As pelvic rehabilitation therapists, our role has traditionally focused on restoring continence, alleviating pain, and improving quality of life. Yet within athletic populations, pelvic floor dysfunction often presents in unique and nuanced ways—masked by high levels of conditioning, normalized symptoms, or misattributed pain patterns. As the bridge between performance and pelvic health, we are uniquely positioned to address these challenges.
In athletes, the pelvic floor must do more than support visceral structures or maintain continence. It plays an integral role in force transmission, lumbopelvic stability, breathing mechanics, and reflexive motor control. The demands of sport—sprinting, lifting, jumping, cutting—place high, repetitive loads on the core system, often revealing (or creating) dysfunctions in timing, tone, and coordination of the pelvic floor.
The athletic population requires a different lens: one that views the pelvic floor as a functional component of the kinetic chain and not in isolation.
Clinical Presentations: What We Commonly See
- Stress Urinary Incontinence (SUI) in High-Impact Sports: Female athletes, particularly in gymnastics, track, CrossFit, and volleyball, often experience SUI—yet many have strong pelvic floor muscles on MMT. The issue is frequently one of timing, coordination, or excessive tension rather than weakness. Screening for functional incontinence during movement (e.g., jumping or heavy lifting) is essential.
- Hypertonicity and Myofascial Pain: High-performing athletes often exhibit pelvic floor overactivity—either from compensatory stabilization or stress-related holding patterns. These individuals may present with deep hip pain, dyspareunia, tailbone pain, or abdominal discomfort. Common coexisting findings include labral pathology, SIJ dysfunction, and overuse injuries.
- Core Dysfunction and Lumbopelvic Instability: Poor load transfer across the pelvis, impaired breath mechanics, and delayed transversus or multifidus activation often coexist with pelvic floor dyscoordination. This population may present with chronic low back pain, hip impingement, or even sports hernia.
- Postpartum Athletes: Returning to sport postpartum brings unique challenges—diastasis recti, levator avulsion, prolapse, and deconditioning of core synergy. Pressure to return to performance prematurely can exacerbate dysfunction if pelvic rehabilitation is bypassed.
Assessment Considerations for the Athletic Client
In working with athletes, it’s critical to think beyond isolated internal examination and assess whole-system function:
- Breath and Pressure Management: Assess how the client regulates intra-abdominal pressure during dynamic tasks (e.g., lifting, landing, change of direction).
- Pelvic Floor Mobility and Control: Use internal and external assessments to evaluate both overactivity and under-recruitment, including timing during functional movement.
- Core Integration: Test synergistic recruitment of diaphragm, transversus abdominis, multifidus, and pelvic floor during anticipatory and reactive tasks.
- Functional Movement Screens: Incorporate squat mechanics, running gait analysis, lunge variations, and single-leg stability to evaluate force transfer and pelvic control under load.
- Load Testing: Progress assessments to mimic sport-specific demands—e.g., jumping with pelvic floor biofeedback, agility drills with breath cueing.
Treatment Priorities in Pelvic Rehab for Athletes
- Down-Training Before Strengthening: Many athletic clients do not need Kegels—they need to let go. Releasing hypertonic tissues, restoring breath, and retraining pelvic floor length-tension balance is often the starting point. Re-establishing proper sequencing of breath, pelvic floor, and deep core muscles is essential. Use dynamic cuing, load modulation, and real-time feedback (e.g., pressure biofeedback, US imaging) to reinforce neuromotor control.
- Myofascial and Manual Therapy: Trigger point release (levator ani, obturator internus), neural mobilization (pudendal nerve, obturator nerve), and SIJ or hip mobilizations are often necessary for full pelvic system mobility.
- Functional Reintegration: Rehabilitate pelvic floor activation in context—squatting, lifting, running, jumping. Train coordination across planes of motion, not just in supine or side-lying.
- Athlete-Specific Return-to-Play Criteria: Use objective metrics—continence during max effort, pelvic floor coordination under fatigue, breath control under load—to clear clients for return to sport. Consider incorporating pelvic floor testing into movement screens or performance evaluations.
Our Expanding Role
As pelvic rehab therapists, we are more than continence specialists—we are movement specialists. Within sports medicine, we bring a unique capacity to identify root causes of dysfunction that go unseen by traditional orthopedic approaches. Our collaboration with strength coaches, orthopedic PTs, sports MDs, and athletic trainers is critical in shaping a comprehensive, athlete-centered plan.
