
Aparna Rajagopal, PT, MHS is the lead therapist at Henry Ford Macomb Hospital's pelvic dysfunction program, where she treats pelvic rehab patients and consults with the sports therapy team. Her interest in treating peripartum patients and athletes allowed her to recognize the role that breathing plays in pelvic dysfunction. Aparna and Leeann Taptich DPT, SCS, MTC, CSCS co-authored the course Breathing and Diaphragm which helps clinicians understand breathing mechanics and their relationship to the pelvic floor.
The diaphragm is well established as the primary muscle utilized for breathing and as an important contributor to the control of intra-abdominal pressure.
The diaphragm also establishes a myofascial connection from the neck to the foot linking the pelvic floor to the entire body. The diaphragm links the pelvic floor to the ribs, pelvis, hip, and shoulder through the fascia. While a firm definition of fascia is debatable, fascia is a continuum of collagen containing loose and dense fibrous connective tissue that permeates the whole human body effectively connecting one part of the body to another, literally from the head all the way to the toes (1). Fascial tissue contains proprioceptors and nociceptors and changes in fascial tension can influence the function of the musculature that it connects and in turn influence motor control, length-tension relationships, and overall posture (2).
Starting from the top of the head, the neck fascia connects anteriorly to the rectus abdominis through the pectoralis and obliques as well as the endothoracic fascia (2). The deep neck flexors and sternocleidomastoid muscles attach to the hyoid bone and the clavicle connecting the fascia of the chest and abdominal wall (3). The anterior fascial connections continue from the rectus abdominis and obliques through the pubis and pelvic down to the hip flexors and quadriceps.
Posteriorly, the neck is connected to the sacrum through the thoracolumbar fascia which links the upper trapezius, latissimus dorsi, and gluteal musculature (2). Fascia starting at the suboccipital muscles connects down to the hamstrings, gastrocnemius, and plantar fascia (3). Deeper, and posterior, to the thoracolumbar fascia, the endopelvic fascia has a direct connection with the pelvic floor musculature including the levator ani and ischiococcygeus as well as the obturator internus and piriformis (3).
Proper functioning fascia is necessary to ensure good diaphragm and pelvic floor function. Dysfunctional fascia can create altered breathing mechanics and pelvic floor dysfunction that in turn can affect posture, alter walking mechanics, and affect load transfer from the upper to lower body (2).
In the Breathing and Diaphragm course scheduled for March 9-10, 2024 taught by Aparna and Leeann, you will learn to assess and treat myofascial connections from the upper and lower body. Myofascial assessment and treatment will help the clinician link the whole body holistically to the treatment of incontinence, constipation, pelvic pain, low back pain, and breathing pattern disorders.
References:
- Adstrum S, Hedley G, Schleip R, Stecco C. Yucesoy CA. Defining the fascial system. Journal of Bodywork and Movement Therapies. 2017; 21: 173-177.
- Tim S, Mazur-Bialy AI. The Most Common Functional Disorders and Factors Affecting Female Pelvic Floor. Life. 2021; 11: 1397. https://doi.org/10.3390/life11121397.
- Bordoni B. The Five Diaphragms in Osteopathic Manipulative Medicine: Myofascial Relationships, Part 1. Cureus. 2020; 12(4): e7794. https://doi.org/10.7759/cureus.7794.

Erika Darbro PT, DPT, PRPC (she/her) is a Physical Therapist and founder of Envision Pelvic Health & Wellness in Chicago, IL. She graduated with a Doctor of Physical Therapy from Midwestern University in 2017. As a wife and mother of two children, Owen and Adalynn, Erika knows first-hand the need for work-life balance. Active within her professional community, she is a member of both the American Physical Therapy Association and the Illinois Physical Therapy Association. Beyond her clinical expertise, Erika is a weekend warrior playing slow-pitch softball and indoor volleyball. She loves to travel and has a personal goal of visiting all U.S. National Parks. Erika was awarded her Pelvic Rehabilitation Practitioner Certification (PRPC) in November 2020.
Introduction:
My journey into the realm of pelvic rehabilitation began during a clinical rotation in my third year in physical therapy school. It was a pivotal moment that sparked a passion within me to bring about meaningful change in an often overlooked area of healthcare – pelvic health. This blog post delves into why I chose pelvic rehab and the significance of obtaining certification, a decision that has shaped my professional trajectory.
Choosing Pelvic Rehab as a New Graduate:
Upon completing my physical therapy education in 2017, the decision to specialize in pelvic rehab was a natural progression. I was drawn to the prospect of contributing to an area of healthcare that is often shamed and brushed aside. This decision marked the beginning of my commitment to providing patient-centered and holistic care for pelvic health.
Discovering the Need for Inclusive Pelvic Care:
Upon entering the profession, I became acutely aware of the necessity for pelvic health providers who could help individuals of all genders. It was disheartening to hear about patients facing rejection or enduring extended commutes in search of a provider willing to address their concerns, solely because a specific pelvic therapist would not treat their gender. Even in the urban city of Chicago, these situations persisted. This further motivated me to become a resource for these patients, aiming to close the gap in care.
Establishing Envision Pelvic Health & Wellness:
Since graduating, I have worked in various settings, ranging from large chain corporations to an outpatient hospital clinic. While I learned valuable lessons that shaped the provider I am today, I was disheartened to witness a shift from patient-centered care to approaches solely based on metrics. This realization became my 'why' for taking a leap of faith and opening my own private pelvic health clinic in the Fall of 2023. My goal was clear to create a safe and inclusive space where individuals of all genders could receive expert one-on-one care for their pelvic health concerns. This endeavor allowed me to align my professional aspirations with my commitment to breaking the stigma surrounding pelvic health.
The Continuous Journey of Learning:
As a perpetual learner, I recognize the importance of staying up to date with the latest advancements in the field. Each year, I actively participate in numerous continuing education courses, a practice that reflects my dedication to providing the highest quality of care. It was a natural next step to take my commitment a step further by pursuing the Pelvic Rehabilitation Practitioner Certification (PRPC) in 2020.
The Decision to Pursue PRPC Certification:
Choosing to become certified was not a decision made lightly. The PRPC certification stood out as the perfect fit for my clinical ethos – to treat all genders. Unlike some certifications that focus solely on women's health, the PRPC encompasses pelvic health topics for all populations. This alignment with my values was a driving force behind my choice, emphasizing my dedication to being an inclusive pelvic health practitioner.
Expertise and Passion Unveiled:
Obtaining the PRPC certification was not just about acquiring a credential; it was a statement of my commitment to being an expert in the pelvic health field. It serves as a recognition of my passion for treating the pelvic health population and reinforces the idea that I don't merely dabble in pelvic health.
