I’m Elizabeth Hampton PT, DPT, WCS, BCB-PMD and I teach “Finding the Driver in Pelvic Pain”, which offers practitioners a systematic screening approach to rule in or rule out contributing factors to pelvic pain. This course helps clinicians to understand and screen for the common co-morbidities associated with pelvic floor dysfunction, like labral tears, discogenic low back pain, nerve entrapments, coccygeal dysfunction, and more. Importantly, it also coaches clinicians to organize information in a way that enables them to prioritize interventions in complex cases. I've noticed that there are some questions that course participants frequently have as they talk through common themes in their care challenges and wrote this blog to share some clinical pearls you may find to be helpful for your own practice or as an explanation to your clients.
Here are some of the most common questions that I get when teaching Finding the Driver in Pelvic Pain:
1) Question: How do I even start to organize information when a client has a complex history and I am feeling overwhelmed?
I write down a road map with key categories: Bowel and bladder; Spine; Sacroiliac Joint/Pubic Symphysis; Hip; Pelvic floor muscles; biomechanics; respiration; neural upregulation; whatever details can be fit into ‘big buckets’ of information. I use it to both organize my thoughts for my notes, as well as educate the client as to what my findings are and the design of their treatment program.
2) Question: How do you get your clients to do a bowel and bladder diary?
I am proud to say that I can talk anyone into a 7 day bowel and bladder diary because I tell them how incredibly helpful it is to understand the way their body responds to what they eat, drink, and daily habits. It’s my secret weapon to snag clients to start connecting with their body and listening to their details, educate about defecation ergonomics and what happens in multiple systems when there is pelvic floor overactivity. It’s a great teaching tool that facilitates self-reflection and how their self-care choices impact their body’s behavior.
3) Question: How do you educate clients about pelvic floor function so they don’t focus so much on Kegels?
Pelvic floor muscles do three things:
-
They contract gently, or powerfully, with no discomfort, and totally normal breathing; PFMs should have the same kind of nuanced control like your voice does: they should be able to do a gentle contraction, like a “whisper” or a powerful contraction, like a “shout”, depending on the task position and intent.
-
They relax fully and completely when the body is resting in support, or they should be able to relax to a supportive level when they are needed posturally. Relaxation should be its own celebrated event!
-
They should be able to relax and gently lengthen.
Faculty member Elizabeth Hampton PT, DPT, WCS, BCB-PMD is the author and instructor of Finding the Driver in Pelvic Pain, a course designed to help practitioners utilize differential diagnosis in evaluating pain. Join Dr. Hampton in Portland, OR on July 27-29, 2018 or November 2-4, 2018 in Phoenix, AZ.
Erica Vitek, MOT, OTR, BCB-PMD, PRPC is the author and instructor of Neurologic Conditions and Pelvic Floor Rehab, a new course coming to Grand Rapids, MI and Philadelphia, PA. This post is the next in her series on creating a course about neurologic conditions and pelvic rehabilititation.
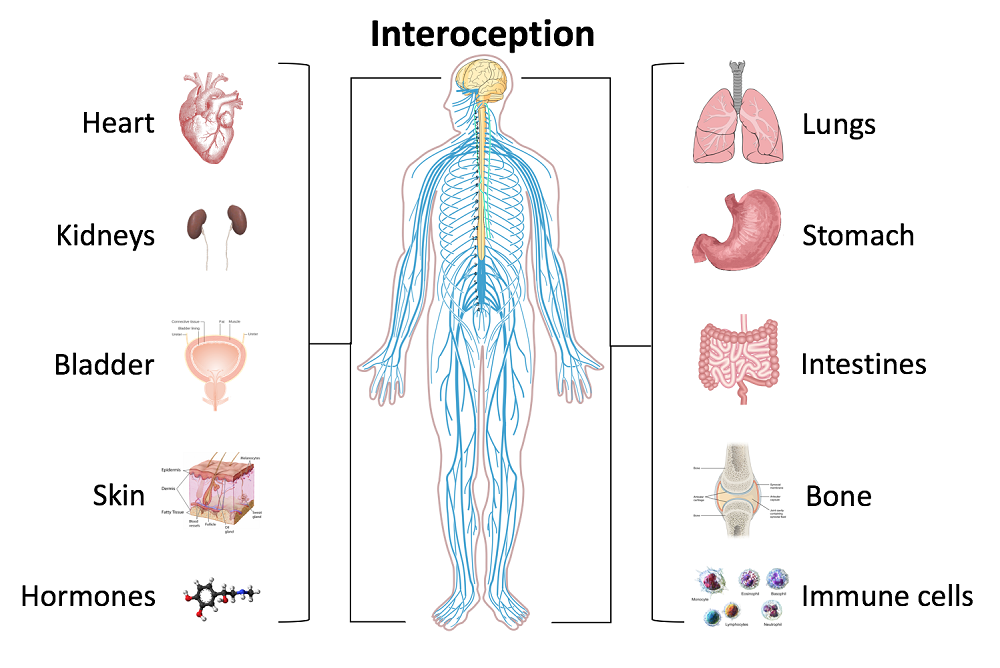
Being a clinician, as we evaluate and treat people with pelvic health conditions, we typically take all systems of the body into account. We take the problem presented to us by the client and we examine, from all angles, how we might go about advice and treatment to best achieve their goals in alleviating the problem. We do a full review of medical history and pharmacology. We examine our client in-depth from a musculoskeletal perspective. We look at psychological contributions to the problem they are facing. We can look at their lifestyle and have them make a detailed diary to help us analyze their bladder, bowel, fluid intake and dietary habits. Do we also always include a look at the neurological components? Do we know what we are looking for? What are the best tools we can have in our toolbox as clinicians to look at our client’s problem through a “neuro brain”?
