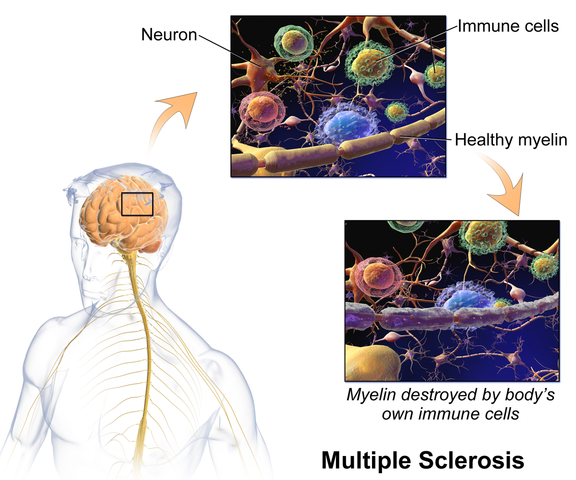
The following is part three in a series documenting Deb Gulbrandson, PT, DPT's journey treating a 72 year old patient who has been living with multiple sclerosis (MS) since age 18. Catch up with Part One and Part Two of the patient case study on the Pelvic Rehab Report. Dr. Gulbrandson is a certified Osteoporosis Exercise Specialist and instructor of the Meeks Method, and she helps teach The Meeks Method for Osteoporosis course.
 On Maryanne’s third visit, after reviewing her home exercises I told her that today our focus was on alignment. “In dealing with osteoporosis we want the forces that act upon our bodies to line up as optimally as possible. We have gravity providing a downward force from above and we have ground reaction forces coming up from below. Remember back to your first visit when we did the Foot Press in sitting and talked about Newton’s 3rd Law? For every action there’s an opposite and equal reaction and, how by pressing your feet down it helped you to sit straighter and gave more support to your back?” She nodded in agreement.
On Maryanne’s third visit, after reviewing her home exercises I told her that today our focus was on alignment. “In dealing with osteoporosis we want the forces that act upon our bodies to line up as optimally as possible. We have gravity providing a downward force from above and we have ground reaction forces coming up from below. Remember back to your first visit when we did the Foot Press in sitting and talked about Newton’s 3rd Law? For every action there’s an opposite and equal reaction and, how by pressing your feet down it helped you to sit straighter and gave more support to your back?” She nodded in agreement.
“Well, there’s another important component to that- one that we call optimal alignment. When we sit or stand in a flexed posture, those two opposing forces do not line up well and can put undue stress and pressure on our body, particularly the vertebral bodies.” I showed her the spine again with an increased flexion (hyper-kyphosis) in the thoracic area. “It’s normal to have a kyphosis in the thoracic spine. What we don’t want is a hyper-kyphosis. We often see the apex of the increased curve around T-7, 8, 9 levels near the bra line. We also call it the “slouch line” because from the front, that’s where we slouch in sitting. A thoracic hyper-kyphosis can lead to hyper-lordosis in the lumbar spine as the body tries to counteract the flexion forces above with extension or arching in the low back. We know that Wolff’s Law states that bone in a healthy person will adapt to the loads under which it is placed.1 But we want those loads to be optimally transmitted; otherwise the adaptation can be problematic.”
With Maryanne sitting in a Perch Posture position on the side of the low mat table, I placed a 4 foot dowel rod alongside her back, touching her sacrum and apex of her thoracic curve. I instructed her to bring her occiput back toward the dowel without extending her neck. I wanted her to do more of a cervical retraction move. She was a good 3+ inches away. Previously I had measured her using the WOD (Wall to Occiput Distance).2 This helps patients understand when they are forward flexed in the upper thoracic and cervical area and becomes an exercise as well. Since Maryanne was not safe in a standing position, we used an armless chair against the wall. I turned it sideways so the side of the chair was snugged up to the wall and transferred her to the chair, sitting so that her sacrum was flush against the wall. “Bring your upper back against the wall without allowing your low back to arch forward”, I told her as I placed a folded towel behind her head. “Now you’re going to press the back of your head into the towel, just as you do when lying down in the Re-alignment routine. Before you perform the Head Press, inhale to prepare, start your exhale, then do the head press. Hold for 3 -5 seconds as you continue to exhale, then relax as you inhale. Do 3-5 reps.”
