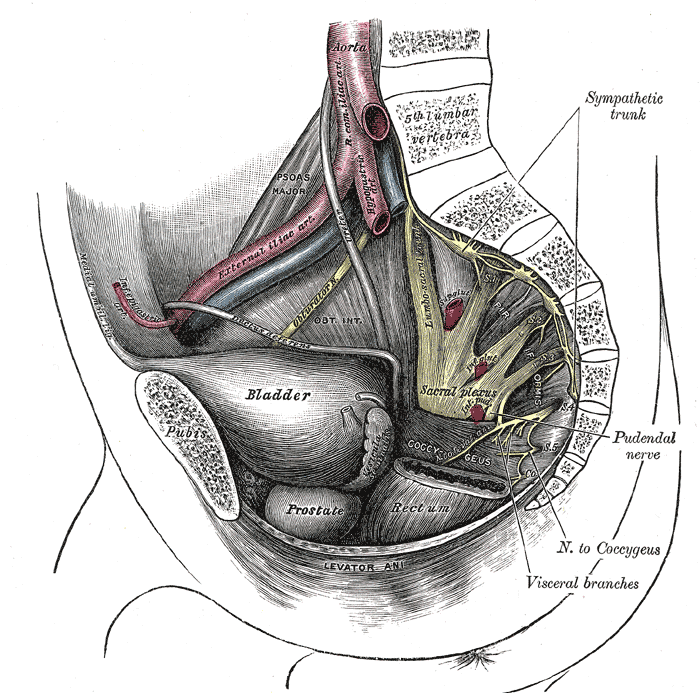 There are a number of courses which I teach for Herman & Wallace including Pelvic Floor Level 2A, my Male Oncology and Female Oncology and the The Athlete and the Pelvic Floor courses. They all have sections on pudendal dysfunction and it’s an area that participants always want more information on. There’s no other nerve that elicits the same interest, discussion and confusion! Nobody really talks about iliohypogastric or ulnar neuralgia with the same intensity as pudendal neuralgia, and no other nerve dysfunction provokes the same amount of controversy and mystery.
There are a number of courses which I teach for Herman & Wallace including Pelvic Floor Level 2A, my Male Oncology and Female Oncology and the The Athlete and the Pelvic Floor courses. They all have sections on pudendal dysfunction and it’s an area that participants always want more information on. There’s no other nerve that elicits the same interest, discussion and confusion! Nobody really talks about iliohypogastric or ulnar neuralgia with the same intensity as pudendal neuralgia, and no other nerve dysfunction provokes the same amount of controversy and mystery.
When I was approached about developing this course for the Institute, I jumped at the opportunity. For those who don’t know me, I really like to bring an integrative approach to my work, both clinically and educationally. I have experience and training in nutrition, coaching, yoga, Pilates and mindfulness as a therapeutic intervention and I think these fit really well alongside traditional pelvic rehab approaches. Manual therapy and bespoke exercise prescription will always be the bedrock of my approach, but sometimes our patients, especially those with chronic pain, need some extra support. I’m also a bit of an anatomy nerd, so the chance to delve deep into pelvic neuroanatomy and neurodynamics was too much to resist!
I think this is a Golden Age in pelvic health – there are so many great learning opportunities and resources available to us to help serve our patients better. Another area that I find fascinating to explore is the huge leap we have made in understanding neuroscience and the role of pain education when it comes to chronic pelvic pain. I’m a big fan of the work done by Moseley and Butler in Australia, and I love how authors like Hilton, Vandyken and Louw have transferred that to the world of pelvic pain in their book "Why Pelvic Pain Hurts". The language that we use is very important when discussing how the brain responds to chronic pain and the changes that occur with central sensitization. We never want our patients to feel as if we think their pain is ‘all in their heads’ but at the same time, we need to be able to incorporate strategies such as motor imagery and graded exposure and to demonstrate to our patients that"…it is important to acknowledge that chronic pain need not involve any structural pathology" (Aronoff 2016).
Those are some of the discussions we’ll be having in Freehold, NJ next June – I hope you’ll come and join the conversation!