 In writing each lecture of this course, I have had to step back each time I am developing a new concept and look at it with in-depth thought and contemplation about how I will use this in the clinic to assess my client’s concerns using a neuro-based approach. Taking the concepts and facts about the musculoskeletal system that we know well and then taking a look at the neurological systems contributions and relationship to that dysfunction can be challenging. The main reason for this challenge is that neuro system dysfunction is many times hard explain, presents with inconsistent or changing symptoms, may have motor or sensory deficits together or by themselves, may radiate to different locations than where the true dysfunction is located, and may have developed into central sensitization causing a hypervigilance to typically non-painful stimuli.
In writing each lecture of this course, I have had to step back each time I am developing a new concept and look at it with in-depth thought and contemplation about how I will use this in the clinic to assess my client’s concerns using a neuro-based approach. Taking the concepts and facts about the musculoskeletal system that we know well and then taking a look at the neurological systems contributions and relationship to that dysfunction can be challenging. The main reason for this challenge is that neuro system dysfunction is many times hard explain, presents with inconsistent or changing symptoms, may have motor or sensory deficits together or by themselves, may radiate to different locations than where the true dysfunction is located, and may have developed into central sensitization causing a hypervigilance to typically non-painful stimuli.
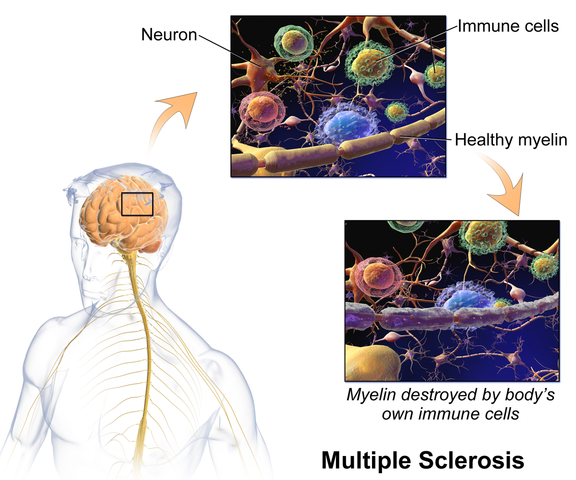
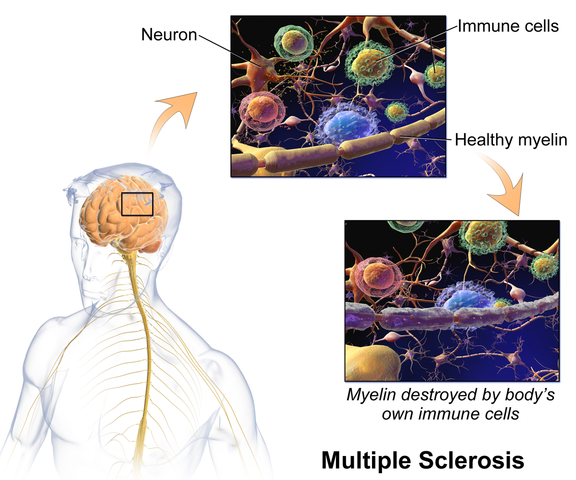
In brain storming our ideas for course creation, much was said about thinking back to college or other continuing education courses and “learning a little about a lot of things neuro” but not the in-depth knowledge one might want to have when focusing their attention on specific neurodegenerative conditions such as Parkinson disease, demyelinating diseases such as Multiple Sclerosis, injury to the brain due to cerebral vascular accident or incomplete or complete spinal cord injury.
As I progress deep into the development of this course, I have my “neuro brain” on and a persistent focus set on providing clinicians with as much in-depth information on neurological contributions to pelvic floor function and dysfunction. I want clinicians to walk away from this course feeling confident that through evaluation of a client that has been diagnosed with Parkinson disease, Multiple Sclerosis or suffered a spinal cord injury, they would have the tools to develop an in-depth treatment plan that would provide these clients with the best results possible to improve their quality of life. I also want clinicians to have the confidence to market themselves to their local neurologists. This is an entirely new avenue for developing a referral base in pelvic health work. Many times for clients who have chronic neurological conditions, the problem list is long and bladder, bowel and sexual health concerns might not even be broached within the very short physician appointment times. We can give our neurologists new treatments to be confident in and excited about to improve their patient’s quality of life!
