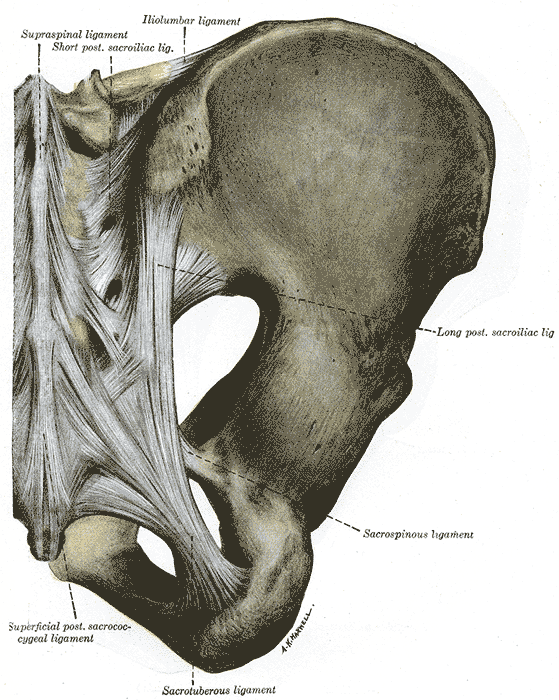
You’ve done a thorough evaluation of the lumbar spine. You’ve done all the special tests for hip pathology, but something is missing. Of course it could be a pelvic floor issue, but what else? Think about the middle child who gets ignored even if making a commotion or goes unnoticed unless being tripped over when standing still. Perhaps the missing link to your patient’s dysfunction is the sacroiliac joint, that “in between” area. If you are unsure how to assess and deal with the “middle child,” learning more about Sacroiliac Joint and Evaluation is something to add to your professional bucket list.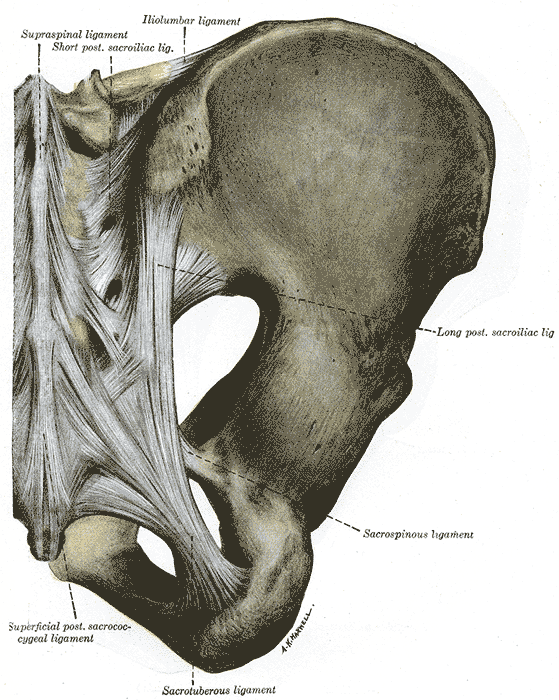
According to the special tests book by Chad Cook, a pain mapping test suggests a referral pattern of SI dysfunction as pain in the buttock unilaterally, below the level of L5, without symptoms in the midline. Often we are on a mission to make the lumbar spine the source of symptoms, but this provides some guideline as to where the pain would be located if the SI joint were the guilty party. If pain is found above L5, the SI joint is likely not the primary tissue in lesion. If the pain is bilateral, the issue is more than just SI joint.(Cook, 2013)
The special tests to diagnose SI joint dysfunction have been considered in a cluster. According to Laslett, distraction, compression, thigh thrust, Gaenslens, and Patricks are the primary tests used to assess SI dysfunction. Three or more of these tests being positive can help a clinician rule in SI joint as a diagnosis, with SI joint blocks being just as predictive. When pain cannot be centralized, and three of the tests are positive, there is a 77% probability the SI joint is the source of pain; and, in the pregnant population, there is an 89% chance the SI joint is the culprit of pain.(Laslett, 2008)
While parents keep up with the oldest and youngest, the middle child can be hard at work causing dysfunction that disrupts the whole family. Likewise, the sacroiliac joint can be hypermobile, hypomobile or have ligamentous strain, yet we therapists may ignore any signs until the lumbar spine or hip or pelvic floor are suddenly provocative. The longer an SI joint dysfunction goes undiagnosed and untreated, the greater the likelihood of pelvic floor dysfunction, secondary to its intimate relationship to the area. A catawampus ilium position on the sacrum can cause hip pain, and the ilium’s relationship to the sacrum can aggravate the lumbar spine. We just need to use all our diagnostic tools to discern what is making our patients symptomatic and then prioritize the treatment.