"What Do We Know About the Pathophysiology of Chronic Pain? Implications for Treatment Considerations" Aronoff, GM Med Clin North Am. 2016 Jan;100(1):31-42
"Why Pelvic Pain Hurts: Neuroscience Education for Patients with Pelvic Pain" Hilton, Vandyken, Louw, International Spine and Pain Institute (May 28, 2014)
When I bring up the topic of pelvic floor dysfunction in athletes, stress urinary incontinence (SUI) is usually the first aspect of pelvic health that springs to mind – and rightly so, as professional sport is one of the risk factors for stress urinary incontinence Poswiata et al 2014. The majority of studies show that the average prevalence of urinary incontinence across all sports is 50%, with SUI being the most common lower urinary tract symptom. Athletes are constantly subject to repeated sudden & considerable rises in intra-abdominal pressure: e.g. heel striking, jumping, landing, dismounting and racquet loading.
What’s less often discussed is the topic of gastrointestinal dysfunction in athletes. Anal incontinence in athletes is not well documented, although a study from Vitton et al in 2011 found a higher prevalence than in age matched controls (conversely a study by Bo & Braekken in 2007 found no incidence). More recently, Nygaard reported earlier this year (2016) that young women participating in high-intensity activity are more likely to report anal incontinence than less active women.
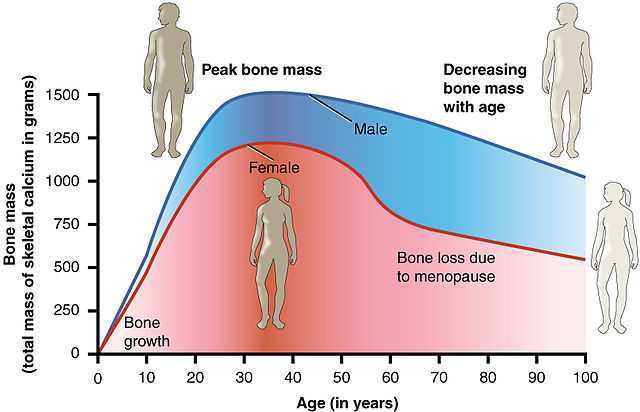
A presentation by Colleen Fitzgerald, MD at the American Urogynecologic Society meeting in 2014 highlighted the multifaceted nature of pelvic floor dysfunction in female athletes, specifically in this case, triathletes. The study found that one in three female triathletes suffers from a pelvic floor disorder such as urinary incontinence, bowel incontinence and pelvic organ prolapse. One in four had one component of the "female athlete triad", a condition characterized by decreased energy, menstrual irregularities and abnormal bone density from excessive exercise and inadequate nutrition. Researchers surveyed 311 women for this study with a median age range of 35 – 44. These women were involved with triathlete groups and most (82 percent) were training for a triathlon at the time of the survey. On average, survey participants ran 3.7 days a week, biked 2.9 days a week and swam 2.4 days a week.
Of those who reported pelvic floor disorder symptoms, 16% had urgency urinary incontinence, 37.4% had stress urinary incontinence, 28% had bowel incontinence and 5% had pelvic organ prolapse. Training mileage and intensity were not associated with pelvic floor disorder symptoms. 22% of those surveyed screened positive for disordered eating, 24% had menstrual irregularities and 29% demonstrated abnormal bone strength. With direct access becoming a reality for many of us, we must acknowledge the need for specific questioning when it comes to pelvic health issues, as well as the ability to recognise signs and symptoms of the female athlete triad in our patients.
Want to learn more about pelvic health for athletes? Join me in beautiful Arlington this November 5-6 at The Athlete and the Pelvic Floor!
J Hum Kinet. 2014 Dec 9; 44: 91–96 Published online 2014 Dec 30. doi:10.2478/hukin-2014-0114 PMCID: PMC4327384. Prevalence of Stress Urinary Incontinence in Elite Female Endurance Athlete Anna Poświata, Teresa Socha and Józef Opara1
J Womens Health (Larchmt). 2011 May;20(5):757-63. doi: 10.1089/jwh.2010.2454. Epub 2011 Apr 18. Impact of high-level sport practice on anal incontinence in a healthy young female population. Vitton V, Baumstarck-Barrau K, Brardjanian S, Caballe I, Bouvier M, Grimaud JC.
Am J Obstet Gynecol. 2016 Feb;214(2):164-71. doi: 10.1016/j.ajog.2015.08.067. Epub 2015 Sep 6. Physical activity and the pelvic floor. Nygaard IE, Shaw JM.
After menopause, more than half of women may have vulvovaginal symptoms that can impact their lifestyle, emotional well-being and sexual health. What's more, the symptoms tend to co-exist with issues such as prolapse, urinary and/or bowel problems. But unfortunately many women aren't getting the help they need, despite a growing body of evidence that skilled pelvic rehab interventions are effective in the management of bladder/bowel dysfunctions, POP, sexual health issues and pelvic pain.