Pelvic rehabilitation is a performance tool. In the athletic population, our interventions can prevent injuries, improve performance, and support longevity in sport. By approaching the pelvic floor as a dynamic contributor to the kinetic chain, we can elevate the standard of care and advance our profession’s impact in sports medicine.
The Course Options
Athletes and Pelvic Rehabilitation remote course scheduled for July 26-27. In this course, Dr. Dischiavi covers evidence-based, immediately-applicable skills related to pelvic floor rehabilitation for the athlete, including treatment philosophies for the pelvis and pelvic floor, and global considerations of how these structures contribute to human movement. Topics include urinary incontinence, as well as the intricacies of athletic movement and how energy transference throughout the kinetic chain is crucial to the rehabilitation approach, injury prevention, and high performance. This course will also cover biomechanics behind human movement of the lumbopelvic-hip complex, so the participant will be able to prescribe effective and innovative therapeutic exercise programs. The connection of how pelvic rehab influences LE pathologies such as ACL, PFP, and chronic ankle instability will be covered. Although this class has a focus on athletes, these concepts of biomechanics and movement patterning are applicable to all patients in the clinic.
The Runner and Pelvic Health is a one-day, remote course scheduled for July 26, created and instructed by Aparna Rajagopal PT, MHS, WCS, PRPC, and Leeann Taptich DPT, SCS, MTC, CSCS. This course is designed to expand your knowledge of the pelvic floor in running athletes. Through lecture and labs by video and participation, participants will learn what normal and abnormal running mechanics are and how the muscles work simultaneously during running. This course includes advanced assessments to help diagnose the reason for movement dysfunction. All assessments can be easily integrated into a therapist's evaluation skill set. The course is applicable for patients who present with pelvic pain, incontinence, constipation, prolapse, postpartum, and lumbar pain.
Sarah Hughes PT, DPT, OCS, CF - L2 has been practicing PT since 2007 and opened her private practice, Arrow Physical Therapy in 2016. She now owns and operates Arrow remotely while residing in the Chicago area and practicing at Outlier Physical Therapy. Her specialties include dance medicine, the CrossFit and weightlifting athlete and conditions of the hip and pelvis such as femoroacetabular impingement and labral tears. Dr. Hughes earned a BS in exercise science from Gonzaga University and a DPT from the University of Washington, she wrote and instructs Weightlifting and Functional Fitness Athletes.
Mobility. What is it and how can we get more of it?? In the CrossFit world, athletes can be really fixated on mobility.
- This feels tight.
- That feels restricted.
- I can’t squat below parallel because my ankles are tight.
- I can’t press fully overhead because my lats are locked up.
- I know I just need to foam roll more.
- I’ve been doing this mobility program but I still can’t make progress

Don’t let these athletes fool you. They may be strong and look capable in their functional fitness, but often there is a REASON they feel tight, and it’s not because they need more passive motion. Many CrossFit athletes spend their warm-up time lying on foam rollers, stretching with heavy resistance bands, static stretching, and using percussion guns and other mobility tools.
But, what IS mobility? Mobility is defined as the ability of a joint to move actively through a range of motion. Mobility is about controlling your body through a full range of active movement; much different than passively stretching into a position. And, mobility can only be achieved with strength training, neuromotor retraining, appropriate exercise prescription and PRACTICE. Keep these athletes in your sights as they perform the exercises. Don’t get caught giving them too much freedom to only see you for manual work and then do a home program alone. No online program that they can purchase will ever replace your education and ability to help them with mobility drills.
Are your patients stretching and stretching without the increased mobility they are looking for? Are you doing manual work that is targeted and effective but only getting you so far with them? Try some stability drills and strength training exercises! In the Weightlifting and Functional Fitness Athletes - Remote Course we will look at different CrossFit requirements and what these athletes need. HINT: it's not more foam rolling!!
Weightlifting and Functional Fitness Athletes

Course Dates: March 4, May 13, and October 14
Price: $295
Experience Level: Beginner
Contact Hours: 9
Description: When it comes to Crossfit and Weightlifting, opinions are divided among Physical Therapists and other clinicians. Why is it that these sports cause such strong differences among rehab professionals? In this half-day, remote continuing education course, instructor Sarah Haran PT, DPT, OCS, CF-L2 looks at the realities and myths related to Crossfit and high-level weight-lifting with the goal of answering “how can we meet these athletes where they are in order to keep them healthy, happy and performing in the sport they love?"