Taking the upcoming sacroiliac course through Herman Wallace (Sep. 12-13 in New Orleans) will make the “middle child” become respected, understood, and never left wanting again. Review the anatomy, explore and proficiently perform the special tests, and effectively implement treatment and stabilization of the SI joint during this course. You owe your patients the ability to understand the lumbar region and pelvic ring in their entirety and leave no source of pain a mystery.
References:
Cook, C., & Hegedus, E. (2013). Orthopedic physical examination tests: An evidence-based approach. Upper Saddle River, N.J.: PearsonPrentice Hall.
Laslett, M. (2008). Evidence-Based Diagnosis and Treatment of the Painful Sacroiliac Joint. The Journal of Manual & Manipulative Therapy, 16(3), 142–152.
A recent systematic review published in The Lancet online describes the benefits of using music as a postoperative aid in recovery. Seventy-three randomized, controlled trials were included in the review, and the articles covered the use of music before, during, and after surgery. A wide variety of surgical procedures were represented in the research articles, and included cardiac procedures, mastectomy, urogynecologic and abdominal surgeries, and gastrointestinal surgeries and procedures. Interventions included listening to music with headphones, listening to relaxation training or “therapeutic suggestion.” Many of the studies included a control group with routine care or white noise, headphones without music.
The main results of the research is that use of music reduces postoperative pain, anxiety, and analgesia use, and improves patient satisfaction. The timing of or choice of music listened to in the studies did not significantly affect outcomes. Interestingly, even when patients were given general anesthesia, music was effective. And when patients chose their own music, there was a slight increase in reduction of pain and analgesia use.
How can this information be of use to pelvic rehabilitation providers? Perhaps one of your patients will be heading into surgery. A recommendation for listening to favorite music in the postoperative period could be made. Is music available to your patients in your setting? If so, what kind of music? Is the patient allowed to influence the type of music? Maybe the patient could play a favorite song list from their smart phone, or request a certain time period of music on a music subscription service you may use in the clinic. Regardless of how we use this information, it’s great to be reminded of the potentially positive ways that music can influence healing.
National Public Radio (NPR) recently posted a story on their website that you can listen to if you are interested. For more interesting reads about music and healing, check out the links below:
Psychology Today: Does Music Have Healing Powers?
Scientific American: Music Can Heal the Brain
 We know that many of our patients who struggle with severe pelvic pain need rehabilitation efforts directed towards quieting of the nervous system. In general, activation of the parasympathetic system is a goal, with targeted physiologic improvements in heart rate, respiration, and blood pressure, for example. Many providers are teaching patients physiologic quieting techniques such as breathing, mindfulness strategies, visualization, meditation, and encouraging activities like yoga. Does yoga really affect the nervous system? To assess the ability of yoga to increase cardiac parasympathetic nervous system modulation, a study published in Evidence-Based Complementary and Alternative Medicine examined the effects of yoga practice on physiologic variables.
We know that many of our patients who struggle with severe pelvic pain need rehabilitation efforts directed towards quieting of the nervous system. In general, activation of the parasympathetic system is a goal, with targeted physiologic improvements in heart rate, respiration, and blood pressure, for example. Many providers are teaching patients physiologic quieting techniques such as breathing, mindfulness strategies, visualization, meditation, and encouraging activities like yoga. Does yoga really affect the nervous system? To assess the ability of yoga to increase cardiac parasympathetic nervous system modulation, a study published in Evidence-Based Complementary and Alternative Medicine examined the effects of yoga practice on physiologic variables.