 Vaginal dryness, hot flashes, night sweats, disrupted sleep, and weight gain have been listed as the top five symptoms experienced by postmenopausal women in North America and Europe, according to a study by Minkin et al 2015, and they also concluded ‘The impact of postmenopausal symptoms on relationships is greater in women from countries where symptoms are more prevalent.’
Vaginal dryness, hot flashes, night sweats, disrupted sleep, and weight gain have been listed as the top five symptoms experienced by postmenopausal women in North America and Europe, according to a study by Minkin et al 2015, and they also concluded ‘The impact of postmenopausal symptoms on relationships is greater in women from countries where symptoms are more prevalent.’
Between 17% and 45% of postmenopausal women say they find sex painful, a condition referred to medically as dyspareunia. Vaginal thinning and dryness are the most common cause of dyspareunia in women over age 50. However pain during sex can also result from vulvodynia (chronic pain in the vulva, or external genitals) and a number of other causes not specifically associated with menopause or aging, particularly orthopaedic dysfunction, which the pelvic physical therapist is in an ideal position to screen for.
According to the North America Menopause Society, ‘…beyond the immediate effects of the pain itself, pain during sex (or simply fear or anticipation of pain during sex) can trigger performance anxiety or future arousal problems in some women. Worry over whether pain will come back can diminish lubrication or cause involuntary—and painful—tightening of the vaginal muscles, called vaginismus. The result can be a vicious circle, again highlighting how intertwined sexual problems can become.’
The research has demonstrated that the optimal strategy for post-menopausal stress incontinence is a combination of local hormonal treatment and pelvic floor muscle training – the strategy of combining the two approaches has been shown to be superior to either approach used individually (Castellani et al 2015, Capobianco et al 2012) and similar conclusions can be drawn for promoting sexual health peri- and post-menopausally.
The pelvic rehab specialist may be called upon to screen for orthopaedic dysfunction in the spine, hips or pelvis, to discuss sexual ergonomics such as positioning or the use of lubricant as well as providing information and education about sexual health before, during and after menopause.
To learn more about sexual health and pelvic floor function/dysfunction at menopause, join me in Atlanta in March for Menopause: A Rehab Approach!
Prevalence of postmenopausal symptoms in North America and Europe, Minkin, Mary Jane MD, NCMP1; Reiter, Suzanne RNC, NP, MM, MSN2; Maamari, Ricardo MD, NCMP3, Menopause:November 2015 - Volume 22 - Issue 11 - p 1231–1238
Low-Dose Intravaginal Estriol and Pelvic Floor Rehabilitation in Post-Menopausal Stress Urinary Incontinence, Castellani D. · Saldutto P. · Galica V. · Pace G. · Biferi D. · Paradiso Galatioto G. · Vicentini C., Urol Int 2015;95:417-421
After menopause, more than half of women may have vulvovaginal symptoms that can impact their lifestyle, emotional well being and sexual health. What's more, the symptoms tend to co-exist with issues such as prolapse, urinary and/or bowel problems. But unfortunately many women aren't getting the help they need, despite a growing body of evidence that skilled pelvic rehab interventions are effective in the management of bladder/bowel dysfunctions, POP, sexual health issues and pelvic pain.
 Vaginal dryness, hot flashes, night sweats, disrupted sleep, and weight gain have been listed as the top five symptoms experienced by postmenopausal women in North America and Europe, according to a study by Minkin et al 2015, and they also concluded ‘The impact of postmenopausal symptoms on relationships is greater in women from countries where symptoms are more prevalent.’ Between 17% and 45% of postmenopausal women say they find sex painful, a condition referred to medically as dyspareunia. Vaginal thinning and dryness are the most common cause of dyspareunia in women over age 50. However pain during sex can also result from vulvodynia (chronic pain in the vulva, or external genitals) and a number of other causes not specifically associated with menopause or aging, particularly orthopaedic dysfunction, which the pelvic physical therapist is in an ideal position to screen for.
Vaginal dryness, hot flashes, night sweats, disrupted sleep, and weight gain have been listed as the top five symptoms experienced by postmenopausal women in North America and Europe, according to a study by Minkin et al 2015, and they also concluded ‘The impact of postmenopausal symptoms on relationships is greater in women from countries where symptoms are more prevalent.’ Between 17% and 45% of postmenopausal women say they find sex painful, a condition referred to medically as dyspareunia. Vaginal thinning and dryness are the most common cause of dyspareunia in women over age 50. However pain during sex can also result from vulvodynia (chronic pain in the vulva, or external genitals) and a number of other causes not specifically associated with menopause or aging, particularly orthopaedic dysfunction, which the pelvic physical therapist is in an ideal position to screen for.