The Head Press in standing, (or in Maryanne’s case, sitting) is a convenient way to not only strengthen the back muscles isometrically, but also increase awareness of body in space and relationship of head to trunk positioning. For any individual who has developed a forward head position over a period of years, there is a loss of the proprioceptive feedback necessary to know when we’re not in alignment, even if we have the ROM to achieve it. And often a lack of strength and especially muscle endurance to maintain that optimally aligned position is problematic. Using the wall several times a day can assist in building strength and awareness. In Maryanne’s case we needed a folded towel behind her occiput to give her something to press into and prevented her from going into increased cervical extension.
“I still want you to do the Head Press in supine as part of the Re-alignment routine everyday”, I told her. “But also practice it in sitting against a wall, making sure your sacrum is right up against it. Do this several times a day for several minutes, holding 3-5 seconds each. And be sure to use your breath to maintain neutral alignment of your lumbar spine.”
And with that, our work for the day was done.
1. Wolff's Law and bone's structural adaptations to mechanical usage: an ... https://www.ncbi.nlm.nih.gov/pubmed/8060014
2. Concurrent Validity of Occiput-Wall Distance to Measure Kyphosis in Communities. Journal of Clinical Trials. May 18, 2012 Sawitree Wongsa1,4, Pipatana Amatachaya2,4, Jeamjit Saengsuwan3,4 and Sugalya Amatachaya1,4*
The following is part two in a series documenting Deb Gulbrandson, PT, DPT's journey treating a 72 year old patient who has been living with multiple sclerosis (MS) since age 18. Catch up with Part one of the patient case study on the Pelvic Rehab Report here. Dr. Gulbrandson is a certified Osteoporosis Exercise Specialist and instructor of the Meeks Method, and she helps teach The Meeks Method for Osteoporosis course.
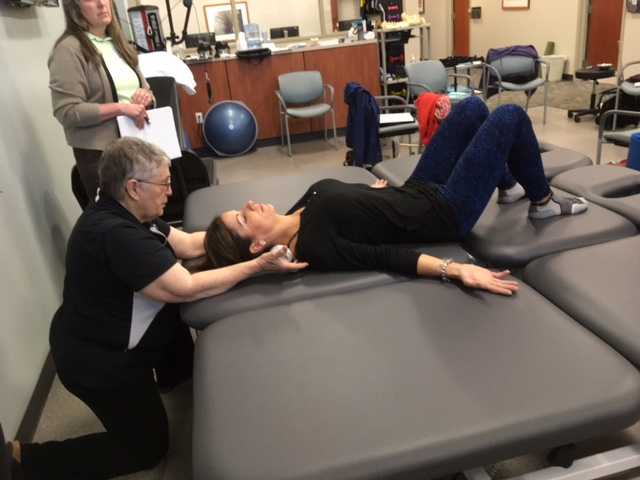
On Maryanne’s second visit, she reported she had been doing her “homework” and didn’t have any questions. Just to be sure, we reviewed them and I had her demonstrate. In Decompression position, she was lying supine with her hands on her abdomen, a common mistake I see. Usually this is due to tightness in pec minor with protracted scapulae. Patients unknowingly resort to the path of least resistance to take the strain off of the muscles. I explained to her that we want to use gravity to gently lengthen those muscles and “widen” the collarbones to allow for improved alignment. With her shoulders abducted to approximately 30 degrees and palms up, I propped a couple of small towels under her forearms which allowed her shoulders to relax into a more posterior and correct position.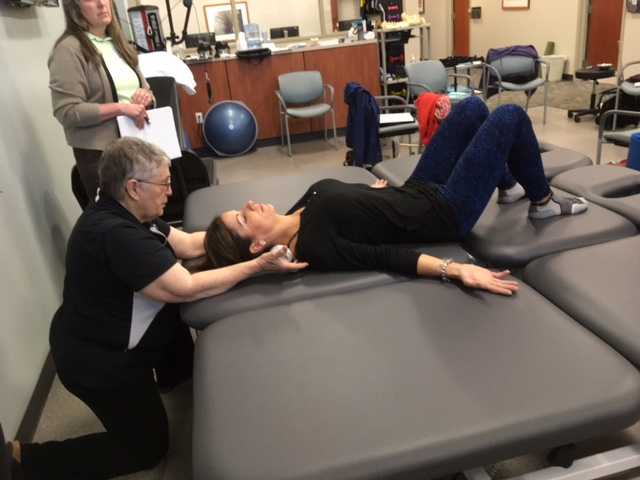