Cardiac vagal modulation was the primary variable assessed in this study; ambulatory 24-hour Holter monitoring, with heart rate variability (HRV) identified hourly by a blinded observer, was the method used to collect data. (The authors explain that this is an established tool to measure HRV, and that HRV can be used as a predictor of cardiac mortality and sudden cardiac death.) Eleven healthy yoga practitioners (4 men and 7 women) completed 5 sessions of training. All of the subjects had at least 3 years of experience practicing Iyengar yoga, and some of the subjects were certified Iyengar instructors. During 2 of the sessions, subjects were trained for 90 minutes, once per week, for 5 weeks. During 2 of these sessions, the subjects practiced a yoga session developed by B.K.S. Iyengar for cardiac patients, and during the other 3 sessions, they practiced a placebo relaxation session. The yoga program started with 15 minutes of resting poses, 60 minutes of standing poses, backbends, inverted poses, and ended with 15 minutes of resting poses. (The yoga sequence is listed in the linked article.) The yoga practitioners were matched to a healthy group of volunteers not practicing any relaxation techniques and instead participating in a placebo program. The placebo program included 15 minutes of resting on the floor, 60 minutes walking in a park, followed by another 15 minutes resting on the floor.
Results of the monitoring indicated that heart rate variability was significantly higher during the yoga intervention. The authors conclude that “…relaxation by yoga training is associated with a significant increase of cardiac vagal modulation.” Recommended as an easy-to-apply, no side effects intervention for cardiac rehabilitation programs, it seems that yoga could be beneficial for many patients with different conditions and in various practice settings. The yoga applications can be modified with props and by sequence of yoga postures to account for patient’s level of health. Finding yoga instructors who are capable of adapting yoga to a patient’s specific needs is also important, and if you would like to learn more about yoga applications in rehabilitation, the Institute has several courses that you may find helpful.
Herman & Wallace has several courses available for practitioners who want to start implementing these tools into their practice. Yoga for Pelvic Pain discusses the positive effects of yoga on interstitial cystitis/painful bladder syndrome, vulvar pain, coccydynia, hip pain, and pudendal neuralgia, and it includes the instruction of many poses/techniques. The next opportunity to take this course is next month, September 12-13 in Boston, MA.
An interesting study aimed to objectively answer the following question: Does applying kinesiotape to promote a posterior pelvic tilt improve an active straight leg raise (ASLR) test in women who have sacroiliac joint pain and who habitually wear high-heeled shoes? To explain some of the rationale for the chosen technique and target population, the authors first describe prior research pointing out that use of high heels can lead to an anterior pelvic tilt position and increased lumbar lordosis. This position can slacken the sacrotuberous ligament and therefore reduce the ability of the ligament to create proper form closure, according to the article.
The research included 16 women with a mean age of 23.63. Inclusion criteria is as follows: having a habit of wearing high-heeled shoes (at least 4 times/week for 4 consecutive hours over at least 1 year), and having pain in both sacroiliac joints with the active straight leg raise test (ASLR). Additionally, having symptoms for at least 3 months, no proximal SIJ pain referral to the lumbar spine, and at least 3 of 5 positive SIJ tests (posterior shear test, pelvic torsion test, sacral thrust test, distraction and compression test) were needed for inclusion in the study.
Anterior pelvic tilt was measured using a palpation meter (PALM) before, immediately after application, 1 day after tape application, and immediately after removal of tape. ASLR was measured at same time points. The ASLR was self-scored on a 6-point scale ranging from “not difficult at all”” to unable to perform”. Kinesiotape was applied for a posterior pelvic tilt taping, and the tape was applied in the target position. I-type strips with ~50% of available tension were applied over the rectus abdominis and external oblique muscles. I-type strips with ~75% tension were placed from ASIS to PSIS aiming for mechanical correction of the anterior tilt.
Results of the study indicated a decrease inanterior pelvic tilt, both during and after tape application, and an improved active straight leg raise test. As this was a preliminary study, the results cannot be extrapolated to SIJ pain and dysfunction with other activities than the ASLR test. The degree of anterior pelvic tilt cannot also directly be correlated to sacroiliac joint pain and dysfunction, yet this research is very interesting, and demonstrates a simple method for affecting in the short term a patient’s mechanics as well as reports of function on the ASLR test, a very clinically simple and useful exam.