According to the North America Menopause Society, ‘…beyond the immediate effects of the pain itself, pain during sex (or simply fear or anticipation of pain during sex) can trigger performance anxiety or future arousal problems in some women. Worry over whether pain will come back can diminish lubrication or cause involuntary—and painful—tightening of the vaginal muscles, called vaginismus. The result can be a vicious circle, again highlighting how intertwined sexual problems can become.’
The research has demonstrated that the optimal strategy for post-menopausal stress incontinence is a combination of local hormonal treatment and pelvic floor muscle training – the strategy of combining the two approaches has been shown to be superior to either approach used individually (Castellani et al 2015, Capobianco et al 2012) and similar conclusions can be drawn for promoting sexual health peri- and post-menopausally.
The pelvic rehab specialist may be called upon to screen for orthopaedic dysfunction in the spine, hips or pelvis, to discuss sexual ergonomics such as positioning or the use of lubricant as well as providing information and education about sexual health before, during and after menopause.
To learn more about sexual health and pelvic floor function/dysfunction at menopause, join me in Atlanta in March for Menopause: A Rehab Approach.
Prevalence of postmenopausal symptoms in North America and Europe, Minkin, Mary Jane MD, NCMP1; Reiter, Suzanne RNC, NP, MM, MSN2; Maamari, Ricardo MD, NCMP3, Menopause:November 2015 - Volume 22 - Issue 11 - p 1231–1238
Low-Dose Intravaginal Estriol and Pelvic Floor Rehabilitation in Post-Menopausal Stress Urinary Incontinence, Castellani D. · Saldutto P. · Galica V. · Pace G. · Biferi D. · Paradiso Galatioto G. · Vicentini C., Urol Int 2015;95:417-421
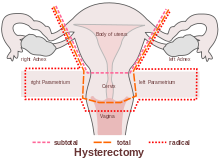
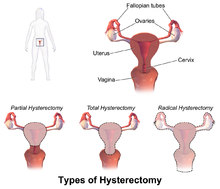 ACOG (American College of Obstetrics and Gynecology) describes hysterectomy as a treatment of last resort, but studies show that anywhere from 10 to 90% of hysterectomies performed in the United States are not medically necessary, evidenced by the fact that today, approximately 90 percent of hysterectomies are performed electively. Corona et al stated: ‘…that alternatives to hysterectomy are underutilized in women undergoing hysterectomy for AUB, uterine fibroids, endometriosis, or pelvic pain. The rate of unsupportive pathology when hysterectomies were done for these indications was 18%.’
ACOG (American College of Obstetrics and Gynecology) describes hysterectomy as a treatment of last resort, but studies show that anywhere from 10 to 90% of hysterectomies performed in the United States are not medically necessary, evidenced by the fact that today, approximately 90 percent of hysterectomies are performed electively. Corona et al stated: ‘…that alternatives to hysterectomy are underutilized in women undergoing hysterectomy for AUB, uterine fibroids, endometriosis, or pelvic pain. The rate of unsupportive pathology when hysterectomies were done for these indications was 18%.’
The US has the highest rate of hysterectomy in the industrialized world; it is the second most common surgical procedure carried out on women. 1 in 3 American women have their uterus removed by the age of 60, with the highest rates in women aged 30-54 (according to Corona et al in 2014, one in five women may not need it).
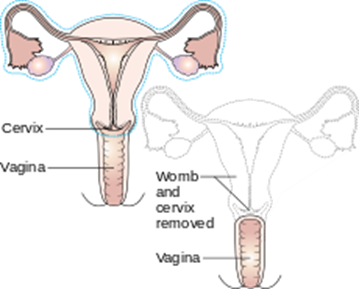 Reasons for hysterectomy include cancer, bleeding with childbirth and severe infection with uterine damage, all of which make up about 10% of cases. The other 90% are made up of medical, non-surgical and other surgical reasons, such as for menstrual cramps, heavy bleeding and fibroids. Unfortunately, too many women are also having hysterectomies as a treatment option for endometriosis (instead of laparoscopic excision, histological confirmation and pelvic rehab follow up)
Reasons for hysterectomy include cancer, bleeding with childbirth and severe infection with uterine damage, all of which make up about 10% of cases. The other 90% are made up of medical, non-surgical and other surgical reasons, such as for menstrual cramps, heavy bleeding and fibroids. Unfortunately, too many women are also having hysterectomies as a treatment option for endometriosis (instead of laparoscopic excision, histological confirmation and pelvic rehab follow up)
Numerous women who undergo hysterectomy remain unclear about the details of their surgical procedures or indeed the implication for short and long term recovery. Clinically, I have seen many women who assume that as they have had a ‘Total’ Hysterectomy, that includes removal of their ovaries (Total vs Partial Hysterectomy generally refers to cervical preservation). I have also see many women confused as to why their recovery from what has been a laparoscopic surgery, with small incisions, is taking so long. A surgical colleague described it well in my opinion: ‘A laparoscopic hysterectomy is major abdominal/pelvic surgery with tiny incisions’.