Challenging Myself and Inspiring Others:
The pursuit of certification was also a personal challenge. It pushed me to elevate my skills, deepen my knowledge, and continually evolve as a practitioner. By challenging myself, I hope to inspire other healthcare professionals to embrace continuous learning and strive for excellence in their field.
Impact on Patient Care on my Community:
The impact of my journey extends beyond personal and professional growth. With Envision Pelvic Health & Wellness, I've been able to witness the positive effects of inclusive pelvic care on my patients. I’m fortunate enough to own a practice in the community where I live. This has enabled me to become an active member of the community and create relationships with other health and wellness providers in my area.
Looking Forward:
As I reflect on my journey, I see a future filled with opportunities to contribute to the evolving profession of pelvic health rehabilitation. My commitment to continuous learning, patient-centered care, and inclusivity will remain unwavering.
Conclusion:
In conclusion, my journey into pelvic rehabilitation has been a purposeful and transformative one. From recognizing the need for inclusive pelvic care to establishing my private practice and pursuing certification, every step has been fueled by a passion to make a difference. The PRPC certification symbolizes my commitment to expertise, inclusivity, and continuous growth – values that will continue to guide my journey in pelvic health and contribute to the well-being of individuals across diverse communities.

Faculty member Christine Stewart, PT, CMPT began her career specializing in orthopedics and manual therapy and became interested in women’s health after the birth of her second child. Her course, Menopause Transitions and Pelvic Rehab is designed for the clinician who wants to understand the multitude of changes that are experienced in the menopause transition and how they affect the aging process. To learn more join Christine in her upcoming course scheduled for February 10-11, 2024.
Conversations about menopause are becoming more mainstream. What used to be a taboo subject has thundered into the media in triumphant fashion. Drew Barrymore, Oprah Winfrey, and Maria Shriver are just a few of the celebrities spreading the word about this transition that will affect all menstruating people at some point in their lives. Despite the headlines and increased coverage, most women feel uneducated and underprepared for how this transition will manifest itself in their bodies concerning symptoms and long-term health (Tariq et al., 2023). Pelvic health providers are the perfect people to educate their patients on these changes.
Menopause is defined as twelve months with no menstrual cycle. Once this has occurred, a patient has then entered a post-menopausal state. However, the process of reaching this twelve-month milestone will begin long before menopause is achieved (Lewis 2021). Symptoms are often experienced in the transitional process leading up to menopause, years before it finally occurs. Perimenopause is the precursor to menopause and represents a time when the ovary begins to change. Hormone levels begin to fluctuate which can affect cycle regularity and intensity. Cycles can now occur every three weeks, ovulation can become irregular, and periods can become heavier. When hormones and cycles change, symptoms can begin. Sleeplessness and night sweats before the onset of menstruation can be an early indicator of perimenopause as well as increased anxiety, brain fog, and irritability (Aninye et al., 2021). These changes can begin in patients as early as their late teens but most commonly will occur in the late 30’s and early 40’s. Knowing how to recognize symptoms that can occur during the perimenopause transition can help to educate patients on what is occurring and what they can anticipate as the ovary continues to age.
Genitourinary Syndrome of Menopause is just one of the many conditions that can occur during this time. It is a cluster of symptoms that can be experienced by patients during this transition. Vaginal dryness, dyspareunia, urinary frequency, and urinary incontinence are included in this disorder (NAMS 2022). To better treat these diagnoses, healthcare providers need to ask questions about menstrual regularity and cycle changes in addition to a patient’s bowel and bladder habits. Often, hormones play a role in their urinary and vulvar symptoms. Without understanding this connection, providers are often missing an important piece that could assist in the treatment of genitourinary complaints.
Changes in hormone levels will also impact other systems in the body. As these fluctuations begin, patients can begin to have effects on their cardiovascular system, brain function, and bone health (Aninye et al., 2021). As health care providers, understanding this impact can help to guide patients down a better path of wellness through lifestyle modifications and referrals to physicians specializing in menopause. Basic recommendations on sleep, exercise, and eating habits during this transition can set up a trajectory of better aging and holistic health.
While the prescription of medications is beyond a therapist’s scope of practice, having a thorough understanding of the risks and benefits of these treatments can help educate our patients on their options for symptom management. Understanding their applications in the treatment of symptoms helps to remove societal and medical biases that have existed for over twenty years. It allows for giving patients more informed choices when it comes to their bodies. Women going through menopause are made to think that bearing their symptoms is a rite of passage, yet proper care and consultation can ease these often life-altering effects. Education on options of treatment and appropriate referral is key to empowering patients.
It is never too early or too late to begin a conversation about menopause. Habits and lifestyle in younger people, such as exercise, sleep hygiene, and self-care can have an impact on the changes they will experience later in life. In our post-menopausal patients, these same habits and lifestyle choices can be implemented to assist with improving health outcomes and the aging process. Understanding this transition is key to any healthcare provider treating current or past menstruating people.
As clinicians, we are often the first line of support when it comes to these patients. There is a lack of education for treating this population (Macpherson and Quinton 2022). Knowing the questions to ask can allow for better treatments, healthcare outcomes, and longevity. Patients are hungry for this information but sometimes need encouragement in pursuing treatments and finding solutions with their healthcare team. As pelvic health specialists, this gap can be bridged by providing patients with information regarding their changing cycles and how this can affect their long-term health. This education can change their lives. Let us keep making menopause mainstream.
References:
- The 2020 genitourinary syndrome of menopause position statement of The North American Menopause Society. Menopause, 2020. 27(9): p. 976-992.
- Aninye, I.O., et al., Menopause preparedness: perspectives for patient, provider, and policymaker consideration. Menopause, 2021. 28(10): p. 1186-1191.
- Lewis, R., Why is menopause a priority in primary care?, in Confidence in the Menopause, N.H. Research, Editor. 2021, Fourteen Fish: United Kingdom.
- Macpherson, B.E. and N.D. Quinton, Menopause and healthcare professional education: A scoping review. Maturitas, 2022. 166: p. 89-95.
- Tariq, B., et al., Women's knowledge and attitudes to the menopause: a comparison of women over 40 who were in the perimenopause, post menopause and those not in the peri or post-menopause. BMC Women’s Health, 2023. 23(1): p. 460.

It's been four years since my pelvic floor bestie (fellow Lead TA Carly Gossard) convinced my introverted self to try my hand at teaching assistant. I was hesitant, to say the least. I had taught small lab groups at Stockton University and mentored many of my colleagues in different areas, including pelvic health, but a class of 50 people relying on me to guide them through their first pelvic exam experience…I was terrified. It was the weekend before the world shut down for COVID, so there was this underlying current of “What does the future hold” and “Should we steal the gloves and hand sanitizer?”