“Today we begin the Re-alignment routine,” I said, “starting with the Shoulder Press.” I showed her how to gently press the back of her shoulders down into the mat without arching her lumbar spine. “As you press your shoulders down, exhale through your mouth as if you’re fogging a mirror. This will help activate your core muscles to keep your back in good alignment. Hold for 2-3 seconds, and then relax. Repeat 3 times.” Maryanne looked at me as if I’d lost my mind. “Did you say do 3 reps?” she asked. “I do 2 sets of 20 reps at the gym,” she said with obvious pride in her voice. “Yes, that’s where we start, and there are a couple of reasons. First, these are very site specific exercises which focus on the exact areas that need strengthening. Exercises done in a gym setting are often more general and usually involve compensation. We are minimizing any compensation such as allowing your low back to arch. There is probably weakness in those upper back muscles as well as the tightness seen in your anterior chest muscles and we need to go slowly. Also, we are simultaneously stretching while we strengthen. Our society is so forward biased (we work on computers, drive cars, make beds, eat- it’s all forward, forward, forward), that the anterior muscles get tight and the upper back muscles get overstretched and weak. We need to reverse that pattern. Take a look at our younger population and their texting postures. Yikes! We will be layering on more exercises as your technique improves so you’ll be doing more than just 3 reps, I promise.”
After the Shoulder Press we proceeded with the Head Press, Leg Lengthener and Arm Lengthener, spending time to make sure her cervical spine stayed in neutral as she pressed her head down into the mat. Head Press (cervical retraction) performed in supine allow patients to have something to press against and helps inhibit the tendency to move into cervical extension. It can also be done standing against the wall with a small pillow or folded towels between the occiput and the wall.
We ended with Maryanne in standing at the kitchen sink to promote functional activities and weight bearing positions. I reminded her to do the Foot Press through the floor using the Triangle of Foot Support visual. This helped to elongate her spine. “Imagine a bungie cord running from the top back of your head to the ceiling” I said which further increased her standing height. “Now I want you to imagine a shelf running straight out from your breastbone with a glass of some very expensive fine drink sitting on it. Do not spill your libation! Oh, and one last thing Maryanne. Breathe!!!” At which point she collapsed into laughter and our session was over. “Busted”, she said.
The following case study comes from faculty member Deb Gulbrandson, PT, DPT, a certified Osteoporosis Exercise Specialist and instructor of the Meeks Method. Join Dr. Gulbrandson in The Meeks Method for Osteoporosis on September 22-23, 2018 in Detroit, MI!