 In Part Two of this blog, I will discuss the sequelae of hysterectomy and the key role of pelvic rehab. Interested in learning more about Endometriosis, Fertility and Hysterectomy? Join me in Denver in January!
In Part Two of this blog, I will discuss the sequelae of hysterectomy and the key role of pelvic rehab. Interested in learning more about Endometriosis, Fertility and Hysterectomy? Join me in Denver in January!
The Boston Women's Health Book Collective. Our Bodies, Ourselves: A New Edition For A New Era. New York: Touchstone, 2005., Centers for Disease Control and Prevention Online. "Hysterectomy Surveillance" --- United States, 1994,1999, 2002. http://www.cdc.gov/mmwr/preview/mmwrhtml/ss5105a1.htm
‘Use of other treatments before hysterectomy for benign conditions in a statewide hospital collaborative’ Corona et al (Presented in oral and poster format at the 4oth Annual Scientific Meeting of the Society of Gynecologic Surgeons, Scottsdale March 24-26 2014)
The abdominal canister is a model that we have used in rehab for a number of years, especially when it comes to discussing the (often controversial) topic of core stability. Traditionally regarded as encompassing the pelvic floor, diaphragm, deep abdominal muscles (particularly Transversus Abdominus), our definitions of ‘the canister’ or ‘core’ have of late expanded to include psoas, obturator internus, quadratus lumborum and the osseous components of the pelvic girdle (Chaitow 2012).
 Often, we in pelvic rehab bemoan the fact that the pelvic floor is not given the attention it deserves (when we know it really is the answer to everything…) but I do believe that we, as pelvic health specialists are just as guilty of not paying enough attention to the ‘roof’ of the canister, the diaphragm.
Often, we in pelvic rehab bemoan the fact that the pelvic floor is not given the attention it deserves (when we know it really is the answer to everything…) but I do believe that we, as pelvic health specialists are just as guilty of not paying enough attention to the ‘roof’ of the canister, the diaphragm.
The diaphragm and the pelvic floor are bound together structurally and functionally by both fascial and muscular connections (Chaitow 2012). The anatomical link between the diaphragm, psoas and the pelvic floor has been explored by Gibbons in 2001 ‘…The diaphragm’s medial arcuate ligament is a tendinous arch in the fascia of psoas major. Distally, the psoas fascia is continuous with the pelvic floor fascia, especially the pubococcygeus’. Newell in 2005 discussed the relationship between the diaphragm and transversus abdominus and Carriere in 2006 concluded that psoas spasm may influence diaphragmatic mechanics, and conversely that abnormal tensions in the medial arcuate ligament of the diaphragm may irritate psoas.
Paul Hodges has also concluded in his 2007 paper that breathing and continence may be more connected to low back pain than levels of activity or BMI, reinforcing Smith’s 2006 study looking at the link between breathing disorders, pelvic floor dysfunction and back pain in over 38,000 Australian women.
Of course, breathing, like pelvic floor functioning, can also be linked to psychological factors: when we are stressed, our breathing tends to become more apical (and our pelvic floors may hold excess tension). When that becomes habitual rather than a temporary stress response, a sub-optimal breathing pattern may develop, which disrupts the abdominal muscle balance and makes both back and pelvic pain more likely, with the added risk of pelvic venous congestion (Chaitow 2012). Myofascial trigger points may also develop because of restricted breathing patterns. We also know the opposite is true – such as using controlled breathing to calm down, to let go of tension and even to modify pain and autonomic responses (Busch 2012). Athletes may be at a particular risk of dysfunction, competing at high levels of intensity, both physically (in competition?) and psychologically (fear of losing a college scholarship?) Although more research is needed to confirm or disprove these connections, theoretically normalizing breathing patterns may improve outcomes in cases of low back or pelvic pain.