Flash forward to the present day. I consider myself so lucky to wear many hats for Herman & Wallace. That first TA experience sparked this love of being with the Level 1 students as they embark on their pelvic health provider journeys. When HW needed to shift to the satellite model, I was one of the first TAs to jump into that role. When Megan Chamberlain (herder of the TAs) asked for help building a Lead TA program, I gave her my list of suggestions (I may consider Leslie Knope from Parks & Rec a role model). One of my favorite things about HW is that they take feedback seriously. At one point, they realized they needed someone to track the patterns of that feedback and guess who got that job….ME!
In 2023, the HW team decided it was time to take that feedback and update the main series to be more…more inclusive, more advanced, more hands-on, more to take home immediately to clinical practice. I was quick to chime in as I had a lot of subjective data from years of review synthesis. We have been organizing, researching, considering, consulting, and revamping the main series, and the first two classes of the series launched in January 2024! As the series rolled out, I decided I needed to TA each class to feel and experience the changes.
I spent January 14th and 15th at Hunter College in NYC with 30+ students during the second run of Pelvic Function Level 1. It went just as amazing as I had hoped as I helped the content team build it. The precourse work laid the foundation for more inclusive providers, reviewed the basics, and set students up to be ready for more advanced and hands-on content in class. There was penile-scrotal anatomy in this course instead of participants having to dive deeper into the pelvic floor series to learn these structures exist. It took about 2 years of my pelvic health career for that to happen in a class for ME! Students came in with more comfort on what they were going to do in person. They also confirmed that the workbook was the thing that hands-on, visual learners dream of. They even noticed we used bigger fonts and included closed captioning.
If you’ve interacted with me at all, through TA experiences, classes, or watching me mic run at HWConnect 2023, you’ll see I’ve come a long way from being the shy wallflower in the back of a PF1. This January, in addition to being one of the teaching assistants for Pelvic Function Level 1 in NYC, I’m also one of the first “TA Takeover” guinea pigs. What does this mean? Probably more videos of me dancing with pelvic organs from iHeartGuts joining the internet! I do hope to show you a little glimpse into what it's like to take a class with HW. In all seriousness though, HW’s goal and mission to bring quality, accessible, and inclusive care to all individuals makes it easy for me to say yes and sign up for any adventure they propose.
Pamela A. Downey, PT, DPT, WCS, BCB-PMD, PRPC is Senior Faculty with Herman & Wallace and is instructing the upcoming Pudendal Neuralgia and Nerve Entrapment scheduled for January 27, 2024. She is the owner of Partnership in Therapy, a private practice in Coral Gables, Florida where she treats women and men with pelvic floor dysfunction, related urogynecological and colorectal issues, spine dysfunction, osteoporosis, and complaints associated with pregnancy and the postpartum period. Her mission is to educate and integrate healthy lifestyles for patients on the road to wellness. Pam sat down with the Pelvic Rehab to discuss her upcoming course.
What makes pudendal neuralgia such a difficult diagnosis to treat?
I think people often see the content in Pelvic Function Level 1 - Introduction to Pelvic Health and it's like a tidy little box. Then you get the patient and as the practitioner you're like I don't know what to do with this person. We need to show that pudendal skills are needed in differential diagnosis. Even though this course is called Pudendal Neuralgia and Nerve Entrapment, it is about differential diagnosis for a lot of pelvic pain. When you feel more secure in knowing what you're treating and have a systematic way of looking at it, then you can be more productive in your patient care.
I think some ortho therapists treat in a linear fashion, and they go from week one to week eight through a protocol and things generally go well because it's a predictable course when you're rehabbing a total knee replacement, or you have an elbow tendonitis, and you expect these structures to follow a path. But then when you come into the nerve side of things, nerves can be unpredictable. They're influenced by lots of factors. It could be your mood. It could be the range of motion around a joint. It could be a previous history of another neurologic problem feeding it, such as disc pathology. It can be something around a postural habit, and it could be a straight up other dysfunction that then affects the pudendal distribution. And if you don't treat the cause of the initial, you will never improve the latter, which is the neurological presentation in pudendal.
I love that it's more about figuring out the differential diagnosis for pelvic pain and going from that angle into pudendal dysfunction, entrapment, neuralgia, and everything that goes with that. For example, you're going to get a patient with an order for pudendal neuralgia, or even worse entrapment. When they get an order for pudendal neuralgia, then they'll kind of forget that the person may not have pudendal neuralgia. They have problems in the pudendal distribution, but that's basically everything we treat. So as a pelvic rehab practitioner they have to tease it out.
When I look at a script I always say, “that's nice.” The referring doctor may have written it as pudendal neuralgia so that the patient could get reimbursement for the therapy with the diagnosis code. But then we get to add our diagnosis codes on top of that and drive a treatment plan.
So, I think that is a big hangup. Practitioners run when they usually see this diagnosis. You don't want a pudendal patient. Especially if you do not have a lot of skills, because you are going to be like, well, what can I do for this patient? If they sit, they have pain. If they exercise, they have pain. They don't have like a whole repertoire. In the pudendal neuralgia course, we talk about how to figure out if the driver is the spine, the hip, the nerve itself, if it's the pelvic floor musculature, or if it's biomechanical. There are so many facets.
How often do these scripts come in for patients that have pudendal neuralgia?
In pelvic pain they're probably coming in a high percentage, like I would say three-quarters. In practice, depending on who's referring into the person's practice, it's going to be a significant amount of walk-in traffic and referred traffic. Because every levator syndrome patient could have a pudendal issue driving the levators, and long-standing levator pain can end up being pudendal.
It's kind of like are you treating the chicken or the egg? I think giving the person skills to do test and retest and having a way to keep falling back on to this and then to also be able to transmit the idea that this isn't a fix -it problem. You know, we just don't put a band aid on it and you're done. Other folks who are more newish, who expect this linear event, they're going to struggle because there's going to be setbacks and sometimes doing more is the exact opposite of what needs to be done. Less is more.
When you look at the H&W course catalog, where would you recommend that practitioners take the Pudendal Neuralgia course?
The sweet spot for taking the pudendal neuralgia course would be practitioners who have taken PF1 and Pelvic Function Level 2A - Colorectal Pelvic Health, Pudendal Neuralgia, and Coccyx Pain, because they learn the rectal canal and PF2A. Practitioners who focus specifically on treating the male pelvic patient would benefit from this course because it is a good thinking course for how to treat men. It could pair well with Pelvic Function Level 2C - Men’s Pelvic Health and Rehabilitation (formerly Male Pelvic Floor). In my practice I get a lot of men coming in because they look on the internet and decide that they got pudenda neuralgia.
If you understand differential diagnosis you can touch on is this a sciatic nerve problem? Is this a genitofemoral problem? We look at the lumbo-sacral plexus in a decision tree, and then we then focus on pudendal and then how people manage them from a medical standpoint and from a therapy standpoint. I talk about using a rule-out method - this could be genital femoral, this could be pudendal nerve. And then you prove what the problem is by doing test and retest.