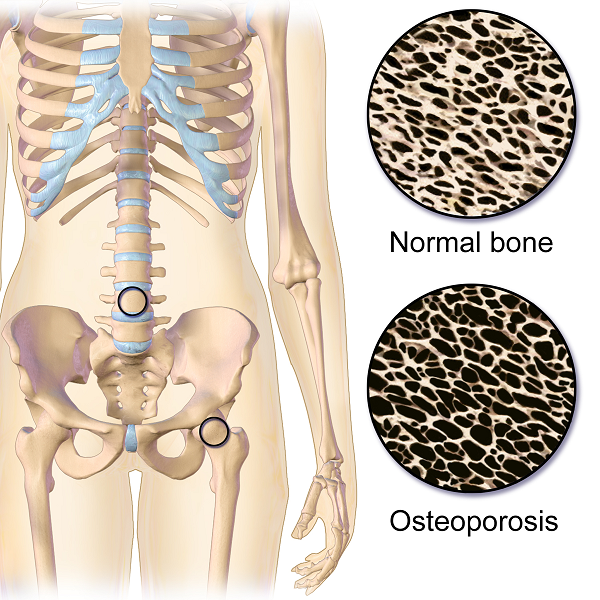
The first sight I had of my new patient was watching her being wheeled across the parking lot by her husband. A petite 72-year-old, I could see her slouched posture in the wheelchair. With the double diagnosis of osteoporosis and Multiple Sclerosis (MS) it didn’t look good. However, “Maryanne“ greeted me with a wide grin and a friendly, “I’m so excited to be here. I’ve heard good things about this program and can’t wait to get started.“
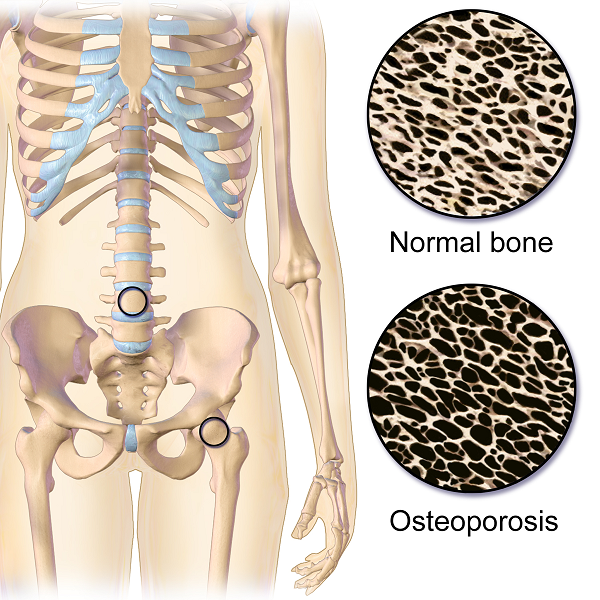 That’s what I find with my osteoporosis patients. They are highly motivated and willing to do the work to decrease their risk of a fracture. Maryanne was unusual in that she was diagnosed with MS at a very young age. She was 18 and had lived with the disease in a positive manner. She exercised 3X a week and had a caring, involved husband. They worked out at a local health club, taking advantage of the Silver Sneakers program. Maryanne was able to stand holding onto the kitchen counter but had stopped walking five years ago due to numerous falls. She performed standing transfers with her husband providing moderate to max assist. Her osteoporosis certainly put her at a high risk for fracture.
That’s what I find with my osteoporosis patients. They are highly motivated and willing to do the work to decrease their risk of a fracture. Maryanne was unusual in that she was diagnosed with MS at a very young age. She was 18 and had lived with the disease in a positive manner. She exercised 3X a week and had a caring, involved husband. They worked out at a local health club, taking advantage of the Silver Sneakers program. Maryanne was able to stand holding onto the kitchen counter but had stopped walking five years ago due to numerous falls. She performed standing transfers with her husband providing moderate to max assist. Her osteoporosis certainly put her at a high risk for fracture.
Even though she had been exercising on a regular basis, she was unfortunately doing many of the wrong exercises. Her workout consisted of sit-ups and crunches. She used the Pec Deck bringing her into scapular protraction and facilitating forward flexion. She was also stretching her hamstrings by long sitting reaching to touch her toes.
Spinal flexion is contraindicated in patients with osteoporosis. A landmark study done in 19841 divided a group of women with osteoporosis into 4 groups. One group performed extension based exercises, a second group did flexion. A third group used a combination of flexion and extension and the fourth was the control and did no exercises. Below are the results 1-6 years later.
- Extension Group: 16% incidence of fracture or wedging of vertebral bodies
- Flexion Group: 89% rate.
- Combination Extension/Flexion: 53% rate
- No Exercise Group: 67%
The results were astounding. Granted, it was a small study- 59 participants and it was done a long time ago. But this is a one study that no one wants to repeat, or volunteer for!
Several take home messages followed this study.
- Flexion is contra-indicated for individuals with osteoporosis.
- It’s better to do no exercise than the wrong exercise. The No Exercise group faired better than the Flexion group although at 67% it’s clear that many of our everyday activities- making beds, placing items on low shelves, and now computing and texting put us at risk.