In my specialist course ‘The Athlete & the Pelvic Floor’ in Denver next month, we will look at specific manual therapy interventions for the diaphragm and its allies, the psoas and quadratus lumborum. As with any manual therapy techniques, we must always follow up with a clinical and home exercise program, or the effects will be only temporarily beneficial (Coronado 2011, Hegedus 2012) and so we will look at breath re-patterning, integration with the pelvic floor and how this is an often overlooked step when it comes to managing athletes with pelvic floor dysfunction. Hope to see you there!
References:
1. Chaitow, L & Jones, R (Eds) ‘Chronic Pelvic Pain and Dysfunction 2012 Elsevier Churchill Livingstone
2. Gibbons, S.G.T. 2001 The model of Psoas Major stability function. In: Proceedings of 1st International Conference on Movement Dysfunction, Sept 21-23 Edinburgh, Scotland
3. Newell, R. 2005 Anatomy of the post-laryngeal airways, lungs and diaphragm. Surgery 23 (11) 393-397
4. Carriere, B 2006 Interdependence of Posture and the Pelvic Floor. In: Carriere, B The Pelvic Floor, Thieme New York
5. Hodges, P, Sapsford, R, Pengel, L 2007 Postural and respiratory functions of the PFMs. Neorourol. Urodyn. 26 (3), 362-371
6. Smith, M, Russell, A, Hodges, P., 2006 Disorders of breathing and continence have a stronger association with back pain than obesity and physical activity. Aust. J. Physiother. 21(52) 11-16
7. Coronado, R, Bialosky, J & Cook, C. 2010 The temporal effects of a single session of high-velocity, low-amplitude thrust manipulation on subjects with spinal pain Physical Therapy Reviews Volume 15, Issue 1 (01 February 2010), pp. 29-35
Michelle Lyons is instructor of "Oncology and the Female Pelvic Floor: Female Reproductive and Gynecologic Cancers", among other Herman & Wallace courses. We thought you might like to hear her expert analysis of current research going on in the field of gynecologic oncology, and the benefits therapeutic yoga can have on patient rehabilitation. Take it away, Michelle!

More than 65,000 women are diagnosed with gynecologic cancers (vulvar, vaginal, cervical, ovarian, endometrial) in the United States each year (Sohl et al 2012). Treatment options for these women include surgery, chemotherapy, radiation and hormone therapy – all of which have the potential to have local, regional and global effects on a woman’s body. The pelvic rehab specialist is in a unique position to hugely improve quality of life issues for these women – dealing with issues directly associated with pelvic health (urinary, sexual and bowel function and dysfunction) as well as more global issues such as bone health, peripheral neuropathies and musculoskeletal dysfunctions.
Yoga has enormous potential as a therapeutic tool for gynecologic cancer survivors and as exercise prescription experts, we can add yoga as a multi-purpose tool to our skill-set.
Empirical research on therapeutic yoga has been ongoing for several decades, including several recent studies conducted with cancer patients and survivors. Although most of the research looking at the benefits of yoga for cancer survivors has been done in the context of breast and prostate cancers, we can safely extrapolate many of the benefits associated with oncology rehab yoga, including its immediately obvious ability to improve flexibility, strength, balance, but also the impact yoga can have on decreasing inflammation, improving sleep and raising quality of life scores in pelvic cancer survivors.
Recent papers by Dewhirst et al showed how moderate exercise can improve the efficacy of chemotherapy and radiation by decreasing tumour hypoxia – they also discovered that this may limit metastatic aggression.
We also know that exercise can be potent medicine when it comes to dealing with the effects of cancer treatments, especially fatigue, bone health and cardiovascular function, which may disrupt return to exercise (Kerry et al 2005). But pelvic cancer patients may face extra barriers when it comes to returning to exercise, such as pelvic pain and concerns about continence, as well as diminished flexibility, balance and strength. But as Blaney et al concluded in their 2013 paper ‘…however, the main barriers reported were those that had the potential to be alleviated by exercise.’ And in my opinion, this can be achieved by integrating yoga into our pelvic oncology rehab programs.
These recent and exciting research findings have encouraged me to add a therapeutic yoga lab session to my Oncology & the Pelvic Floor course, which I will be teaching in NY next month. This is the last chance to catch this course stateside this year so I hope you will join me in White Plains to explore the many ways we can make a serious impact on pelvic cancer survivorship (Bring your yoga mat!)