Tiffany Ellsworth Lee MA, OTR, BCB-PMD joined the Herman & Wallace faculty to teach a course on biofeedback along with Jane Kaufman, PT, M.Ed, BCB-PMD. The month of April is Occupational Therapy month, and we are celebrating by highlighting the role that Occupational Therapists play in pelvic floor rehabilitation. Tiffany founded a biofeedback program at Central Texas Medical Center in San Marcos in 2004, and currently runs her a pelvic rehab private practice .
 Working in this area of biofeedback is extremely rewarding and fulfilling to help change peoples’ lives. I have a private practice now exclusively dedicated to treating patients with pelvic floor dysfunction. I became involved in working with patients with incontinence and pelvic floor disorders because of many opportunities along my career path. I have been an Occupational Therapist since 1994. Both of my parents are also OTs, so I think I was born to do this!
Working in this area of biofeedback is extremely rewarding and fulfilling to help change peoples’ lives. I have a private practice now exclusively dedicated to treating patients with pelvic floor dysfunction. I became involved in working with patients with incontinence and pelvic floor disorders because of many opportunities along my career path. I have been an Occupational Therapist since 1994. Both of my parents are also OTs, so I think I was born to do this!
Erica Vitek, MOT, OTR, BCB-PMD, PRPC wrote a blog recently about the role of OTs in pelvic health. She writes:
“As we look closer at the framework and the definition of OT (Occupational Therapy Practice Framework: Domain and Process, 3rd edition 2014), there is clear evidence that the occupational therapist (OT) has a role in the treatment of pelvic health conditions. Importantly, occupations are defined by this document as ‘…various kinds of life activities in which individuals, groups, or populations engage, including activities of daily living (ADL), instrumental activities of daily living (IADLs), rest and sleep, education, work, play, leisure, and social participation.”
The clearest examples of the OT’s role in pelvic health occupations within this section include:
- ADL section: toileting and hygiene (continence needs, intentional control of bowel movements and urination) and sexual activity.
- IADLs section: sleep participation (sustaining sleep without disruption, performing nighttime care of toileting needs).
- Achieving full participation in work, play, leisure, and social activities, requires one to be able to maintain continence in a socially acceptable manner in which they can feel confident and comfortable to fulfill their roles and duties.
"We believe that the great patient need that exists can be better served by having trained OTs able to treat pelvic health conditions"
How to get started as an OT
Occupational therapists wishing to pursue pelvic floor have a few options. The first thing is to find a pelvic floor clinical setting or work with their respective settings to check to see if they can start a women's health program with a strong focus on pelvic floor. OTs quite often do not start out in pelvic health directly after school and since this is a newer area as compared to other certifications such as the NDT and PNF it takes a little bit of research, time and effort to find one’s exact niche. To get started, an OT should seek out courses that teach the basics of bladder and bowel management. It is important to understand the anatomy and physiology of the bladder, bowel, and sexual systems.
Incontinence and pelvic floor disorders have a profound impact on occupation, the daily activities that give life meaning! OTs should have a larger role in treating this patient population. Offering hope to our patients is imperative when he/she is dealing with pelvic floor dysfunction!
Keep an eye out for an upcoming post from Tiffany with some inspiring clinical case studies. You can join Tiffany and Jane Kaufman in Biofeedback for Pelvic Muscle Dysfunction to get lots of hands-on time with surface eletromyography, and to work toward BCIA certification!
Sara Chan Reardon, DPT, WCS, BCB-PMD is a pelvic floor dysfunction specialist practicing in New Orleans, LA. Sara was named the 2008 Section on Women’s Health Research Scholar for her published research on pelvic floor dyssynergia related constipation. She was recognized as an Emerging Leader in 2013 by the American Physical Therapy Association. She served as Treasurer of the APTA’s Section on Women's Health and sat on their Executive Board of Directors from 2012-2015. Today she was kind enough to share a bit about her course Post-Prostatectomy Patient Rehabilitation, which is taking place twice in 2018.
 My name is Sara Reardon, and I teach the Post-Prostatectomy Patient Rehabilitation course, which I wrote and developed in the year 2015. At the time, I had been a pelvic health Physical Therapist for over 10 years. Earlier in my career, I had taken the Pelvic Floor 2A course by Herman and Wallace Institute, which was a fantastic and thorough introduction to treating a male patient.
My name is Sara Reardon, and I teach the Post-Prostatectomy Patient Rehabilitation course, which I wrote and developed in the year 2015. At the time, I had been a pelvic health Physical Therapist for over 10 years. Earlier in my career, I had taken the Pelvic Floor 2A course by Herman and Wallace Institute, which was a fantastic and thorough introduction to treating a male patient.
Over the years, I started seeing more and more men with post-prostatectomy urinary incontinence and erectile dysfunction in my clinic. Urinary incontinence is the most common and costly complication in men following prostate removal surgery, and their quality of life is directly related to their duration of experiencing those symptoms. Evidence supports that pelvic floor muscle training started as soon as possible after surgery can help decrease incontinence and improve quality of life. I enjoyed being able to help men decrease their incontinence and improve their other symptoms after all they had been through following a cancer diagnosis and treatment.