There's also a lot of pain neuroscience, so practitioners who have taken Pain Science for the Chronic Pelvic Pain Population would benefit from this course. The pudendal neuralgia course goes really well with this course because the practitioners who have taken the pain science course already know that there's going to be ups and downs. Also Nari Clemon’s nerve courses, Lumbar Nerve Manual Assessment and Treatment and Sacral Nerve Manual Assessment and Treatment, are definitely lab -oriented courses and this could be a backgrounder even going into her series, because she's going to talk about a lot of nerve techniques that can be then applied to the pudendal. Nari's courses give solid hands-on skills to deal with nerves, palpation, and finding them. Then this course shows you how to treat them. Not necessarily Pudendal, but all the nerve things. These courses enhance each other. It's like a decision tree where pudendal is on there and you can pass through it and go into Nari’s stuff where you can get a good idea and then use your myofascial, your orthopedic, your neuro skills.

Emily McElrath, PT, DPT, MTC, CIDN is instructing her upcoming course Pregnancy & Postpartum Considerations For High Intensity Athletics scheduled on March 9, 2024. Emily is highly trained in Sports and Orthopedics and has a passion for helping women achieve optimal sports performance and is certified in manual therapy and dry needling, which allows her to provide a wide range of treatment skills including joint and soft tissue mobilization. She is an avid runner and CrossFitter and has personal experience modifying these activities during pregnancy and postpartum.
It’s no secret that high intensity exercise during pregnancy and early postpartum has been debated for years. For many decades, pregnant female athletes have been told things like “you shouldn’t be doing that,” or “that’s not safe.” Are these claims rooted in truth or misunderstanding? I personally think more of the latter, and as it turns out the research supports that as well. In fact, the entire narrative around high intensity exercise in pregnancy seems to be shifting.
In truth, I believe some of the disconnect comes from a lack of understanding of high intensity exercise by clinicians. While many clinicians themselves participate in high intensity exercise, many others do not and also do not understand high intensity exercises like powerlifting, orange theory, crossfit, triathlon training, etc. The other part of the disconnect comes from a general lack of research on the subject. Thankfully, this is also changing and more research is being done on the impact of high intensity exercise on fetal and maternal health, as well as the pelvic floor and core. But up until recent years, we had mostly anecdotal evidence. Finally, we are seeing more and more clinicians being athletes themselves, which has led to a personalized understanding of high intensity exercise during pregnancy and postpartum. Interestingly enough, many of these athlete clinicians are on the frontlines of the current research.
Some of the most recent research that we should highlight includes:
“Clinical and exercise professional opinion of return-to-running readiness after childbirth: an international Delphi study and consensus statement.” This international Delphi survey was published in the British Journal of Medicine and surveyed over 100 clinicians and exercise professionals on readiness to return to running postpartum. They asked these professionals to define “runner” and “postpartum,” what biopsychosocial milestones they felt runners needed to meet, various methods of screening they recommended, supportive items they may recommend, a timeline for when and how to return to running, factors that may contribute to them advising a patient against running, and other educational points they felt were important. At least 75 % of the participants or more felt that, following a minimum 3-week period of rest and recovery, and as long as the patient has met all screening criteria, an individualized return to running progression can be considered.
“Impact of Pelvic Rest Recommendations on Follow-Up and Resolution of Placenta Previa and Low-Lying Placenta.” This retrospective study was published in the Journal of Ultrasound in Medicine in March of 2023 and reviewed 410 pregnancies of women who had placenta previa (144) or low-lying placenta (266). 45% of placenta previa patients and 12% of low-lying placenta patients were placed on pelvic rest. All of the study participants were given an ultrasound at 28 weeks gestation. Resolution occurred in 51% of the placenta previa patients and 75% of the patients with low-lying placenta regardless of whether they were placed on pelvic rest or not. This is exciting because it may indicate that women with placenta previa and/or low-lying placenta previa may not need to be placed on pelvic rest and/or limited from activity.
Another study done by Eichelberger, et al. in the American Journal of Perinatology in 2011 found that 84% of complete placenta previas and 98% of marginal placenta previas resolved naturally by roughly 28 weeks. This study is promising because it shows that while some pregnant athletes may be temporarily limited from exercise, they may be able to return after resolution of the previa.
A study published in 2020 by Chen et al looked at the role of exercise in treating low back pain in pregnancy and found that the transverse abdominis, multifidus, pelvic floor, and diagonal trunk musculature play a significant role in load transfer in the lumbopelvic region. This is important to consider when working with pregnant athletes as we can use these concepts via accessory work to support their tissues for more strenuous activity.
While many of these studies were small, and survey only in nature, it is promising to see more research being done. In the meantime, we have lots of anecdotal evidence that women who were high intensity athletes prior to pregnancy can in fact continue their desired level of exercise confidently and safely. Additionally, when we as clinicians have a thorough understanding of the musculoskeletal system, and how those tissues handle various loads, we can help patients modify as needed to continue loading those structures appropriately and without risk of injury. The goal of my course Pregnancy and Postpartum Considerations For high intensity Athletics is to help give clinicians the confidence they need to work with this patient population. I blend research, clinical experience, and personal experience as a pregnant athlete to help clinicians understand how to meet these athletes where they are to help them continue doing what they love. My mission is to empower women to feel strong, capable, and healthy (mentally, emotionally, and physically) throughout their pregnancy and as they recover postpartum and to change the narrative surrounding high intensity exercise during pregnancy from one of fear and misunderstanding to one of empowerment and encouragement.
Dawn Sandalcidi PT, RCMT, BCB-PMD is a trailblazer and leading expert in the field of pediatric pelvic floor disorders. Dawn is a national and international speaker in the field. In addition to lecturing internationally on pediatric bowel and bladder disorders, You can join Dawn Sandalcidi with HW in her courses, Pediatrics Level 1 - Treatment of Bowel and Bladder and Pediatrics Level 2 - Advanced Pediatric Bowel and Bladder Disorders. Her next HW course, Pediatrics Level 1, is scheduled for February 3-4 and still has seats available for registration.
In the realm of pediatric pelvic health, the issue of urinary and fecal leakage is a subject that demands a nuanced understanding. Too often, these incidents are dismissed as mere "accidents," inadvertently subjecting children to shame and stigma. It's crucial to recognize that in many cases, children are grappling with conditions such as enuresis and encopresis, which are not behavioral issues or mistakes but rather manifestations of underlying health issues. In this blog, we'll explore the issue of the most common pediatric bowel and bladder disorders, the challenges faced by both parents and healthcare professionals and the need for a holistic approach to treatment.