If you would like to learn more about evaluating and treating dysfunctions related to the sacroiliac joint, join Peter Philip at Sacroiliac Joint Evaluation and Treatment - New Orleans, LA this Sep 12, 2015 - Sep 13, 2015.
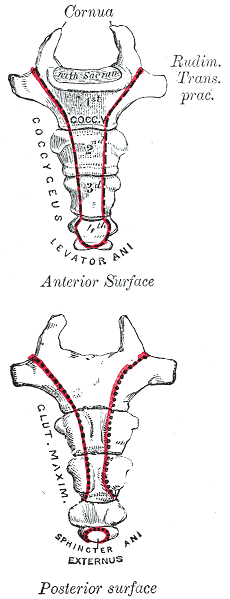
Herman & Wallace faculty member Lila Abbate instructs several courses in pelvic rehabilitation, including "Coccyx Pain, Evaluation and Treatment". Join Lila this October in Bay Shore, NY in order to learn evaluation and treatment skills for patients with coccyx conditions.
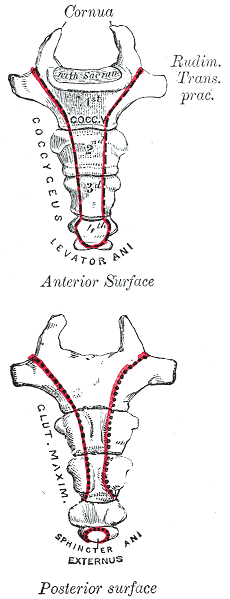
Case studies are relevant reading for physical therapists. Reviewing case studies puts you into the writer’s brain allowing you to synthesize your current knowledge of a particular diagnosis taking you through some atypical twists and turns in treating this particular patient type. In JOSPT, August 2014, Marinko & Pecci presented a very well-written case study of two patients with coccyx pain. By then, I had already written my Coccyx course and couldn’t wait to see what the authors had written. I eagerly downloaded the article to see another’s perspective of coccyx pain and their treatment algorithms, if any, were presented in the article. How were the author’s patients different than mine? What exciting relevant information can I add to my Coccyx course?
I believe that coccyx pain patients have more long-standing pain conditions than other patient types. For the most part, the medical community does not know what to do with this tiny bone that causes all types of havoc in patients’ pain levels. Sometimes treating a traumatic coccydynia patient seems so simple and I am bewildered as to why patients are suffering so long - and other times, their story is so complex that I wonder if I can truly help.
The longer I am a physical therapist, the more important has the initial evaluation become. Our first visit with the patient is time together that really helps me to create a treatment hypothesis. This examination helps me to put together an algorithm for treatment. I now hear their story, repeat back their sequence of events in paraphrase and then I ask: do you think there is any other relevant information, no matter how small or simple, that you think you need to tell me? Some will say, I know it sounds weird, but it all started after I twisted my ankle or hurt my shoulder or something like that. I assure them that we have the whole rest of the visit together and they can chime in with any relevant details. Determining the onset of coccyx pain will help you gauge the level of improvement you can expect to achieve. Coccyx literature states that patients who have coccyx pain for 6 months or greater will have less chance for resolution of their symptoms. However, none of the literature includes true osteopathic physical therapy treatment, so I am very bias and feel that this statement is untrue.
The coccyx course is a very orthopedically-based which takes my love of manual, osteopathic treatment and combines it with the women’s health internal treatment aspects so that we are able to move more quickly to get patient’s back on the path to improved function and recovery. The course looks at patients from a holistic approach from the top of their head down to their feet. In taking on this topic, I couldn’t do it without honing into our basic observation skills, using some of my favorite tools in my toolbox: Hesch Method, Integrated Systems Model, and traditional osteopathic and mobilization approaches mixing it with our internal vaginal and rectal muscle treatment skill set.
Marinko LN, Pecci M. Clinical decision making for the evaluation and management of coccydynia: 2 case reports. J Orthop Sports Phys Ther. 2014 Aug; 44(8): 615-21.
Today we hear from Martina Hauptmann, PT, PMA-CPI, instructor of "Pilates for the Pelvic Floor: Pelvic Floor Dysfunction, Osteoporosis and Peripartum". Join Martina this September 19-20 in Chicago, IL to learn how to incorporate Pilates into your treatment plans!