References:
Psychooncology. 2013 Jan;22(1):186-94.
Cancer survivors' exercise barriers, facilitators and preferences in the context of fatigue, quality of life and physical activity participation: a questionnaire-survey. Blaney JM1, Lowe-Strong A, Rankin-Watt J, Campbell A, Gracey JH.
Annals of Behavioral Medicine
April 2005, Volume 29, Issue 2, pp 147-153
A Longitudinal Study of Exercise Barriers in Colorectal Cancer Survivors Participating in a Randomized Controlled Trial
Kerry S. Courneya Ph.D., Christine M. Friedenreich Ph.D., H. Arthur Quinney Ph.D., Anthony L. A. Fields M.D., Lee W. Jones Ph.D., Jeffrey K. H. Vallance M.A., Adrian S. Fairey M.Sc.
JNCI J Natl Canc
Allison S. Betof, Christopher D. Lascola, Douglas H. Weitzel, Chelsea D. Landon, Peter M. Scarbrough, Gayathri R. Devi, Gregory M. Palmer, Lee W. Jones, and Mark W. Dewhirst
Modulation of Murine Breast Tumor Vascularity, Hypoxia, and Chemotherapeutic Response by Exercise
Today we present Part II of Michelle Lyons' discussion on sex after gynecologic cancer. Michelle will be teaching a course on this topic in White Plains in August!
In Part One of this blog, I looked at the sexual health issues women face after gynecologic cancer. In Part Two, I want to explore different treatment options that we as pelvic rehab specialists can employ to help address the many implications of cancer and cancer treatment
Treatment for gynecologic cancers, including vulvar, vaginal, cervical, endometrial and ovarian cancers, may include surgery, radiation therapy, chemotherapy, and/or hormonal therapy. We know that any of these approaches can have an adverse effect on the pelvic floor, as well as systemic effects on a woman’s body. Issues can include pain, fibrosis, scar tissue adhesions, diminished flexibility, fatigue and feeling fatigued and unwell. The effects on body image should not be under-estimated either. In their paper ‘Sexual functioning among breast cancer, gynecologic cancer, and healthy women’, Anderson & Jochimsen explore how ‘…body-image disruption may be a prevalent problem for gynecologic cancer patients…more so than for breast cancer patients’. The judicious use of manual therapy and local and global exercise prescription may be excellent pathways for a women to re-integrate with her body.
Many women will have to learn to care for a new colostomy or how to catheterize a continent urostomy. A woman who has had a vulvectomy will need sensitive counselling to understand that she can still respond sexually. Patients who have had a vaginectomy with reconstruction as part of a pelvic exenteration will need extensive rehab to help them achieve successful sexual functioning. We as pelvic rehab practitioners are in a uniquely privileged position – not only can we ask the questions and discuss the options but we are licensed to be ‘hands on’ professionals, using our core skills of manual therapy, bespoke exercise advice and educating our patients about a range of issues from the correct usage of lubricants, dilators, sexual ergonomics and brain/pain science. I am in the habit of describing pelvic rehab as the best specialty in physical therapy but I think this is especially true when it comes to the junction of oncology and pelvic health. This is where we can integrate our knowledge of neuro-science, orthopaedics, the lymphatic system and pelvic health to deal with the effects of pelvic cancers and their treatment.
In Farmer et al’s 2014 paper, ‘Pain Reduces Sexual Motivation in Female But Not Male Mice’ , the authors found that ‘Pain from inflammation greatly reduced sexual motivation in female mice in heat -- but had no such effect on male mice’. Unfortunately ongoing pelvic pain is a common sequela of treatment for gynecologic cancers – reasons ranging from post-operative adhesions, post-radiation fibrosis or vaginal stenosis or genital lymphedema. It is also worth bearing in mind the ‘rare but real’ scenario of pudendal neuralgia following pelvic radiation, as discussed by Elahi in his 2013 article ‘Pudendal entrapment neuropathy: a rare complication of pelvic radiation therapy.’