Understanding the Scope of Pediatric Incontinence
Enuresis and encopresis are clinical terms used to describe involuntary urine and fecal leakage, respectively, in children beyond the age when such control is typically expected. Contrary to common misconceptions, these occurrences are not the result of a child's intentional mistake. Instead, they often signal underlying physiologic disturbances as well as pelvic floor and core dysfunction, which can have wide-ranging effects on a child's physical and psychological well-being.
Causes of enuresis and encopresis can vary, encompassing a range of physical and psychological factors. In many cases, these conditions are linked to pelvic floor dysfunction and bowel issues such as constipation. However, other contributing factors may include genetic predispositions, neurological issues, hormonal imbalances, and emotional stressors. Traditional approaches, such as the outdated notion of letting a child "grow out of it," fail to recognize the multifaceted nature of these conditions. Such passive strategies not only prolong the child's suffering but also perpetuate societal misconceptions around pediatric incontinence — ” What’s ‘wrong’ with these kids?”. Truly, nothing is “wrong”, except that children aren’t granted the access they need to professionals equipped to help. It is imperative to replace such antiquated views with informed, proactive approaches that address the root causes of enuresis and encopresis, providing children with the support and interventions they need to thrive.
Enuresis and Encopresis: Current Challenges
Only about 15% of children per year will organically “outgrow” bedwetting. This statistic underscores the prevalence of the issue and highlights the need for a compassionate and informed approach. Many children experiencing urinary and fecal leakage endure shame, embarrassment, and self-esteem issues, leading to internalizing and sometimes externalizing psychological behaviors.
Parents and healthcare workers encounter formidable challenges when confronted with pediatric incontinence. Beyond the inherent complexities of addressing the physical and emotional well-being of affected children, navigating the healthcare landscape presents additional hurdles. The prevailing societal perception that dismisses these incidents as mere "accidents" contributes to the challenges parents and healthcare professionals face. One of the primary obstacles is the scarcity of trained healthcare providers specializing in pediatric pelvic health. Locating professionals with the expertise to address the nuanced complexities of enuresis and encopresis can be a daunting task, often resulting in delayed or inadequate care.
Moreover, time constraints faced by healthcare providers pose another significant challenge. Parents seeking assistance often find themselves struggling to locate professionals who not only possess the necessary expertise but also have the time to listen attentively to their concerns. In a system where healthcare practitioners are stretched thin, the need for personalized attention and understanding of the intricate nature of pediatric incontinence can be overlooked.
Navigating the intricate web of insurance and referral systems exacerbates the situation. Healthcare workers often grapple with bureaucratic hurdles that can impede the timely access of patients to necessary interventions. Delays in appointments due to administrative complexities not only prolong the child's suffering but also add to the stress experienced by both parents and healthcare providers.
Furthermore, the societal misconception surrounding pediatric incontinence compounds the emotional burden on families. The prevailing notion that these incidents are either behavioral or somehow otherwise the fault of the child contributes to a culture of silence, making it challenging for parents to seek support and understanding from their social circles. The stigma associated with pediatric incontinence can lead to feelings of isolation and shame, inhibiting open discussions about the challenges faced by affected children and their families.
In light of these challenges, it becomes evident that addressing pediatric incontinence requires a multi-faceted approach. Dawn Sandalcidi, a trailblazer and seasoned practitioner in pediatric pelvic health, emphasizes that these issues go beyond the pelvic floor. Children with pelvic floor dysfunction often present with ribcage and core dysfunction, necessitating a broader perspective in treatment. Without a “how-to” manual, Dawn tackled these issues head-on. She incorporated her decades of clinical experience and developed coursework such that other practitioners in the United States (and around the world!) can more easily access effective training on how to treat the pediatric pelvic floor.
Efforts should be directed not only toward enhancing the availability of trained healthcare professionals but also toward dismantling societal misconceptions and streamlining administrative processes. By fostering a more supportive and informed environment, we can empower parents, healthcare workers, and, most importantly, the children affected by enuresis and encopresis to navigate the intricate landscape of pediatric pelvic health with resilience and understanding.
A Holistic Approach to Pediatric Pelvic Health
Dawn Sandalcidi's courses offer a comprehensive understanding of pediatric pelvic health. Pediatrics Level 1 - Treatment of Bowel and Bladder Disorders covers the basics of pediatric pelvic floor anatomy, physiology, and voiding reflexes. Biofeedback and ultrasound techniques provide less invasive alternatives for children. Pediatrics Level 2 - Advanced Pediatric Bowel and Bladder Disorders expands the focus beyond the pelvic floor, examining the entire musculoskeletal system in more complex cases, offering evaluation and treatment techniques that “zoom out” to look at the whole child.
Acknowledging that children don't comprehend pain in the same way as adults, a biopsychosocial approach is essential. The incorporation of enjoyable elements makes the treatment process more accessible for young patients.
It's time to shift the narrative around pediatric incontinence. Labeling these incidents as accidents not only oversimplifies the complex challenges children face, but lends to an environment where children aren’t able to truly heal - not just physically, but mentally and emotionally as well. Dawn Sandalcidi's expertise underscores the need for practitioners to view pediatric pelvic health holistically, and to move toward a trauma-informed approach. By understanding the interconnectedness of pelvic and full-body musculoskeletal health and adopting innovative treatment approaches, we can empower both children and their families to navigate the complexities of pediatric incontinence with compassion and understanding. Let's move beyond the 'accident' label and foster an environment where children feel supported, not ashamed, in their journey to health and well-being.

Rachna Mehta, PT, DPT, CIMT, OCS, PRPC, RTY 200 is the author and instructor of the Acupressure for Optimal Pelvic Health course. Rachna brings a wealth of experience to her physical therapy practice and has a personal interest in various eastern holistic healing traditions.
A Holistic Self-Regulation practice
A patient smiled at me as I gathered her history at the clinic, and declared in a resounding voice:
“I am a Type A personality honey! I have never been able to relax so good luck trying to relax me !!!”
As we went over her history and medical review, the word “anxiety” popped up several times within fifty-plus years of mental and physical abuse, PTSD, insomnia, and chronic stress. She is a retired nurse now in her late 70s presenting with urinary incontinence. She knew all her medications with the exact doses memorized yet she couldn’t remember the last time she had slept through the night. Chronic anxiety pervaded every aspect of her life, and she didn’t know how to relax her mind, much less relax her bladder or pelvic floor muscles. Every time she got anxious, she clenched every part of her body.
Over the years I have seen so many of these patients in my clinical practice and besides the medications, most of them were looking and trying holistic treatment options. Some of my patients were also doing Acupuncture and Yoga and the question that always came back to me was what they could do themselves to get better. These patients sparked my interest in holistic Complementary & Alternative Medicine (CAM) therapies. I knew that teaching them self-regulation skills would be the key to addressing their musculoskeletal impairments successfully.