 Because the cost of staying in business is increasing and the insurance reimbursement rates are dropping, many physical therapy clinics are looking for cash based supplemental services (medically-orientated gym memberships, Pilates classes, yoga classes, durable exercise supplies etc). Offering Pilates as part of the physical therapy clinic’s therapeutic interventions will differentiate your clinic and may be marketed to physicians and the community to increase your clinic’s market share. Post rehabilitation, the offering of cash based Pilates wellness classes can increase the clinic’s bottom line, allowing for further rehabilitation of the client beyond the time frame allowed by insurances and improve retention of clients.
Because the cost of staying in business is increasing and the insurance reimbursement rates are dropping, many physical therapy clinics are looking for cash based supplemental services (medically-orientated gym memberships, Pilates classes, yoga classes, durable exercise supplies etc). Offering Pilates as part of the physical therapy clinic’s therapeutic interventions will differentiate your clinic and may be marketed to physicians and the community to increase your clinic’s market share. Post rehabilitation, the offering of cash based Pilates wellness classes can increase the clinic’s bottom line, allowing for further rehabilitation of the client beyond the time frame allowed by insurances and improve retention of clients.
Pilates is a system and philosophy of exercises based on the work of Joseph Pilates (1883-1967) that focuses on precision and optimal alignment. This approach requires the client to focus her mind on the exercise in order to increase motor control. Women are attracted to the Pilates method because of its gentle but effective nature. Offering Pilates as part of your therapeutic offerings is a great marketing tool to physicians and to the community as well as an effective method for instructing specific muscle re-training.
My course will focus on the application of the Pilates method to women’s health issues: incompetent pelvic floor, hyperactive pelvic floor, chronic pelvic floor pain, pre-natal, post-natal and osteoporosis with small props. The course will utilize equipment that you may have in the clinic already (physio balls, foam rollers, resistance bands, small balls BOSUs and introduction to the Hooked on Pilates MINIMAX and HANDIBANDs).
The course specifically will incorporate Pilates exercises that increase the function of the pelvic floor via the intrinsic and extrinsic synergists of the pelvic floor muscles. Rationale for modified Pilates exercises for clients that exhibit hyperactivity in the pelvic floor muscles (Carriere & Feldt, 2006), pre-natal (ACOG, 2002) and osteoporosis (Sinaki, 1984 and Sinaki, 2002) will be discussed and modified exercises performed. Finally discussion of post-natal issues of lumbo-pelvic pain and pubic symphysis pain will be incorporated and specific exercises for these issues performed (Richardson and Jull, 1995).
This course has a heavy emphasis on exercise. Participants in this course will be able to utilize all instructed exercises immediately following the course. I hope to see you there!
References:
Carriere & Feldt (2006). The Pelvic Floor. Stuttgart, Germany: Georg Thieme Verlag.
American College of Obstetricians and Gynecologists (2002).
Sinaki, Mikkelsen (1984). Post-menopausal spinal osteoporosis: Flexion versus extension exercises. Arch Phys Med Rehab. Vol 65, Oct, 593-596.
Sinaki et al. (2002). Stronger back muscles reduce the incidence of vertebral fractures: A prospective 10 year follow-up of postmenopausal women. Bone. 30(6); 836-841.
Richardson, Jull (1994). Muscle control-pain control. What exercises would you prescribe? Manual Therapy. 1, 2-10.
Isa Herrera, MSPT, CSCS teaches the "Low-Level Laser Therapy for Female Pelvic Pain Conditions" course for Herman & Wallace. Join her on October 3-4 in New York, NY to learn about this new modality!
Physical therapists deal with chronic pain that can be problematic to treat and manage on a daily basis. There is an arsenal of tools, exercises and techniques at their disposal, but many times using a modality can help accelerate the pain-relieving process.
 At my healing center in New York City, we treat an extremely difficult type of chronic pain loosely classified under the umbrella term "pelvic pain". Pelvic pain can express itself as sacroiliac pain, hip bursitis, symphysis pubic dysfunction, and vulvodynia. Chronic pelvic pain is sometimes perceived as a "woman's issue", but we treat both men and women who have suffered for years with their conditions. We are challenged to think outside the box to provide relief for these patients.