The good news is that we have much to offer. Yang in 2012 (‘Effect of a pelvic floor muscle training program on gynecologic cancer survivors with pelvic floor dysfunction: A randomized controlled trial’) showed that pelvic rehab improved overall pelvic floor function, sexual functioning and QoL measures for gynecological cancer patients. Yang’s pelvic rehab group (administered by an experience physiotherapist) displayed statistically significant differences in physical function, pain, sexual worry, sexual activity, and sexual/vaginal function. Gynecological cancer and treatment procedures are potentially a fourfold assault: on sexual health, body image, sexual functioning, and fertility. Sexual morbidity is an undertreated problem in gynecological cancer survivorship that is known to occur early and to persist beyond the period of recovery (Reis et al 2010). We have a good and growing body of evidence that pelvic rehab, delivered by skilled therapists, has the potential to address each of these issues. And perhaps, most encouraging, here is Yang’s conclusion: ‘…‘Pelvic Floor Rehab is effective even in gynecological cancer survivors who need it most.’ (Yang 2012)
Interested in learning more about the role of pelvic rehab in gynecologic cancer survivorship? Join me in White Plains in August!
The following comes to us from Herman & Wallace faculty member Michelle Lyons. Michelle travels the world spreading the word about pelvic rehabilitation and the powerful benefits it can have on a patient's everyday life. Michelle will be teaching her newest course, "Oncology and the Female Pelvic Floor: Female Reproductive and Gynecologic Cancers" in White Plains, NY this August 14 - 15. Join her to learn more about evaluating and treating oncology patients.

According to the Scientific Network of Female Sexual Health and Cancer, ‘Sexuality is an experience that really is at the intersection of mind, body and relationship, and cancer treatment can impact all three of those elements”. Dr Sharon Bober of Dana Farber says ‘Part of the problem is that doctors are so focused on saving a cancer patient's life that they forget to discuss issues of sexual health. My sense is that it's not about physicians or health care providers not caring about your sexual health or thinking that it's unimportant, but that cancer is the emergency, and everything else seems to fall by the wayside".
If you harness the power of Google to look up female sexual dysfunction after gynaecologic cancer, you may see phrases like ‘Possible sexual side effects…’ or ‘Cancer treatment can cause physical changes that make having sex more difficult’ or even ‘cancer treatments may make intercourse painful’. To call these descriptions ‘understatements’ does not really do them justice.
For many women post-gynaecological cancer, resuming sexual function can be a multi-faceted problem. Issues can range from dealing with Cancer Related Fatigue and nausea, vomiting or diarrhea to physical changes in the size and shape of the vaginal canal. Cancer treatments can also cause hormone imbalances and tissue damage. Add to this issues with post-surgical/radiation adhesions, a disruption to the ability to produce lubrication, challenges to the musculo-skeletal systems within the hips and the pelvis as well as the onset of medically induced menopause….well you get the picture.
In a 2009 paper, ‘Interventions for sexuality after pelvic radiation therapy and gynaecological cancer’, Katz talks about the fact that ‘…very little attention has been paid to the sexual difficulties women experience after radiation to the sexual organs. There are a limited number of interventions for the woman who has been treated for gynaecological cancer with radiation. These focus on the provision of information and some specific suggestions related to treating vaginal dryness, the need for vaginal dilatation after radiation therapy, and management of fatigue. In ‘A systematic review of sexual concerns reported by gynaecological cancer survivors’ (Abbot Anderson 2012), the author points out that common concerns in the physical dimension were dyspareunia, changes in the vagina, and decreased sexual activity.
In the psychological dimension, common concerns were decreased libido, alterations in body image, and anxiety related to sexual performance. And in the social dimension, common concerns were difficulty maintaining previous sexual roles, emotional distancing from the partner, and perceived change in the partner's level of sexual interest.
The good news is that you can return to a normal sex life after surviving gynaecological cancer – particularly with the help of a skilled pelvic rehab provider.
In part 2 of this blog series, I will look at specific interventions in sexual rehab for the gynaecological cancer survivor. Interested in learning more about pelvic rehab and oncology? Join me in White Plains in August!
Calling all Pelvic Rehab tweeters! On June 24th, there will be a tweetchat hosted by 'Living Beyond Breast Cancer' to discuss and explore the effects of breast cancer on sexual health. Topics will include:
- How diagnosis and treatment side effects can affect intimacy and sexuality
- How to communicate with your cancer care team and partner
- Tips and suggestions for managing these side effects

Now, while I think it is brilliant that we are talking about sexuality during and after cancer, the panel has no input from pelvic rehab providers! We have so much to offer women in terms of sexual rehab in an oncology setting but if our colleagues and patients don't know about us.....
So some along and join the conversation on twitter on the 24th - don't forget to use the hashtag #LBBCchat. Hope to see you there to help raise the profile of pelvic rehab in the world of oncology.
Interested in learning more about sexual rehab after gynecologic cancer? Join me in White Plains NY this August!