In addition to teaching her a home program that included pelvic girdle stretches, pelvic floor relaxation, bladder training, and behavioral modifications, I also taught her two key Acupressure points Central Vessel 17 ( CV 17 ) and Yintang (EX-HN 3) for breathing, calming and self-regulation. CV17 is located at the center of the chest while Yintang (EX-HN 3) is located between the eyebrows and is known to have a mentally stabilizing effect in Traditional Chinese Medicine (TCM). Within a few minutes of applying gentle Acupressure to these points, the patient felt calmer and more relaxed. Over the course of her program, we continued to address musculoskeletal impairments, fascial restrictions, and also started strengthening her pelvic floor muscles.
Along with this standard program, the patient was also taught a self-regulation Acupressure home program on how to relax her mind and body using potent Acupressure points in the Kidney, Bladder, Stomach, Spleen, Heart, and Pericardium meridians. The Bladder meridian with 67 Acupoints is the longest meridian in the human body and of these, there are 16 Acupoints located on the sacrum that are the key to addressing both bowel and bladder dysfunctions. 6 visits later this patient improved from using 3 pads per day to no pads, she had minimal symptoms of incontinence with good mind-body-bladder control, and she came to rely on these self-Acupressure points to tackle daily stressors to be in a calmer state of mind.
Acupressure is a type of Acupuncture in East Asian traditional medicine or integrative medicine that involves the application of pressure to specific points (i.e., Acupoints) or specific areas of the body using one’s hands or other Acupressure devices (Kwon et al). Acupressure has been used in Traditional Chinese Medicine for over 3000 years and is based on Meridian theory.
Emerging research shows that these Acupoints are embedded in a three-dimensional fascial network throughout the body and have a high electrical conductivity on the surface of the skin. Histological studies show a high density of A and C afferent fibers at these points. Through a vast network of interstitial connective tissue, these Acupoints connect the peripheral nervous system to the central viscera.
Studies also show that Acupressure has also been used widely to alleviate symptoms of anxiety like anxiety tics. One of the key applications of Acupressure has been the use of Acupoints in Emotional Freedom Techniques (EFT). EFT is an “evidence-based” therapeutic method. It combines elements of cognitive and exposure therapy with Acupressure. It is popularly termed “tapping” because its distinguishing feature is the stimulation of acupuncture points using fingertip percussion. EFT tapping itself has been used in Chinese medicine, Japanese massage, qigong, and yoga for thousands of years (Church et al).
EFT has also been shown to be effective in addressing emotional challenges such as Anxiety, depression, burnout, stress management, and fears. The basic principle of EFT is to send activating and deactivating signals to the brain by stimulating points on the skin that have distinctive electrical properties, usually by tapping on them. These points correspond with the Acupressure points that in Traditional Chinese Medicine are believed to regulate the flow of the body's energies4.
Acupressure uses the same points as Acupuncture and is a non-invasive, low-cost, and efficient CAM therapy to alleviate Anxiety and pain. Acupressure involves the application of pressure to points located along the energy meridians of the body. These Acupoints are thought to exert certain psychologic, neurologic, and immunologic effects to balance optimum physiologic and psychologic functions (Monson et al). Acupressure can also be used for treating a variety of pelvic health conditions including Chronic Pelvic Pain, Dysmenorrhea, Constipation, digestive disturbances, and urinary dysfunctions to name a few.
As healthcare providers, we can incorporate holistic self-regulation tools into our clinical practice to improve the efficacy of our rehabilitation interventions. We can empower our patients by giving them the tools and self-care regimens to live healthier anxiety-free lives.
The course Acupressure for Optimal Pelvic Health is curated and taught by Rachna Mehta. It explores Acupressure and Yin Yoga as powerful integrative practices and offers unique evidence-based self-regulation tools in the realm of energy medicine. To learn how to integrate Acupressure into your practice, join the next scheduled remote course on February 3-4, 2024.
References:
- Kwon CY, Yeh CH. Use of Information and Communication Technologies to Enhance Self-Acupressure: a Literature Review. J Acupunct Meridian Stud. 2022;15(4):214-226. doi:10.51507/j.jams.2022.15.4.214
- Mehta P, Dhapte V, Kadam S, Dhapte V. Contemporary acupressure therapy: adroit cure for painless recovery of therapeutic ailments. J Tradit Complement Med 2016;7:251-63. https://doi.org/10.1016/j.jtcme.2016.06.004.
- Kwon CY, Lee B. Acupuncture or Acupressure on Yintang (EX-HN 3) for Anxiety: A Preliminary Review. Med Acupunct. 2018;30(2):73-79. doi:10.1089/acu.2017.1268
- Church D, Stapleton P, Vasudevan A, O'Keefe T. Clinical EFT as an evidence-based practice for the treatment of psychological and physiological conditions: A systematic review. Front Psychol. 2022;13:951451. Published 2022 Nov 10. doi:10.3389/fpsyg.2022.951451
- Monson E, Arney D, Benham B, et al. Beyond Pills: Acupressure Impact on Self-Rated Pain and Anxiety Scores. J Altern Complement Med. 2019;25(5):517-521. doi:10.1089/acm.2018.0422
- Chen SR, Hou WH, Lai JN, Kwong JSW, Lin PC. Effects of Acupressure on Anxiety: A Systematic Review and Meta-Analysis. J Integr Complement Med. 2022;28(1):25-35. doi:10.1089/jicm.2020.0256

Ramona Horton, MPT, DPT developed and instructs the visceral and fascial mobilization courses for HW and presents frequently at local, national, and international venues – including International Pelvic Pain Society, CSM and HWConnect - on topics relating to women’s health, pelvic floor dysfunction, and manual therapy. Join Ramona in her upcoming course, Mobilization of the Myofascial Layer: Pelvis and Lower Extremity this February 2-4, 2024.
1. Learn from Ramona Horton!
Ramona C. Horton MPT, DPT serves as the lead therapist for her clinic’s pelvic dysfunction program in Medford, OR. Her practice focuses on treating adults and children with urological, gynecological, and colorectal issues. Her PT career began in the US Army, and she has taken the military “mission first” mentality into her approach to patient care. Simply said, “Diagnosis is just a label, perform a comprehensive musculoskeletal evaluation and treat what you find”. For her many contributions to the field of pelvic health, Ramona was awarded the prestigious Academy of Pelvic Health Elizabeth Noble Award in 2020.
2. The myofascial course is a concepts course.
The whole idea of the myofascial course is to help clinicians learn to problem-solve. To learn some basic concepts of physiology and mobility testing to stop chasing the boo-boo, and instead find and treat the cause. Just because it hurts at the right SI joint, doesn’t mean that you should treat the right SI joint. Joint hypermobility is profoundly nociceptive, especially in a one-bone/two-joint scenario as the sacrum and SI joints. Consider the idea that pain may be generated on the right from hypermobility that is a result of hypo-mobility on the left. Which side should then be treated, the painful side or the stiff side? Let’s treat where the brain is protecting and guarding the tissue.