At my healing center in New York City, we treat an extremely difficult type of chronic pain loosely classified under the umbrella term "pelvic pain". Pelvic pain can express itself as sacroiliac pain, hip bursitis, symphysis pubic dysfunction, and vulvodynia. Chronic pelvic pain is sometimes perceived as a "woman's issue", but we treat both men and women who have suffered for years with their conditions. We are challenged to think outside the box to provide relief for these patients.
'Secret Weapon' for Pain
Chronic pelvic pain is very different from other types of pain because it's intimately connected to our emotional, spiritual and psychological states, and can involve many symptoms in the nervous, endocrine, visceral, gynecological, urological and muscular systems. It can be very difficult to treat, and can require from six months to one year of physical therapy, depending on patient presentation and history.
This lengthy course of treatment requires a fresh approach to therapy and modalities. When I started treating this population I had many difficulties when it came to controlling their pain and I had to think differently. Electrical stimulation and ultrasound were not working as well as I'd hoped, and were providing insufficient pain relief to these patients.
I needed a modality that, when incorporated with my pelvic pain treatment protocols, could help produce immediate and long-lasting pain-relieving effects. I needed a modality that could significantly decrease pain within one session, and that my patients could believe in because of the results.
Low-level laser therapy (LLLT) proved to be my secret weapon when treating women with chronic pelvic pain. (I frequently call it "light therapy", because many patients are put off by the term "laser.")
I have been successfully using light therapy for nearly ten years. It helps my patients keep their pain at bay, and many request that I use it as part of their therapy. Of course, light therapy is only as good as the therapist using it. You have to apply this modality correctly, and use the science properly to maximize results.
LLLT was approved by the FDA in 2002. At that time, the modality was hailed by the New England Patriots and the U.S. Olympic Committee, among others, for its ability to help top athletes quickly return from injury. Endorsements from these organizations piqued my interest and I decided to research its principles.
I realized that LLLT could be used on many levels. LLLT is unique: it is a cellular bio-stimulator and is used to increase vitality of cells as well as processes that occur within the cell. Not all lasers are "created equal," and you have to be careful with the type you purchase.
Principles that must be taken into consideration include wavelength in nanometers, power in milliwatts, and total energy delivered in joules. In my pelvic pain protocols, I use LLLT on sensitive and painful tissues that are unable to tolerate any heat production.
Many lasers claim to be great therapeutic lasers, but actually produce heat within the tissue and cells. Any heat production has the potential to harm cells and destroy them. Heat production indicates the delivery of too many joules of energy per cycle. The goal with LLLT is to stimulate health and vitality within the cell to produce effects such as pain relief, collagen synthesis, resetting nerve potential, anti-inflammatory effects, and endorphin production.
New Look at Modalities
LLLT has changed the way I treat all pain syndromes. It's had such a positive impact that I've created laser protocols for vulvodynia, scar and bladder pain. I also created a special class for the Herman and Wallace Institute class for physical therapists who treat chronic pelvic pain. I encourage any colleagues specializing in this population to investigate this remarkable modality and to attend the class in October. If you are looking for something different and a modality that will change the way you treat come and learn how to use if effectively.
An article promoting the beneficial role of a thorough clinical assessment was published last year in the Scandinavian Journal of Urology, and although the article is directed to medical providers, serves as an excellent summary for pelvic rehabilitation providers. Doctors Quaghebeur and Wyndaele describe a “four-step plan” that can help direct treatment efficiently, and that emphasizes the muscular and neurologic systems as potential referral sources. While you may not be surprised about several of the steps, you may find this article to be a useful tool, particularly for the terrific chart about neuralgia-type pain that you can find in the linked article.