No courses focused specifically on treating post-prostatectomy pelvic floor dysfunction were offered at the time, so I scoured the research, shadowed with physicians, observed surgeries, and attended urology conferences to understand how to effectively treat these individuals. Treating this population of men is fun, fulfilling, and rewarding, and I was inspired to help other pelvic health physical therapists dive deeper as I witnessed the impact pelvic health physical therapy can have on the quality of life of these patients. I love teaching this course, and I am excited to help other pelvic health professionals learn evidence based and effective treatment strategies to help these men navigate their recovery after prostatectomy.
Join Dr. Reardon in Philadelphia, PA on June 2-3, 2018 or in Houston, TX on November 10-11, 2018 to learn evaluation and treatment techniques for men recovering from prostatectomy surgery.
Using sEMG biofeedback to get real-time results
Tiffany Lee, MA, OTR, BCB-PMD and Jane Kaufman, PT, BCB-PMD are internationally board-certified clinicians in the treatment of pelvic floor muscle dysfunction through the Biofeedback Certification International Alliance. Combined, they have over fifty years of treatment experience using sEMG biofeedback. Their new course, “Biofeedback for Pelvic Floor Muscle Dysfunction”, will provide the nuts and bolts of this powerful tool so that clinicians can return to the clinic after this course with another component to their toolbox of treatment strategies.
 As a clinician treating patients with pelvic floor muscle dysfunction, have you gone away from a treatment session and asked yourself ‘what else can I do for this patient?’. Have you considered adding surface EMG, often referred to as biofeedback, to your treatment plan, but aren’t sure how to go about it correctly or effectively? Perhaps you think you can’t use the sensor because the patient has pain. Maybe you think biofeedback only helps with up-training or strengthening.
As a clinician treating patients with pelvic floor muscle dysfunction, have you gone away from a treatment session and asked yourself ‘what else can I do for this patient?’. Have you considered adding surface EMG, often referred to as biofeedback, to your treatment plan, but aren’t sure how to go about it correctly or effectively? Perhaps you think you can’t use the sensor because the patient has pain. Maybe you think biofeedback only helps with up-training or strengthening.
So exactly what is biofeedback? Why should I consider this modality? Biofeedback provides a non-invasive opportunity for patients to see muscle function visualized on a computer screen in a way that allows for immediate feedback, simple representation of muscle function, and allows the patient and the clinician the opportunity to alter the physiological process of the muscle through basic learning strategies and skilled cues. Many patients gain knowledge and awareness of the pelvic floor muscle through tactile feedback, but the visual representation is what helps patients really hone in on body awareness and connect all the dots. Here are a few comments that our patients have made; “I can now pay attention to my muscle while at work thanks to the visual of my muscle when sitting and standing”; “I needed to see my muscle to fully understand how to release the tension in it “; “I totally get what I need to do now that I have a clear picture of what you want”; “Seeing is believing”.
A 2017 study by Moretti, E., et al. is a great article that helps support the concept that measuring the pelvic floor electrical activity through a standard vaginal sensor is not always an option. For many patients, use of surface electrodes with peri-anal electrodes will provide the same reading and offer a more comfortable alternative for those patients who cannot use an internal sensor. This allows the clinician more opportunities to use this treatment modality with ease and assurance that the patient can learn from the visual representation of the muscle without fear of penetration from a sensor, and get great results!
In another study by Aysun Ozlu MD, et al. the authors conclude that biofeedback assisted pelvic floor muscle training, in addition to a home exercise program, improves stress urinary incontinence rates more than home exercise program alone.
Herman & Wallace is offering a course for clinicians in Alexandria, Virginia this June that will answer all of your questions and concerns about this fabulous treatment tool: biofeedback! This course enables the clinician to learn and practice this valuable tool and gain knowledge about the benefits of this modality, so that treatment can begin immediately with ample opportunity for patient’s positive feedback and awareness of muscle function. Participants will experience being a biofeedback practitioner and patient (using a self-inserted vaginal or rectal sensor). Participants will be administering biofeedback assessments, analyzing and interpreting sEMG signals, conducting treatment sessions, and role-playing patient instruction/education for each diagnosis presented during the many hands-on lab experiences. Biofeedback is a powerful tool that can benefit your patient population, and add to your skill-set.