3. Understand the true function and mechanisms of manual therapy.
Manual therapy is presented as a concept and technique that does NOT “release” tight or bound fascia based on the skill or magic hands of the practitioner. The issue is not in the tissue, if the tissue is tight, it’s tight because the brain is keeping it that way. Muscles are marionettes, and the brain is the puppet master. Manual therapy utilizes the fascial system to access the nervous system. In other words, having a conversation with the brain over the tissue that it appears to be protecting while trusting that the homeostatic mechanism is functioning in the body. If this is done in a non-threatening manner, the brain will normalize the tissue it is holding and guarding.
4. Add a whole host of new tools to your practitioner toolbelt.
The myofascial course teaches basic screening techniques that will point you in the right direction toward finding where the body is protecting, not where symptoms are being expressed. You will learn a variety of techniques to approach different fascial layers including direct and indirect fascial stacking for superficial nerves within the panniculus, muscular, and articular restrictions, as well as indirect technique of positional inhibition for trigger points. In addition, the science behind basic neural mobilization, instrument-assisted fascial mobilization and fascial decompression (cupping) are presented.
5. Learn more about fascia, its origins, and its functions.
Fascia is EVERYWHERE throughout the body; it is the ubiquitous connective tissue that holds every cell together much like the mortar in a brick wall, in addition to cells, it connects every system in the body. Fascia contains a vast neurological network including nociceptors, mechanoreceptors, and proprioceptors just to name a few. The fascial system has multiple layers within the body: starting at the panniculus which blends with the skin, the investing fascia surrounding muscles and forming septae, the visceral fascia which is by far the most complex and the deepest layer of fascia, the dura surrounding the central nervous system extending to the peripheral nerves. All fascial structures, regardless of layer or location have their origin in the mesoderm of early embryologic development. The myofascial course presents evaluation and treatment techniques for three of the four fascial layers while the three visceral courses address the complex visceral fascial layer.
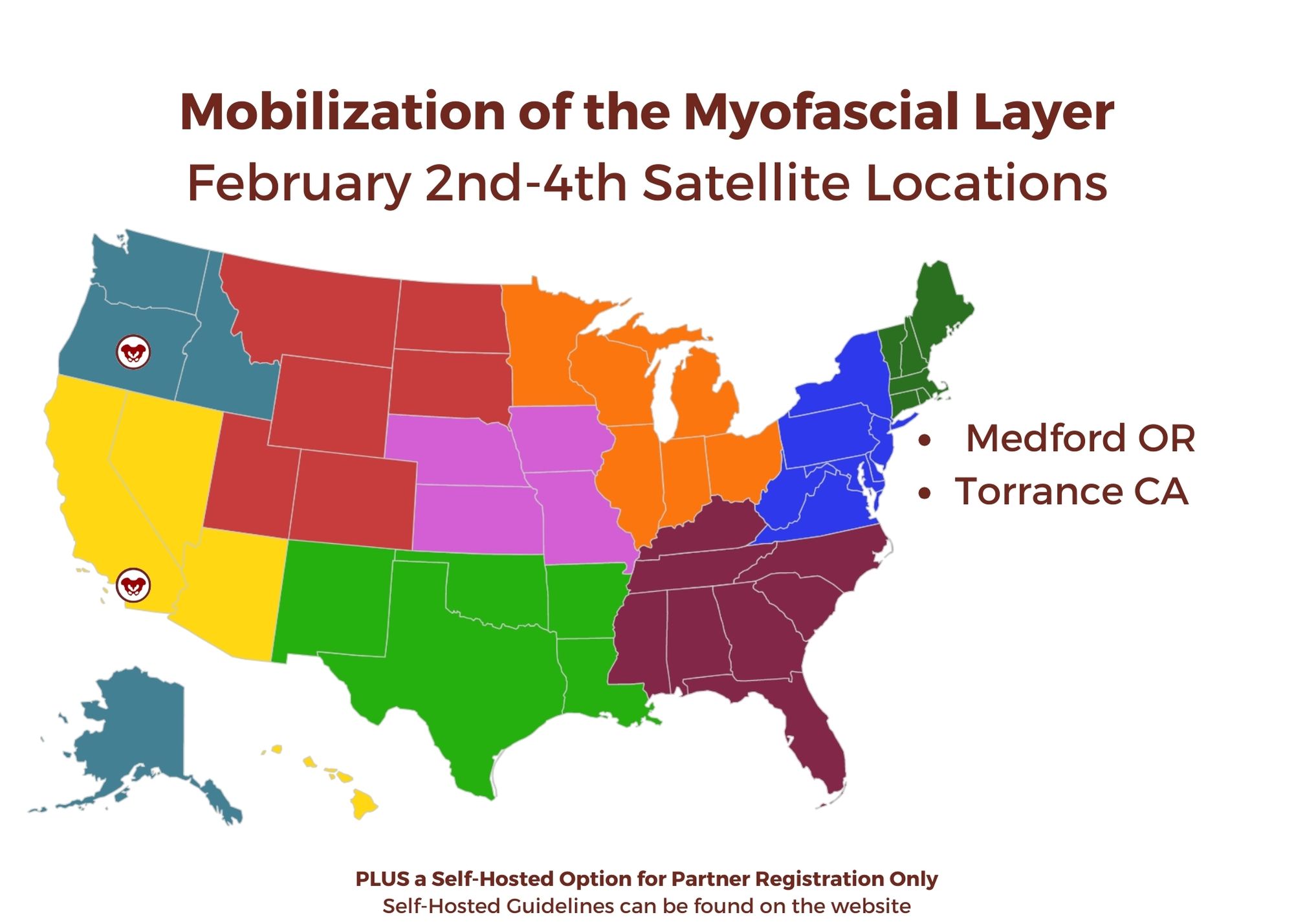
Mobilization of the Myofascial Layer: Pelvis and Lower Extremity
February 2-4, 2024
Price: $675
Experience Level: Intermediate
Contact Hours: 22.5
Medford, OR Satellite
Torrance, CA Satellite
Self-Hosted
HW Looks forward to seeing you in a future course!
We are pleased to announce the following changes and additions to our core series of courses. These changes are being undertaken by our Curriculum Development Team based on evolving realities of our field and the body of evidence and literature. In keeping with the way the field has evolved, we will be making the following changes to our core coursework.
Two courses will be joining our Pelvic Function Series:
- Pelvic Function Modalities - This brand new course is an in-person two-day continuing education course targeted to pelvic health clinicians covering frequently used modalities in pelvic health, including biofeedback and EStim. Hands-on labs using a variety of equipment necessitate that this course be offered in-person, where participants can practice using the equipment.