 Step 1 should include history taking with attention to information about the following:
Step 1 should include history taking with attention to information about the following:
- urinary frequency, urgency, and nocturia
- bowel habits
- sexual complaints and quality-of-life impact
- pain description with significant detail
- use of questionnaires
Step 2 emphasizes review of prior assessments and reports, including:
- imaging (x-rays, MRI, CT)
- lab work
Step 3 involves a thorough clinical assessment. This includes a neurologic assessment of the lumbosacral plexus, with evaluation of motor and sensory functions as well as reflexes. The nerves suggested for testing are the sciatic, iliohypogastric, ilioinguinal, genitofemoral, obturator, lateral cutaneous femoral, perineal and dorsal, and the medial, lateral, and inferior cluneal nerves. (An excellent chart listing each of these nerves and their dynamic tests is included in the article.) Of note in the chart is the lack of neurodynamic tests for the deep peroneal nerve, pudendal, perineal, dorsal nerve of the clitoris or penis, and the interior cluneal- these can be tested for symptom reproduction with direct palpation according to the authors. Other Step 3 tests are listed below.
- neurodynamics tension testing and nerve palpation
- EMG testing if needed
- evaluation for hernia (abdominal, inguinal, or femoral)
- exam of external genitalia (rash, secretion, abscess, fistula, atrophic disorders, signs of trauma, palpation)
- rectal and/or vaginal exam
Step 4 involves an extensive musculoskeletal system examination. This includes the spine, pelvic girdle, muscles, tendons, and pain points.
- spinal mobility (palpation, AROM, PROM)
- joint play of SI joints, pubis and sacrococcygeal joints
- muscular pain or other soft tissue pain reproduction
The physicians recommend a multidisciplinary team of providers including physical therapy. The true value of this article, from a rehabilitation standpoint, may be the emphasis on a thorough musculoskeletal examination as well as attention to recognizing neuralgias. We might utilize an article such as this to dialog with medical providers, or to assess our own “thorough” list of examination techniques. Herman & Wallace offers several courses which can benefit the practitioner seeking to gain new evaluation techniques. "Manual Therapy for the Lumbo-Pelvic-Hip Complex" is a great option which will be available this October 17-18 in beautiful Napa, CA.
Today we get to hear from Mitch Owens, MsPT, COMT who is the author and instructor of "Neck Pain, Headaches, Dizziness, and Vertigo: Integrating Vestibular and Orthopedic Treatment". Join Mitch in Rockville, MD on November 14-15 in order to learn more about treating patients with head trauma.
 Following a whiplash injury, concussion or vestibulopathy patients will complain of the same cluster of symptoms: neck pain, dizziness, and headache. In order to properly treat patients complaining of these symptoms a clinician must first be able to determine the source and understand the physiology at work to reason out the best plan of care.
Following a whiplash injury, concussion or vestibulopathy patients will complain of the same cluster of symptoms: neck pain, dizziness, and headache. In order to properly treat patients complaining of these symptoms a clinician must first be able to determine the source and understand the physiology at work to reason out the best plan of care.
Treating individuals for dizziness, neck pain and headaches requires a refined understanding of the systems involved, the clinical tests that can be used to differentiate symptom generation and then finally which evidence based interventions should be deployed.
A patient who presents with a complaint of dizziness or vertigo following a trauma to the head or neck will challenge the examination skills of even the best practitioners. The list of differential diagnosis includes a number of conditions that could prove to be quite threatening to the patient with or without intervention. These conditions include: vertebral basilar insufficiency, cervical fracture, dislocation or instability, stroke, traumatic brain injury, concussion, and peripheral vestibulopathy to name a few. The ability to clinically reason and properly assess these individuals is crucial to the effective management of any orthopedic or neurologic case load.
Clinicians treating either population need skill sets that bridge the orthopedic and neurologic expertise gap that often exist if clinicians. The need to close this gap is highlighted the following facts:
- 15-20% of Benign Paroxysmal Positional Vertigo is caused by trauma (Gordon, Carlos et al. 2004).
- 19% of cases of whiplash demonstrated vestibulopathy with videonystagmography (VNG) testing within 15 days of their accident (Nacci, A. et al 2011).
- 60% of cases of whiplash with head trauma demonstrated vestibulopathy (Nacci, A. et al. 2011).
- Dizziness is reported 20-58% of whiplash patients (Wrisley DM et al. 2000).
- Between 40%-70% of individuals with persistent whiplash associated disorders complain of dizziness (Treleaven, Julia et al. 2003).