Moretti, E., Galvao de moura Filho, A., Correia de Almedia, J., Araaujo, C., Lemos, C. “Electromyographic assessment of women’s pelvic floor: What is the best place for a superficial sensor?” Neurology and Urodynamics; 2017; 9999:1-7.;
Aysun Ozlu MD, Neemettin Yildiz MD, Ozer Oztekin MD, “Comparison of the efficacy of perineal and intravaginal biofeedback assisted pelvic floor muscle exercises in women with urodynamic stress urinary incontinence”
In an effort to provide the best possible educational experience for clinical rehabilitation application of neuroanatomy, I was on a mission. Having a core, base knowledge review of the nervous system is essential when leading into talking about dysfunction and disease of that system. I went on a search for anatomical depictions that could clearly identify the structures and processes I was trying to portray. New books from the library and books I own from when I was in college serve as great resources when trying to get back into studying the specifics, but do not offer the opportunity to easily get these images into a powerpoint. Online resources are also challenging. I am learning how time consuming the process can be to determine who owns the online image, if it is free to copy, save and utilize for my own teaching purposes, or if I need to go through the process of requesting permissions for use.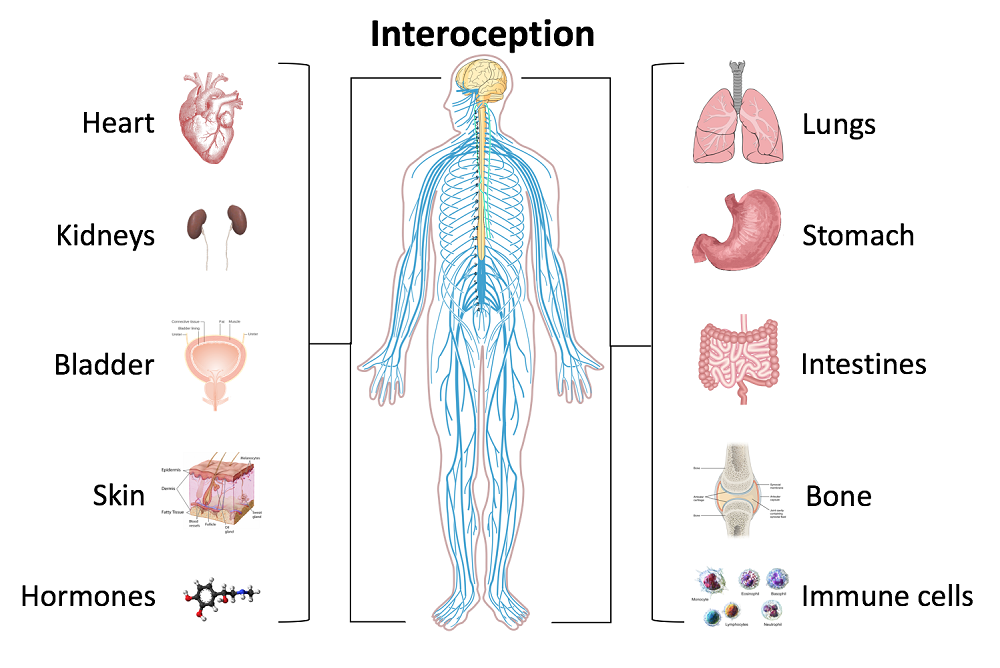
Through my employer, where I treat patients in the clinic, I have access to a program called Primal Pictures. I had used this in the past for clinic related marketing presentations and educational materials for patients and other clinicians I have mentored. Looking into the product further, I came to find out that there is a newer version of the program which offered so many more options. A truly unlimited amount of images which can be manipulated into an optimal position depicting the most clear neuroanatomical views I have ever been able to find. Not only does it provide me with the images I need in order to depict the treacherous pathways of the nerves in our body, but it also provides some amazing depictions of the physiological processes that occur within our nervous system to allow for healthy day to day functioning and protection of our bodies.
I also came across the title of a journal article that I was sure would provide some excellent depictions of neuroanatomy. The article titled, Sectional Neuroanatomy of the Pelvic Floor, provides cross sectional views of both the male and female pelvises. I obtained the article which has an excellent color-coded system, each nerve colored the same as the muscles and skin surface it innervates, going from superior to inferior cross sections. This makes for a clear understanding of each structures anatomical position. It is a great reference when looking at the anatomical relationships to adjacent structures and can help guide palpation skills. The article was more specifically written for physicians to best direct needle procedures/injections in the most accurate location possible when targeting nerves and structures. Neuroanatomy and physiology can be essential to understanding certain patient populations we encounter as we practice pelvic floor rehabilitation. Having clear depictions to refer to can help you provide the best possible base knowledge to your patients as you help them understand the challenges they face and how to overcome them.
Kass, J. S., Chiou-Tan, F. Y., Harrell, J. S., Zhang, H., & Taber, K. H. (2010). Sectional neuroanatomy of the pelvic floor. Journal of computer assisted tomography, 34(3), 473-477.
The following is the first in a series of posts by Erica Vitek, MOT, OTR, BCB-PMD, PRPC. Erica joined the Herman & Wallace faculty in 2018 and is the author of Neurologic Conditions and Pelvic Floor Rehab.

Looking back, being passionate about how to physically exercise a person with Parkinson disease to produce the best functional outcome actually became a passion of mine when I was offered my first job. I was thrown into treating people with Parkinson disease in an acute care setting. I had very limited knowledge about Parkinson disease at the time, but I learned quickly from the vast opportunity that was offered to me through my place of work, which was the regions sought after Parkinson disease center of excellence. At the same time, I was eager to further advance my skills as a pelvic floor therapist, which I developed a substantial interest in when I was in college.