This course will review the history and style of Crossfit exercise and Weightlifting, as well as examine the role that therapists must play for these athletes. Common orthopedic issues presented to the clinic will be examined. Labs will introduce and practice the movements of Crossfit and Weightlifting, discussing the points of performance for each movement. The practitioner will not only learn how to speak the language of the athlete but will experience what the movement feels like so that they may help their client to break it down into its components for a sport-specific rehab progression. The goal of this course is to provide a realistic breakdown of what these athletes are doing on a daily basis and to help remove the stigma that this type of exercise is bad for our patients. It will be important to examine the holes in training for these athletes as well as where we are lacking as therapists in our ability to help these individuals. We will also discuss mindset and culture issues such as the use of exercise gear (i.e. straps or a weightlifting belt), body image, and the concept of "lifestyle fitness". Finally, we will discuss marketing our practices to these patients.
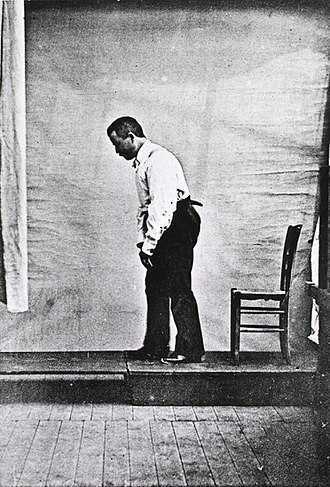
Akinesia is a term typically used to describe the movement dysfunction observed in people with Parkinson disease. It is defined as a poverty of movement, an impairment or loss of the power to move, and a slowness in movement initiation. There is an observable loss of facial expression, loss of associated nonverbal communicative movements, loss of arm swing with gait, and overall small amplitude movements throughout all skeletal muscles in the body. The cause of this characteristic profile of movement is due to loss of dopamine production in the brain which causes a lack of cortical stimulation for movement.
 If the loss of dopamine production in the brain causes this poverty of movement in all skeletal muscles the body, how does the pelvic floor function in the person with Parkinson disease and what should the pelvic floor rehabilitation professional know about treating the pelvic floor in this population of patients?
If the loss of dopamine production in the brain causes this poverty of movement in all skeletal muscles the body, how does the pelvic floor function in the person with Parkinson disease and what should the pelvic floor rehabilitation professional know about treating the pelvic floor in this population of patients?
Let’s take a closer look referencing a very telling article about Parkinson disease and skeletal muscle function. In the Italian town of L’Aquila, a major devastating 6-point Richter scale earthquake occurred on April 6, 2009. 309 people died and there was destruction and collapse of many historical structures, some greater than 100 years old. The nearby movement disorder clinic had been following 31 Parkinson disease patients in the area, 17 of them higher functioning and the other 14 much lower functioning. In fact, of those 14, 10 of them were affected by severe freezing episodes with severe nighttime akinesia requiring assistance with bed mobility tasks, 1 was completely bedridden and the others with major fluctuations in motor performance. 13 of the 14 patients also had fluctuating cognitive functioning.
This devastating earthquake occurred at 3:30 am. All 14 of these patients were able to escape from their homes during or immediately following the event. Caregivers reported that in the majority of the cases, the person with Parkinson’s disease was the first one to be alerted to the earthquake, the first one to get out of the house, ability to alert relatives to run for safety, physically assisting relatives out of the collapsing buildings, and in some cases independently escaping down 1-2 flights of stairs.
Paradoxical kinesia is thought to be the reason for this all but sudden ability to move normally within the presence of an immediate threat to their life and lives of loved ones. Paradoxical kinesia is defined as “a sudden and brief period of mobility typically seen in response to emotional and physical stress in patient’s with advanced idiopathic Parkinson’s disease.” There are a few mechanisms hypothesized to play a role, such as, adrenaline, dopaminergic reserves activating the flight reaction, and compensatory nearby cerebellar circuitry.
There is no pathological evidence that in Parkinson disease there is any break in the continuity of the motor system. The neurologic pathways are all intact and the ability to produce muscle power is retained however requires a strong base of clinic knowledge of the disease to help these patients activate these intact motor pathways. I look forward to sharing the neurologic basis of these deficits in Parkinson disease and strategies in pelvic floor rehab to do just that!
Erica Vitek, a specialist in treating patients with neurologic dysfunction, is the author and instructor of Neurologic Conditions and Pelvic Floor Rehab, taking place September 14-16, 2018 in Grand Rapids, MI.
Bonanni, L., Thomas, A., Anzellotti, F., Monaco, D., Ciccocioppo, F., Varanese, S., Bifolchetti, S., D’Amico, M.C., Di Iorio, A. & Onofrj, M. (2010). Protracted benefit from paradoxical kinesia in typical and atypical parkinsonisms. Neurological sciences, 31(6), 751-756.