- The incidence of cervicogenic dizziness has been reported to be 7.5% of all dizziness (Ardic FN, et al. 2006)
Recent evidence has shown that sensory dysfunction is as much a part of dizziness as it is a component of chronic neck pain (Treleaven, Julia et al. 2003).
Interventions directed at training cervical proprioception have been show to significantly reduce pain and has improved function in patients with chronic neck pain (Revel, Michel, et al 1994). Manual therapy techniques directed at the upper cervical spine have also been shown to effectively treat dizziness in randomized control trials (Reid, Susan A., et al. 2013).
Thus we are learning the ability to effectively measure and treat neurologic dysfunction is an important part of address cervical spine issues. It is equally true that being able to assess and treat cervical spine dysfunction is an important part of treating patients who complain of dizziness.
Enhancing your neurologic and orthopedic skill set is clearly useful for any clinician and will help improve your outcomes across all patient populations. Continued training in these areas will expand what patients you can see, add to your clinical tool belt, and improve your confidence within your current caseload.
References:
Ardic FN, Topuz B, Kara CO. Impact of multiple etiology on dizziness handicap. Otol Neurotol. 2006;27:676 – 680.
Gordon, Carlos R., et al. "Is posttraumatic benign paroxysmal positional vertigo different from the idiopathic form?." Archives of Neurology 61.10 (2004): 1590-1593.
Nacci, A., et al. "Vestibular and stabilometric findings in whiplash injury and minor head trauma." Acta Otorhinolaryngologica Italica 31.6 (2011): 378.
Reid, Susan A., et al. "Comparison of Mulligan Sustained Natural Apophyseal Glides and Maitland Mobilizations for Treatment of Cervicogenic Dizziness: A Randomized Controlled Trial." Physical therapy (2013).
Revel, Michel, et al. "Changes in cervicocephalic kinesthesia after a proprioceptive rehabilitation program in patients with neck pain: a randomized controlled study." Archives of physical medicine and rehabilitation 75.8 (1994): 895-899.
Treleaven, Julia, Gwendolen Jull, and Michele Sterling. "Dizziness and unsteadiness following whiplash injury: characteristic features and relationship with cervical joint position error." Journal of Rehabilitation Medicine 35.1 (2003): 36-43.
Wrisley DM, Sparto PJ, Whitney SL, Furman JM: Cervicogenic dizziness: a review of diagnosis and treatment. Journal of Orthopaedic & Sports Physical Therapy 2000, 30(12):755-766.
What are the attributes and barriers to care for college-aged women who have pelvic pain? This is a question asked by researchers who published an original article on the topic in the Journal of Minimally Invasive Gynecology. To complete the study, a random sample of 2000 female students at the University of Florida were sent an online questionnaire. Included in the questionnaire was basic demographic data, general health and health behavior questions, psychosocial factors, measures assessing different types of pelvic pain such as dyspareunia, dysmenorrhea, urinary, bowel, or vulvar pain, and information about barriers to care for pelvic pain and quality of life measures. A total of 390 women completed the survey, and the mean age was 23 years old. Most of the women in the sample identified as white, with 9.6% identifying as black or African-American. Most of the respondents had never been pregnant. The chart below lists some of the data.

| Experienced pelvic pain over past 12 months | 73% |
| Dysmenorrhea | 80% |
| Deep dyspareunia | 30% |
| Symptoms with bowel movements | 38% |
| Vulvar pain (including superficial dyspareunia) | 21.5% |
| Of women with pelvic pain, those lacking diagnosis | 79% |
| Of women with pelvic pain, those who have not visited doctor | 74% |
Barriers to receiving care included difficulty with insurance coverage and providers’ “…lack of time and knowledge or interest in chronic pelvic pain conditions.” An interesting finding was that among the women who had pelvic pain, those who were sexually active reported lower scores on physical and mental health. Even among the women without pelvic pain, those who were sexually active reported lower mental health scores.
How can this study encourage us as pelvic rehabilitation providers? Can we reach out to providers and share the potential benefits of pelvic rehab care to decrease the burden on the patient in finding services? It seems that in addition to continually spreading the word that pelvic pain can be eased with rehabilitation efforts, we can provide the interest and knowledge in the subject so that the patient can feel validated and can be instructed in self-management tools.