As I learned more about what people with Parkinson disease had to manage in their daily lives, it became very clear to me that autonomic dysfunction was a very challenging, and sometimes disabling, aspect of the disease. Being knowledgeable about the neurological and musculoskeletal system along with the urinary, gastrointestinal, and sexual systems seemed to fit well together but there was no specific place to go to combine this knowledge. The research I began collecting on this topic was abundant and very intriguing. Bringing this information together could be practice changing for me to help people living with Parkinson disease.
As clinicians, we already know how to be understanding about the very personal details of the people we work with. People with Parkinson disease deal with an extra layer of challenge, such as, bradykinesia, freezing of gait, and tremor affecting their day to day self-care and relationships. Adding urinary incontinence, constipation or sexual dysfunction to the list makes for even more difficult management.
How does one clinician share their passion with other clinicians that also have the same desires to give the best care to their patients with Parkinson disease? Having a great deal of respect for Herman and Wallace and what they have to offer clinicians practicing pelvic rehabilitation, it seemed like it could be the perfect fit for a course like this. The work that would lie ahead if this idea took off was overwhelming but did not hinder me from my proposal. In fact, it has led to an even larger scope addressing the of treatment of the pelvic floor for a multitude of neurologic conditions many of us see daily in our clinics. Pulling it all together to share is a process that will reward not only people with Parkinson disease in my practice but hopefully yours as well.
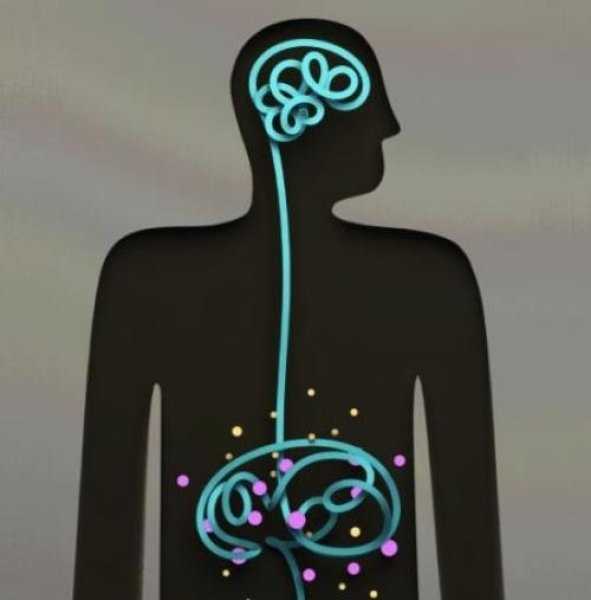
Recently I had a patient referred to me for fecal incontinence. She looked so familiar to me and we realized she had seen me before, years ago, for bladder issues. She was a sweet 60 something single woman who had raised 6 kids on her own after her husband left her. We laughed as she remembered something funny I had said back then. Then we got down to business. In recent years my patient “Inez” had been diagnosed with both diabetes and Crohn’s disease. She was managing the Crohn’s very well but her sugars were much harder for her to get under control. When I asked her about her current complaints and symptoms she reported that most days her bowels were perfect. She reported one or two soft easy to pass stools per day. But when she had to leave the house for a doctor appointment, she would have explosive diarrhea. This didn’t happen if she went to the grocery store or to visit a friend. Upon further questioning she realized she was really anxious about her diabetes and her interactions with her medical provider regarding her diabetes had not been positive. She felt frustrated, scared, and powerless. 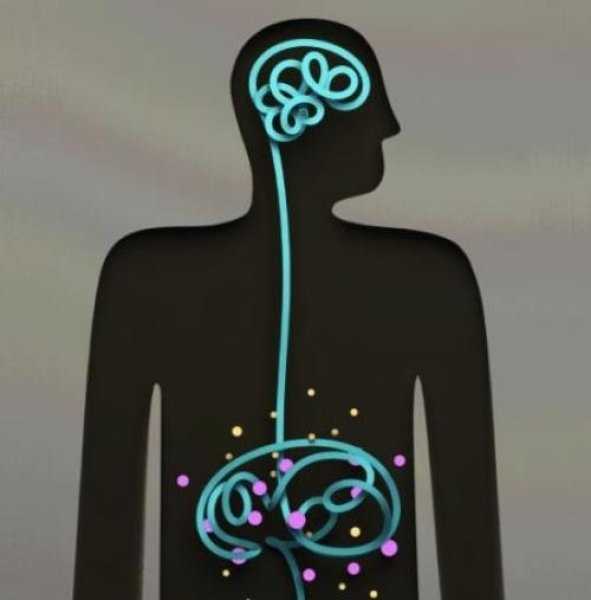
As a pelvic health PT I could have treated Inez in a variety of ways. With my initial exam I did not see any glaring musculoskeletal issues. I suggested to Inez the possibility that her nervous system was sending the wrong kind of signals to her bowels when she got anxious and that we could address this in PT. Inez agreed that she would like to try this approach. We decided that we would reevaluate after four visits to see if we needed to change the plan. Over four visits I used craniosacral therapy protocols to address nervous system upregulation and tension. I taught Inez relaxation techniques and encouraged 10 or 15 minutes of daily relaxation practice. Inez opened up about her relationship with her kids and how they tended to be takers but not givers. She would get frustrated and feel a bit used at times. We had conversations about boundaries and saying “no” and I shared some of my own experiences and struggles as well. Lastly we talked about how what we think can affect how we feel and what we do. Inez’s faith was important to her. She found a few bible verses that were meaningful to her about fear and anxiety and would repeat those during her daily relaxation time. On her fourth visit, Inez was all smiles. She brought me a jar of her homemade salsa as a graduation present. As we sat down to talk she reported to me that she saw her doctor yesterday. She had no bowel issues. And more than that, as her doctor began to talk over her she said to him, “No. Stop. You are always talking and never listening. I need you to listen to me today.” She went on to explain to him how it worried her that she was not able to control her diabetes well and she didn’t think he was doing enough to help her. Her physician did stop and listen and asked Inez, “what would you like me to do for you?” She asked for a referral to a specialist and he obliged. Inez was thrilled that she was able to manage her anxiety in a way that helped her bowels and to find the courage to confront her doctor to get the care she felt she needed.