Sadly, many individuals with osteoporosis are told by their physicians to start exercising.......but without any guidance they do what Maryanne did. Just start exercising. And putting themselves at greater risk.
Maryanne was also doing nothing to strengthen her back extensors and scapular area. After giving an overview of the vertebral bodies, pelvis, and hip joint with my trusty spine, I showed both my patient and her husband how forward flexion puts increased compression on the anterior aspect of the spine, particularly in the thoracic curve at T 7, 8, 9, the most common site of compression fractures. We started with Decompression, which is the beginning position for the Meeks method. Many therapists know this as hooklying. This position allows the spinous processes to press against the hard surface of the floor, opening up the anterior portion of the spine and providing tensile forces throughout the length of the spine. With the help of her husband, Maryanne could get down on the floor but I often advise patients who are unable to safely transfer to the floor to lay across the end of their bed. This is less cushy than lying longways where they sleep. Adding a yoga mat or a quilt on top to give more firmness improves the effect.
Supine is the least compressive of all positions; sitting is the most compressive. While Decompression may not seem like much of an exercise it is vital to reduce the effects of gravity and compression on the spine.
We addressed sitting posture by firming up the base of her wheelchair as well as recommending transferring into other chairs and positions frequently throughout the day. Spending time sitting towards the edge of a firm chair in what we call Perch Posture and practicing Foot Presses into the floor created improved alignment in her spine as well as isometrically activating glutes, abs, quads. Using the Foot Press is an example of Newtons 3rd Law, “For every action there’s an equal and opposite reaction” so by pressing her feet down she actually lengthened her torso and head. We also discussed discontinuing the contraindicated exercises in her workout routine and I assured her that the Meeks method would progressively challenge her core (the reason everyone thinks they should do sit-ups) and target the right muscles to help strengthen her bones. We use site specific exercises to target certain muscles that pull on the bone and increase bone strength.2
With instructions to Decompress several times daily to reduce compression on the spine along with the other adjustments made, I felt Maryanne was on her way to reducing her risk of fracture and increasing the quality of her life. She thanked me profusely for the education and the exercise of that session. We both look forward to the next one.
1. Sinaki M, Mikkelsen BA. Postmenopausal spinal osteoporosis: flexion versus extension exercises. Arch Phys Med Rehabil. 1984 Oct;65(10):593-6.
2. Frost HM1. Wolff's Law and bone's structural adaptations to mechanical usage: an overview for clinicians. Angle Orthod. 1994;64(3):175-88.
The British author, John Donne, wrote, “No man is an island, entire of itself; every man is a piece of the continent.” In a similar idea, no neurological symptom is independent and isolated; every system has potential to impact the whole body. Neurogenic bladder should cue a clinician to check for neurogenic bowel and to assess the pelvic floor in order to get a complete map of what to address in treatment.
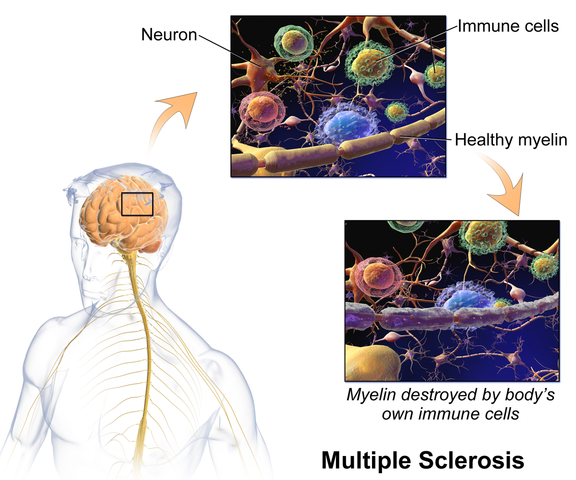 Martinez, Neshatian, & Khavari (2016) reviewed literature on neurogenic bowel dysfunction (NBD) and neurogenic bladder in patients with neurological conditions such as multiple sclerosis (MS). Constipation and fecal incontinence can coexist with NBD, and a multifactorial bowel regimen is vital to conservative management in patients with neurological disorders. Nonpharmacological, pharmacological, and surgical approaches were reviewed in the article. Specific results for MS were reported only for transanal irrigation (TAI) and biofeedback. In TAI, fluid is used to stimulate the bowel and clean out stool from the rectum. A study showed 53% of the 30 patients with MS demonstrated a 50% or better improvement in bowel symptoms with TAI. In anorectal biofeedback, operant conditioning retrains motor and sensory responses via exercises guided by manometry. With biofeedback, a study showed 38% of patients had a beneficial impact with the intervention. The list of treatment approaches not specifically researched for MS patients in this review includes: dietary modifications, perianal/anorectal stimulation, abdominal massage, suppositories, oral medications such as stool softeners or prokinetic agents, sacral neuromodulation, antegrade continence enema, and colostomy.