- Pelvic Function Level 2C: the Male Pelvic Floor and Men’s Pelvic Health - formerly the stand-alone course, Male Pelvic Floor Function Dysfunction and Treatment, this course is now being adapted and reformatted to be a part of the Pelvic Floor Series, reflecting the inclusive stance of H&W core series instructing in the care of all patients. This course will be offered as satellite, self-hosted, and in-person options in order to provide the most flexible pathway for participants.
In addition to these two new offerings, you will see greater inclusion of all genders throughout the series, starting with PF1. The modified titles and topics will be as follows:
Pelvic Function Level 1: Introduction to Pelvic Health - this course will provide a thorough and comprehensive introduction to anatomy and physiology of the pelvis and surrounding structures in all genders. Includes an introduction to performing intra-vaginal exam. This course will be offered in satellite and in-person formats.
Pelvic Function Level 2A: Colorectal Pelvic Health and Pudendal Neuralgia, Coccyx Pain. In labs, anorectal internal exam will be introduced. This course will be offered in satellite and in-person formats.
Pelvic Function Level 2B - Urogynecologic Topics in Pelvic Health. This course will be offered in satellite, self-hosted and in-person formats
Pelvic Function Series Capstone - Integration of Advanced Concepts in Pelvic Health. This course will remain targeted to the advanced clinician. A greater emphasis on workshopping clinical case studies will be incorporated. This course will be offered in satellite, self-hosted and in-person formats.
Questions:
What courses will be required in order to advance to the Capstone course?
As we understand the “advanced pelvic floor clinician” may have a variance of experience and focuses, the following course “journeys” can all be taken in order to take the Capstone course:
PF1
PF2A
P2B and/or PF2C
The Modalities course is strongly recommended, but not required, in order to take the Capstone course.
Why is the series being expanded and updated in this way? .
It is a reality of our field that pelvic rehab evolved from a tradition of “women’s health physical therapy”, and that is reflected in the vulvovaginal emphasis of the current coursework. As the scope of pelvic rehab has expanded to encompass men’s health and care for all genders, it is important that all pelvises be incorporated at every level of our series, and that men’s health be a foundational part of our curricula, rather than being siloed as a specialty offering.
I have already started my PF series coursework, where do I go now?
If you have taken only PF1, you should advance to PF2A, 2B or 2C in any order. You may also wish to take the Modalities course in order to learn evidence-based use of modalities and practice biofeedback and Estim in a hands-on, in-person setting. The best way to choose which course to take next will be determined by who shows up in your clinic after completing PF1 and beginning to see your first pelvic patient caseload.
If you have taken PF1 and 2A - take either 2B or 2C or both in any order to advance to Capstone. If you took PF1 following the pivot to the satellite model, you may also wish to take the Modalities course in order to practice hands-on biofeedback and Estim labs.
If you have taken PF1 and 2B, you must take 2A prior to Capstone. You may take the 2C course to learn men’s health topics if seeing male and male-identifying patients is part of your clinical goals. If you took PF1 following the pivot to the satellite model, you may also wish to take the Modalities course in order to practice hands-on biofeedback and Estim labs
If I have taken PF1, 2A, and 2B - you may advance to Capstone or you may take the 2C course to learn men’s health topics if seeing male and male-identifying patients is part of your clinical goals. If you took PF1 following the pivot to the satellite model, you may also wish to take the Modalities course in order to practice hands-on biofeedback and Estim labs
If you have taken PF1, 2A, 2B and Capstone but have not taken the former Male Pelvic Floor course, you may take the 2C course to learn men’s health topics if seeing male and male-identifying patients is part of your clinical goals.
If you have taken PF1, 2A and the Male Pelvic Floor course, you may advance to Capstone
If you have taken PF1, 2A, 2B and the Male Pelvic Floor course, you may advance to Capstone
Am I required to take more courses in order to complete the PF series now?
No. Previously, there were three prerequisite courses for taking the advanced Capstone course: PF1, 2A and 2B. Following the changes to the series, the prerequisite courses for taking Capstone will be PF1, 2A and 2B OR 2C (or both, depending on one’s target patient population). The Modalities course is a strongly encouraged, but not required, level of the PF series.
As before, participants should choose their next course based on the patient needs they are seeing in the clinic. Following PF1, many may see patients with fecal incontinence or coccyx pain and may choose to prioritize PF2A as the next step in their journey. Others may see patients with penile pain or incontinence post-prostatectomy and may choose to take 2C as their next step.
As before, there are no required courses in order to sit for the Pelvic Rehab Practitioner Certification Exam.
Why aren’t there self-hosted options for PF1 and PF2A?
PF1 is most learners’ first introduction to performing intra-vaginal assessment and therefore we believe the best learning experience will be under the guidance of either an HW faculty member or trained teaching assistant at an in-person or satellite course. Similarly, PF2A is most learners’ first experience performing anorectal exam, which should also take place under the supervision of an experienced clinician. In PF2B, 2C, and Capstone, these techniques are refined and it is therefore appropriate to allow self-hosted options for those who have already learned these skills and are comfortable with independent learning.
I see that there will be options for a few in-person as well as satellite offerings for much of the series. Will HW continue to offer both formats?
We understand that many people appreciate the flexibility and accessibility of the satellite model as an improvement over the days when all series courses were sold out with long waitlists and lengthy travel was often required to attend our courses. We also understand that some folks simply prefer the format in which instructors are present at the course. Our intention is to offer formats that accommodate everyone’s needs, which is why the PF series will be available in-person as well as in the satellite format starting in 2024. Because of the hands-on equipment needs of the Modalities course, this will be available exclusively in person.
Why is PF1 required for 2C if it wasn't for MPF?
Historically, the Male Pelvic Floor course was a stand-alone course, meaning that many participants would take this course after beginning their journey with PF1 and after already seeing patients with pelvic floor dysfunction. Others, often male and male-identifying practitioners who did not feel their goals were met by the vulvovaginal-centered PF series, would take the Male course as their first ever introduction to pelvic health. This resulted in course attendees being in vastly different places in terms of experience, which often results in a sub-optimal learning experience for all.
As part of our push to see more information about patients of all genders incorporated at every level of the core series, PF1 which contains foundational information on all pelvises and core concepts in pelvic rehab, will be a prerequisite for 2C, which will build on those core concepts as they apply specifically to the male and male-identifying patient.
Who can act as a Teaching Assistant for the series courses in the new format?
PF1 - must have PF1, and ⅔ of the Level 2s (2A, 2B, and 2C)
PF2A - must have 1, 2A, and 2B or C
PF2B - must have 1, 2B
PF2C - must have 1 and have taken the Male Pelvic Floor in 2016 or later
Capstone - must have 1, 2A, 2B or 2C, and Capstone
By accepting you will be accessing a service provided by a third-party external to https://www.hermanwallace.com/










