As we grow in the knowledge of how the human body works it seems like all roads lead back to the nervous system. All of our treatments and interactions with patients affect the nervous system in one way or another. In our fast paced, stressed out world, finding ways to be intentional in addressing the nervous system can be a game changer for patients (as well as for ourselves). If this is an area you would like to grow in, please consider a new course being offered this January in Tampa, Florida. Participants taking Holistic Interventions and Meditation will experience and explore evidence-based information on strategies to address the nervous system. Topics covered include practical meditation, use of essential oils, supplements, yoga, calming and centering manual techniques and instruction in how to best dialogue with patients struggling with pain, anxiety and the effects of trauma. Nari Clemons and I hope to see you there.
Faurot, K. K. R., Gaylord, S., Palsson, O. S., Garland, E. L., Mann, J. D., & Whitehead, W. E. (2014). 715 Mindfulness Meditation Has Long-Term Therapeutic Benefits in Women With Irritable Bowel Syndrome (IBS): Follow-Up Results From a Randomized Controlled Trial. Gastroenterology, 146(5), S-124.
Kearney, D. J. (2012). Mindfulness meditation for women with irritable bowel syndrome–evidence of benefit from a randomised controlled trial. Evidence-based nursing, 15(3), 80-81.
Keefer, L., & Blanchard, E. B. (2001). The effects of relaxation response meditation on the symptoms of irritable bowel syndrome: results of a controlled treatment study. Behaviour research and therapy, 39(7), 801-811.
When it comes to discussing nutrition with our clients in pelvic rehab, it is normal to initially feel both uncertain and perhaps a bit overwhelmed at the prospect of delving into this topic. Yet we know that there must be links, some association between nutrition and the many chronic conditions we encounter. Gradually, over the last several years, a cornerstone of my practice with patients in pelvic rehabilitation has become providing nutritional guidance.
 I was both humbled and immensely grateful when many of my colleagues and peers attended Nutrition Perspectives for the Pelvic Rehab Therapist (NPPR) in Kansas City last March. In the following months, our clinics underwent a significant change in the types of discussions occurring with our patients. By embracing concepts presented in NPPR, a continuous stream of patient stories developed about lives having been touched by this shift. For many, “one small change” made a very big difference or served as the catalyst to many more positive lifestyle changes. Simply placing a high priority on re-thinking health situations through the lens of nourishment has been a very important shift, one that can occur across the spectrum of pelvic rehab practitioners if we choose to answer the call to “do what’s necessary”.
I was both humbled and immensely grateful when many of my colleagues and peers attended Nutrition Perspectives for the Pelvic Rehab Therapist (NPPR) in Kansas City last March. In the following months, our clinics underwent a significant change in the types of discussions occurring with our patients. By embracing concepts presented in NPPR, a continuous stream of patient stories developed about lives having been touched by this shift. For many, “one small change” made a very big difference or served as the catalyst to many more positive lifestyle changes. Simply placing a high priority on re-thinking health situations through the lens of nourishment has been a very important shift, one that can occur across the spectrum of pelvic rehab practitioners if we choose to answer the call to “do what’s necessary”.
Learning the essence of a topic outside our comfort zone is not easy, yet in present time is necessary for providers trying to grapple with how to wrap our professional minds around what we know in our hearts to be true: the effect of nourishment on health is profound. This brings to mind the resonating wisdom of Francis of Assisi:
“Start by doing what’s necessary, then do what’s possible;
and suddenly you are doing the impossible.”