Martinez, Neshatian, & Khavari (2016) reviewed literature on neurogenic bowel dysfunction (NBD) and neurogenic bladder in patients with neurological conditions such as multiple sclerosis (MS). Constipation and fecal incontinence can coexist with NBD, and a multifactorial bowel regimen is vital to conservative management in patients with neurological disorders. Nonpharmacological, pharmacological, and surgical approaches were reviewed in the article. Specific results for MS were reported only for transanal irrigation (TAI) and biofeedback. In TAI, fluid is used to stimulate the bowel and clean out stool from the rectum. A study showed 53% of the 30 patients with MS demonstrated a 50% or better improvement in bowel symptoms with TAI. In anorectal biofeedback, operant conditioning retrains motor and sensory responses via exercises guided by manometry. With biofeedback, a study showed 38% of patients had a beneficial impact with the intervention. The list of treatment approaches not specifically researched for MS patients in this review includes: dietary modifications, perianal/anorectal stimulation, abdominal massage, suppositories, oral medications such as stool softeners or prokinetic agents, sacral neuromodulation, antegrade continence enema, and colostomy.
Miletta, Bogliatto, & Bacchio (2017) presented a case study about management of sexual dysfunction, perineal pain, and elimination dysfunction in a 40 year old female with multiple sclerosis. She had been experiencing perineal pain for 5 months and had chronic MS symptoms of lower anourogenital dysfunction, including bladder retention and obstructed defecation syndrome. Physical therapy treatment included pelvic floor muscle training (primarily decreasing overactivity of pelvic muscles in this case), perineal massage, biofeedback, postural correction, global relaxation techniques, and a home self-training program. After 5 months of physical therapy, the woman had improved pelvic floor muscle contraction strength, resolution of pelvic floor muscle overactivity, increased sexual satisfaction (according to the Female Sexual Function Index score), a visual analog scale improvement of vulvar and perineal pain by 4 points, normalization of obstructed defecation syndrome, and decreased bladder retention symptoms. The authors concluded the variety of symptoms in MS require a multimodal approach for treatment, considering all the motor, autonomic, and cognitive impairments as well as side effects of medications that try to improve those symptoms. The quality of life of women with MS has potential to be improved significantly if pelvic floor disorders related to MS are addressed appropriately.
Ultimately, treating urinary dysfunction but avoiding bowel dysfunction does neurological patients a disservice. Systems are intertwined in a series of cause and effects throughout the body. The “Neurologic Conditions and the Pelvic Floor” course can expand your knowledge and understanding of how the symptoms of conditions such as multiple sclerosis can impact pelvic health and how we can better address the whole patient for optimal outcomes.
Martinez, L., Neshatian, L., & Khavari, R. (2016). Neurogenic Bowel Dysfunction in Patients with Neurogenic Bladder. Current Bladder Dysfunction Reports, 11(4), 334–340. http://doi.org/10.1007/s11884-016-0390-3
Miletta, M., Bogliatto, F., & Bacchio, L. (2017). Multidisciplinary Management of Sexual Dysfunction, Perineal Pain, and Elimination Dysfunction in a Woman with Multiple Sclerosis. International Journal of MS Care, 19(1), 25–28. http://doi.org/10.7224/1537-2073.2015-082