At this crossroads in our health care system we know that nutrition matters. We must start by doing what’s necessary: acknowledging our role in helping patients along their path to a better life through less pain, ease of movement, normalization of function, and healing. With commitment to our patient’s well-being, we too must commit to investigating the realm of nutrition and rehabilitation. Next, we can strive to do what’s possible. NPPR can serve as a springboard for professionals ready to develop programs incorporating sound nourishment principles in relation to both specific conditions in pelvic rehab and general health and well-being. Finally, we may - in a few short years - realize that suddenly we are doing the impossible; integrating these vital principles as standard care in rehabilitation.
Please join us in White Plains, NY March 31-April 1, 2017 for Nutrition Perspectives for the Pelvic Rehab Therapist. Whether you are just beginning to integrate nutrition and its correlates to pelvic rehab or are already well on your way along this path, you will come away with both a strong understanding of how food affects function along with tools you can immediately begin sharing with the clients you serve.
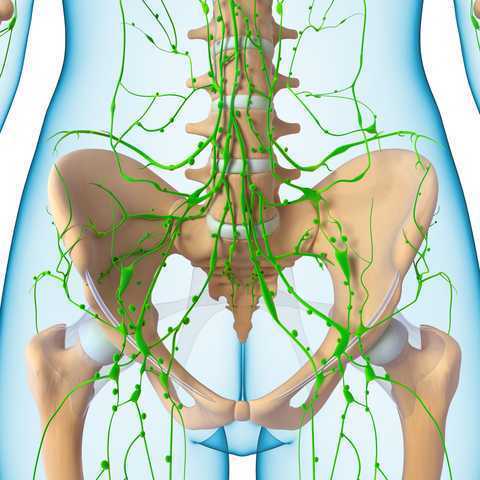
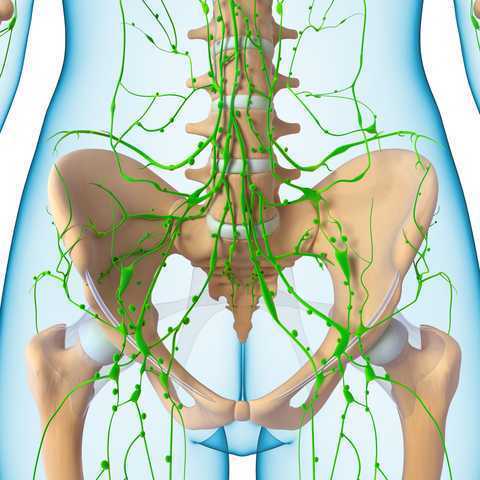 In 1998, faculty member Debora Chassé was asked to evaluate a patient with bilateral lower extremity lymphedema following repeated surgeries for cervical cancer. Her formal education did not cover this in school, so Dr. Chassé began to study peer-review research and consult with other clinicians about the diagnosis. Her journey down the rabbit hole began.
In 1998, faculty member Debora Chassé was asked to evaluate a patient with bilateral lower extremity lymphedema following repeated surgeries for cervical cancer. Her formal education did not cover this in school, so Dr. Chassé began to study peer-review research and consult with other clinicians about the diagnosis. Her journey down the rabbit hole began.
Dr. Chassé became a certified lymphedema therapist in 2000 and a certified Lymphology Association of North America therapist in 2001. She continued training by moving into osteopathy taking her into the direction of lymphatic vessel manipulation. In 2006 she began taking courses in pelvic pain and obstetrics with a focus on pelvic floor dysfunction. It was at this point that Dr. Chasse realized nobody was applying lymphatic treatment to women’s health and pelvic floor dysfunction. In 2009 she became a Board Certified Women’s Health Clinical Specialist in Physical Therapy and began traveling around the United States offering workshops in the area of lymphatic treatment.
Dr. Chassé’s approach is to incorporate all her varied skills in the clinic to produce the best patient outcomes. Debora explains that she is “…showing the similarities between pelvic pain and the lymphatic system. The treatment principles are the same, when you are treating both lymphedema or pelvic pain, you are working to reduce inflammation, pain and scarring.”
Another advantage of the lymphatic treatment approach is that it is more comfortable for the patient. “Most intravaginal techniques causes increased pain and inflammation. However, using lymphatic drainage intravaginally is well tolerated and decreases the intravaginal pain. The results are phenomenal!”
Dr. Chassé recollects her experience with a 21 year old female who suffered from chronic pelvic pain. By applying intravaginal lymphatic drainage techniques for 5 consecutive days, the patient experience a 4.83 reduction in pelvic girdle circumference and her intravaginal pain went from 8/10 to 2/10. The patient was amazed at how much better she felt. “My pants fit better, my energy level increased 25% and pain decreased more than 50%. I went from having 2-3 bad days per week to having 2-3 bad days per month, even when my work level increased. My feet no longer swell and I haven’t missed any classes since receiving this treatment.
In her course, “Lymphatics and Pelvic Pain: New Strategies”, Dr. Chassé seeks to train practitioners to utilize lymphatic drainage techniques when treating specifically pelvic pain. Participants will learn lymphatic drainage principles and techniques. They will learn how to clear pathways to transport lymph fluid and internal techniques which will have incredible impacts for patients.